ORIGINAL ARTICLE
OLIVEIRA, Ronan Djavier Alves [1], ESPÓSITO, Mario Pinheiro [2], PLACHESKI, Ana Carolina Galindo [3], PASSOS, Fabio Manoel dos [4], ANDRAOS, Lorhana Botelho [5]
OLIVEIRA, Ronan Djavier Alves. Et al. PFAPA Syndrome – Periodic Fever, Aphthous Stomatitis, Pharyngitis and Adenitis. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year 05, Ed. 10, Vol. 13, pp. 121-129. October 2020. ISSN: 2448-0959, Access link: https://www.nucleodoconhecimento.com.br/health/pfapa-syndrome
ABSTRACT
Periodic fever, aphthous stomatitis, pharyngitis and adenitis syndrome (PFAPA) is a chronic and benign disease characterized by recurrent episodes of high and periodic fever, aphthous stomatitis, pharyngitis and cervical adenitis, often found in children under five years of age. The etiopathogenesis is unknown and the diagnosis is clinical and exclusionary. The objective of our study is to report the clinical case of a patient with PFAPA syndrome, as well as the diagnostic criteria and treatments of choice performed at Hospital Otorrino de Cuiabá – MT. A 25-year-old female patient with sporadic episodes of high fever and long-standing odynophagia. Hypertrophic palatine tonsils, grade II with crypts, in addition to hyperemic and painful spots on the lower lip. Signs of laryngeal pharyngeal reflux on videolaryngoscopy. In the treatment, the use of clindamycin according to antibiogram and prednisolone was proposed, in addition to scheduled tonsillectomy. After analyzing the literature, it is clear the importance of the correct diagnosis of the syndrome and how it should be considered early, even in children who do not meet all the clinical criteria. Contrary to the prevailing literature, in our study we observed a patient in adulthood with persistence of the clinical picture, without complete remission of symptoms. Although good results were obtained with symptomatic therapy. The most effective medical treatment is corticosteroid therapy, which, however, does not prevent recurrences. In the long term, tonsillectomy surgery is considered an option.
Keywords: Recurrent Fever, Pharyngitis, Aphthous Stomatitis.
INTRODUCTION
PFAPA – (Periodic Fever, Aphtous Stomatitis, Pharyngitis and Cervical Adenitis), translated as Periodic Fever, Oral Aphthas, Pharyngitis and Cervical Adenitis. PFAPA is the autoinflammatory syndrome belonging to the most common group of recurrent febrile syndromes in childhood, although its exact prevalence is not known and it was only identified as a clinical condition in 1987.
It is a rare, non-genetic, chronic disease, symptomatic before the age of five years and, in most patients, the condition resolves spontaneously before the age of 10-12 years. However, it can be prolonged or started in the patient’s adult life.
The prevalence varies throughout the world, and there are no statistical data on the disease in Brazil. It is an important differential diagnosis with many infections in preschool age children, and sure, every doctor will encounter some cases of PFAPA during their career.
CASE REPORT
A 25-year-old female patient comes to the office in June 2018 complaining of odynophagia for 6 days, dry cough, sporadic episodes of unmeasured fever and use of nimesulide since the onset of symptoms, without improvement. On physical examination: oroscopy with grade 2 palatine tonsils, hypertrophic crypts with purulent secretion and oropharyngeal hyperemia. In addition to hyperemic and painful spots on the lower lip, suggestive of stomatitis. Videolaryngoscopy was performed, which showed signs of laryngeal pharyngeal reflux and chronic tonsillitis. In September and October 2018, he returned to the office with the same complaints of odynophagia without improvement, fever spikes, oral aphthae and symptoms of dyspepsia and regurgitation, which reinforce the hypothesis of gastroesophageal reflux. In March 2019, the patient returned due to recurrent tonsillitis, stomatitis, worsening of long-standing oral aphthae, fever associated with arthralgia, myalgia and headache. On physical examination: oropharynx with grade 2 palatine tonsils, with crypts, hypertrophic and aphthoid lesions in the tonsil, palatine and lingual tonsils. Oropharyngeal culture and antibiogram were requested. Culture result: Staphylococcus aureus and colony count 106 CFU. On antibiogram, minimum inhibitory concentration lower than 0.5 for Ceftarolin, Ciprofloxacin, Clindamycin, Oxacillin, Penicillin G, Trimethoprim-Sulfamethoxazole and Vancomycin. The treatment of choice was clindamycin and prednisolone, progressing with significant clinical improvement, without complete remission of symptoms.
DISCUSSION
Periodic fevers with aphthous stomatitis, pharyngitis and adenitis syndrome (PFAPA) is a self-limiting fever syndrome that typically manifests among children 2 to 5 years of age. However, currently, it is known that it can affect older children and, exceptionally, adults. In northern Italy, like the Bueno scholars; Paiva and Carvalho (2019) analyzed, the incidence was approximately 0.4 cases/1000 children/year. Furthermore, the study did not observe a predilection for ethnic groups, however, it was considered that there was a slight predominance for males.
Fonseca and Cherubini (2015) understood that each febrile episode, of undetermined origin, lasts approximately three to six days and, with regard to periodicity, the different published works establish a variation of three to eight weeks (average of 28 days). High fever (39-40.5°C) does not respond to antipyretics and anti-inflammatories. Exudative and erythematous pharyngitis is present in up to 90% of patients, followed by cervical lymphadenopathy in up to 75% and oral aphthae in up to 50%. As for aphthous stomatitis, the lesions are predominantly located in the anterior region of the oral cavity, are smaller than 3 mm, in small amounts and spare the gums. These features allow us to exclude other conditions that present with canker sores, such as herpangina and herpetic gingivostomatitis. Other less frequent symptoms are headache, malaise, chills, myalgia, arthralgia, abdominal pain, nausea and vomiting. Patients are healthy between attacks, with no association with other diseases or impairment in child development.
The Vanoni researchers; Theodoropoulou and Hofer (2016) understood that in adults, it is common for the syndrome to manifest in childhood, with resolution and return in adulthood around the second decade of life, with the diagnosis usually occurring in the third decade. Comparing adults and children with PFAPA syndrome, it is possible to note that there is a lower frequency of arthralgias and myalgias, and greater aphthous lesions and manifestations associated with febrile episodes when associated with the latter group.
Moreira (2012), in his research, understands that the etiology and pathophysiology of PFAPA are still unknown, and there is still doubt about whether it is an infectious disease or immunological dysfunction. Although the genetic causes have not yet been determined, this syndrome tends to be grouped with the syndromes of hereditary fevers. The presence of more than one case in the family suggests polygenic origin or complex inheritance. The hypothesis of an abnormal response of innate immunity, with an increase in interleukin (IL)-1 beta, as occurs in many monogenic autoinflammatory diseases, is the pathogenesis most supported by current studies. The infectious agent in the etiology of PFAPA is unknown, but environmental factors may be associated with immunological factors, contributing to the disease in a genetically susceptible individual.
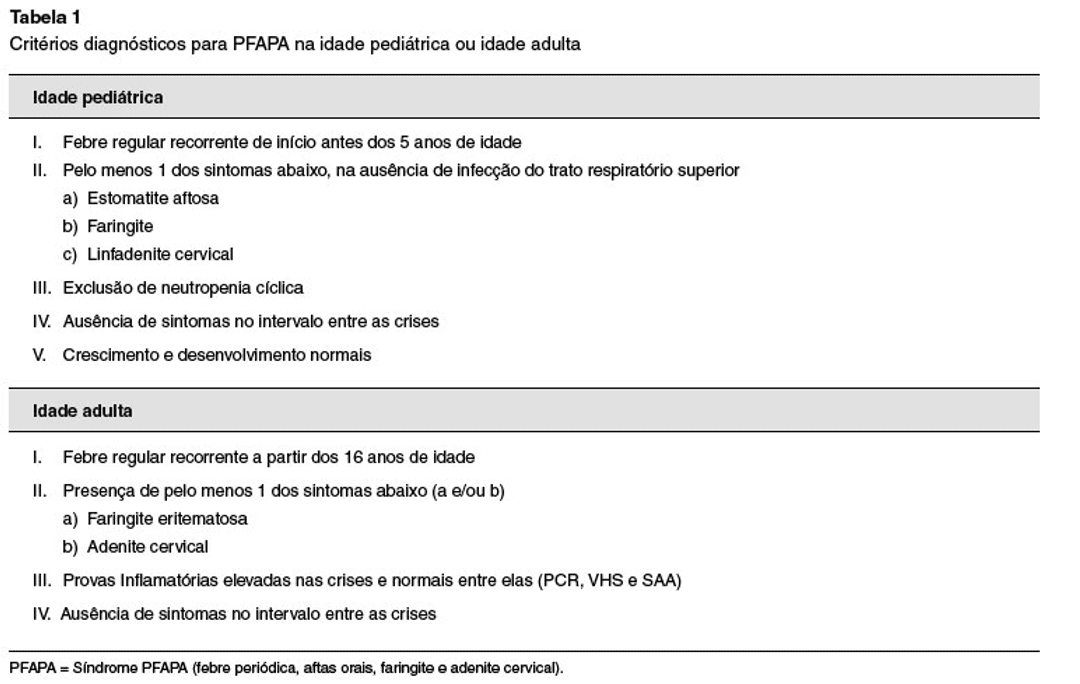
The most used diagnostic criterion for PFAPA is the Thomas criterion (Table 1), established in a cohort of 94 patients with PFAPA in 1999, which is a modification of the 1987 Marshall criterion, when the disease was described.
FIGURE 1: TABLE
Sampaio and Marques (2011) understand that laboratory findings are nonspecific. During febrile outbreaks, there is usually moderate leukocytosis with a predominance of neutrophils, monocytosis, increased erythrocyte sedimentation rate and C-reactive protein (acute phase reactants), with normalization of these markers in the intervals between attacks. Serology for cytomegalovirus, herpes, and Epstein-Barr virus in at least one episode is important. Neutropenia and other symptoms such as diarrhea, rash and cough do not appear to be present, suggesting the need to rule out another disease.
FIGURE 2 – OROPHARYNX

Sampaio and Marques (2011) also state that PFAPA has an important differential diagnosis from other infections in preschool-age children. Febrile illnesses with similar symptoms, especially viral and bacterial pharyngotonsillitis, should be excluded by identifying signs of upper respiratory tract infection or positive oropharyngeal cultures. Patients with hereditary febrile syndromes may fulfill the diagnostic criteria for PFAPA, which is also an autoinflammatory disease, but is not associated with the genetic mutation. Therefore, some patients should be selected and investigated clinically or genetically for other periodic fever syndromes. The main diagnosis to be excluded is cyclic neutropenia, as patients present with fever, pharyngitis, stomatitis and other bacterial infections depending on the severity of the neutropenia, which usually lasts from 3 to 10 days and is repeated at intervals of approximately 21 days.
The therapeutic and prognostic approach is still controversial, but it aims at remission of febrile episodes and improvement in quality of life. Although it does not require specific treatment, glucocorticoids are highly effective in controlling attacks. A single dose of prednisone (1–2 mg/kg) or betamethasone (0.1–0.2 mg/kg) early in the episode reduces fever in less than six hours, as well as most associated symptoms within 48 hours, except aphthous stomatitis (slower onset to respond). If one dose is not effective, a second dose can be given the next day (0.5–1 mg/kg). In adults, prednisone at a dose of 60mg/day administered early, dramatically improved the symptomatic picture.
However, the usefulness of steroids is questioned. Due to recurrence, on-demand use of corticosteroids appears to have the same immunosuppressive effect as chronic use. The asymptomatic interval between episodes can be reduced by 25% to 50% of cases. In addition, administration of corticosteroids does not prevent future outbreaks of fever. Corticosteroid response can be used as a therapeutic test, distinguishing febrile episodes of PFAPA from those seen in other febrile autoinflammatory diseases that generally do not manifest this type of response.
For patients not responding to corticosteroid therapy, an alternative is cimetidine, which seems to increase the synthesis of interferon, in addition to modulating the release of cytokines and chemotactic factor from leukocytes involved in the PFAPA syndrome. Colchicine may be an interesting option for patients with frequent episodes. Its prophylactic use is based on the clinical and laboratory similarities between PFAPA syndrome and familial Mediterranean fever, in addition to the experience in treating the latter with colchicine. (BUENO; PAIVA and CARVALHO, 2019)
Many patients with PFAPA syndrome have low serum levels of vitamin D. Some authors have used vitamin D replacement as a form of treatment, achieving a significant reduction in the number of febrile episodes. However, it is still not possible to state that vitamin D is effective, as studies of large cohorts of patients are lacking.
Recently, Vanoni; Theodoropoulou and Hofer (2016) understood that the numerous studies showed the effectiveness of tonsillectomy in patients with PFAPA, especially in cases of high recurrence and with a short time interval between crises, in addition to cases with contraindication or refractory to clinical treatment. Surgery, in most patients, eliminates recurrent febrile seizures, and is currently considered definitive therapy for PFAPA.
In contrast, the prevalence of the disease, in our study, we observed an adult female patient, with persistence of the clinical picture. We obtained good results with symptomatic therapy, without complete remission of symptoms, and tonsillectomy surgery was proposed.
FINAL CONSIDERATIONS
There is no denying that this is an infrequent pathology whose recognition can be difficult. Therefore, in literary analysis, it is extremely important to give the correct diagnosis of the syndrome, even in children who do not meet all the clinical criteria, eliminating possible differential diagnoses.
Once confirmed, the professional should reassure and guide the family members, clarifying them about the decrease in the recurrence of the conditions with advancing age.
On the other hand, in our study, a 25-year-old female patient was observed, without complete remission of symptoms despite a conservative therapeutic approach. The primary medical treatment of choice is corticosteroid therapy, which, however, does not prevent future recurrences. The tonsillectomy surgery has obtained satisfactory results, and the removal of the palatine tonsils is considered curative, and it is necessary to maintain postoperative follow-up to confirm the remission of the disease.
BIBLIOGRAPHIC REFERENCES
BUENO, Laniel Aparecido; PAIVA, Débora Magalhães; CARVALHO, Paulo Henrique Pimenta. Síndrome PFAPA: Diagnóstico e Tratamento na Atenção Primária à Saúde. Revista Brasileira de Medicina, Família e Comunidade, Minas Gerais, 2019. Disponível em: < https://www.rbmfc.org.br/rbmfc/article/view/1815> Acesso em: 08 de out. de 2020.
FONSECA, Alisson; CHERUBINI, Karen. Aspectos de interesse clínico sobre a síndrome PFAPA (febre periódica, estomatite aftosa, faringite e adenite). Scientia Médica, Porto Alegre, 2005. Disponível em: < https://revistaseletronicas.pucrs.br/ojs/index.php/scientiamedica/article/view/1546/0> Acesso em: 08 de out. de 2020.
MAGALHÃES, Claudia Saad. Diretrizes de conduta e tratamento de síndromes febris periódicas: síndrome de febre periódica, estomatite aftosa, faringite e adenite. Revista Brasileira de Reumatologia, São Paulo, 2016. Disponível em: < https://www.scielo.br/pdf/rbr/v56n1/0482-5004-rbr-56-01-0052.pdf> Acesso em: 08 de out. de 2020.
MENDONÇA, Leandro Oliveira; DIAS, Gabriella Mello Fontes Silva; SOUSA, Natália Cândido; FRANCESCO, Renata; CASTRO, Fábio Fernandes Morato; BARROS, Myrthes Toledo. Síndrome PFAPA (febre periódica, aftas orais, faringite e adenite cervical) em crianças e adultos. Arquivos de Asma Alergia e Imunologia, São Paulo, 2019. Disponível em: < http://aaai-asbai.org.br/detalhe_artigo.asp?id=965> Acesso em: 08 de out. de 2020.
MOREIRA, Filipa; PEREIRA, Gabriel; MARÇAL, Nuno; GUIMARÃES, Joana; MIRANDA, Daniel. Síndrome PFAPA – Caso clínico. Revista Portuguesa de Otorrinolaringologia e Cirurgia Cérvico-Facial, Braga, 2012. Disponível em: < https://www.journalsporl.com/index.php/sporl/article/view/95> Acesso em: 08 de out. de 2020.
SAMPAIO, Isabel; MARQUES, José Gonçalo. Síndrome de febre periódica, estomatite aftosa, faringite e adenite – Análise retrospectiva de 21 casos. Acta Médica Portuguesa, Lisboa, 2011. Disponível em: <actamedicaportuguesa.com> Acesso em: 08 de out. de 2020.
VANONI. Frederica; THEODOROPOULOU, Katerina; HOFER, Michaël. PFAPA syndrome: a review on treatment and outcome. Pediatric Rheumatology, Lausanne, 2016. Disponível em: < https://ped-rheum.biomedcentral.com/articles/10.1186/s12969-016-0101-9> Acesso em: 08 de out. de 2020.
[1] Resident in Otorhinolaryngology and Cervico-Facial Surgery, Graduate in Medicine at the University of Cuiabá – UNIC.
[2] Doctor in Otorhinolaryngology, Faculty of Medical Sciences, Santa Casa de São Paulo.
[3] Resident in Otorhinolaryngology and Cervico-Facial Surgery; Graduated in Medicine from the University of Cuiabá – UNIC.
[4] Resident in Otorhinolaryngology and Cervico-Facial Surgery; Graduation in Medicine from the Federal University of Paraná – UFPR.
[5] Medical student at the University of Cuiabá – UNIC.
Sent: August, 2020.
Approved: October, 2020.















