ORIGINAL ARTICLE
ARAGÃO, José Aderval [1], ARAGÃO, Iapunira Catarina Sant’Anna [2], ARAGÃO, Felipe Matheus Sant’Anna [3], LOURENÇO, Bárbara Costa [4], ALMEIDA, João Victor Rocha de [5], PORTO, Luciano Conceição [6], GUERRA, Danilo Ribeiro [7], FEITOSA, Vera Lúcia Correa [8], REIS, Francisco Prado [9]
ARAGÃO, José Aderval. et al. Biometrics of the suspensory ligament of the thyroid and its correlation with the morphometry of the thyroid gland in cadavers of human fetuses. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year. 08, Ed. 07, Vol. 05, pp. 55-73. July 2023. ISSN: 2448-0959, Access link: https://www.nucleodoconhecimento.com.br/health/biometrics-of-the-suspensory, DOI: 10.32749/nucleodoconhecimento.com.br/health/biometrics-of-the-suspensory
ABSTRACT
Introduction: Berry’s ligament (BL) is a known anatomical structure, which connects the thyroid gland to the tracheal wall, but its biometry has so far been little explored. Objective: In the present study, we sought to perform the BL biometry, correlating it with the morphometry of the thyroid gland. Material and method: Without the aid of optical instruments, the BL of 24 thyroid glands of human fetuses were dissected. With the gland in an anatomical position, the biometric data of the BL and the gland were taken. The data were treated statistically to establish the correlation between the length and height of the BL with the biometric data of the thyroid gland. Result: Significant correlations were found at the 5% level for the width of the thyroid gland and the weight of the gland, as well as for the length of the left lobe and the width of the right and left thyroid lobes, all in relation to the length of the LB and also the length in relation to the width of the gland and the isthmus of the thyroid gland. There was no significant correlation between the BL height and the morphometric findings of the right and left lobes and the isthmus of the thyroid gland. Conclusion: Knowledge of the anatomy of the BL is essential to prevent, in particular, injuries to the RLN, during thyroidectomy or parathyroidectomy.
Keywords: Berry’s Ligament, Suspensory ligament of thyroid gland, Recurrent Laryngeal Nerve, Tubercle of Zuckerkandl, Thyroid gland, Biometry.
1. INTRODUCTION
The suspensory ligament of the thyroid or Berry’s ligamnt (LB) is a dense condensation of the pretracheal vascular fascia that posteriorly connects the thyroid gland to the cricotracheal structures of the first to third tracheal rings (SASOU, NAKAMURA, KURIHARA, 1998; ARDITO et al., 2004; RANDOLPH et al., 2011; ASGHARPOUR et al., 2012; NGO NYEKI, 2015; SRITHARAN et al., 2016; MANTALOVAS et al., 2022). It is a region considered very vulnerable to injuries during thyroidectomy, due to the medial location of the BL in relation to the course of the recurrent laryngeal nerve (RLN), where it penetrates the larynx (THOMPSON, OLSEN, HOFFMAN, 1973; LORÉ, KIM, ELIAS, 1977; ARDITO et al., 2004; ASGHARPOUR et al., 2012). The location of the RLN in relation to the BL is controversial, and it has been emphasized that its identification decreases the incidence of nerve injury during thyroidectomy (LORÉ, KIM, ELIAS, 1977; DELBRIDGE et al., 1992). A better understanding of the frequency with which the RLN penetrates the BL may reduce complications, as traction-related injuries are associated with the RLN during the course of its penetration into the BL (HUNT, POOLE, REEVE, 1968; ARDITO et al., 2004). Furthermore, until now, data on the biometrics of the BL and the thyroid gland, as well as their histological characteristics, have rarely been described. In the present study, we sought to perform the BL biometry, correlating it with the morphometry of the thyroid gland.
2. MATERIAL AND METHODS
This is a descriptive anatomical study with morphometric data about the suspensory ligament of the thyroid gland. The BL were dissected (Figure 1) from 24 thyroid glands of human fetal cadavers belonging to the laboratory of human anatomy of the Department of Morphology of the Federal University of Sergipe, obtained in accordance with Law No. 8501 of November 30, 1992, which provides for the use of unclaimed cadavers in research. Of the 24 glands, 12 were from male fetuses and 12 from female fetuses. The age of the fetuses ranged from 20.3 to 36.8 weeks with a mean of 26.3 weeks. In male fetuses the age ranged from 22 to 36.8 weeks with a mean of 27.3 weeks and in females the mean was 25.3 weeks and ranged from 20.3 to 31.7 weeks. In the dissection, a skin incision was made, followed by the removal of the infrahyoid muscles, in which the thyroid gland surrounded by its false and true capsules was exposed. The samples included in the study were normal and without any pathology detected macroscopically. Thyroid glands that presented anatomical variations and developmental anomalies were excluded, such as: agenesis, partial or complete absence of the isthmus, accessory thyroid tissue, ectopic thyroid tissue and pyramidal lobe.
The biometric data of the BL and the thyroid gland were taken with the gland in its anatomical location, performed with the aid of a digital caliper with a precision of 0.01 mm. Afterwards, the thyroid gland was removed from its bed, dried with a sponge and blotting paper and weighed on a digital scale with a precision of 0.01 g. No attempt was made to remove the parathyroid glands as their weight was described as negligible (SNYDER et al., 1975).
3. STATISTICAL ANALYSIS
Categorical variables were described using absolute and relative frequency, percentage. Continuous variables were described using mean, standard deviation, median and interquartile range. Pearson’s correlation between morphometric variables was estimated and tested. The significance level adopted was 5% and the software used was R Core Team 2021.
Figure 1. Thyroid suspensory ligament or Berry’s ligament (circle)
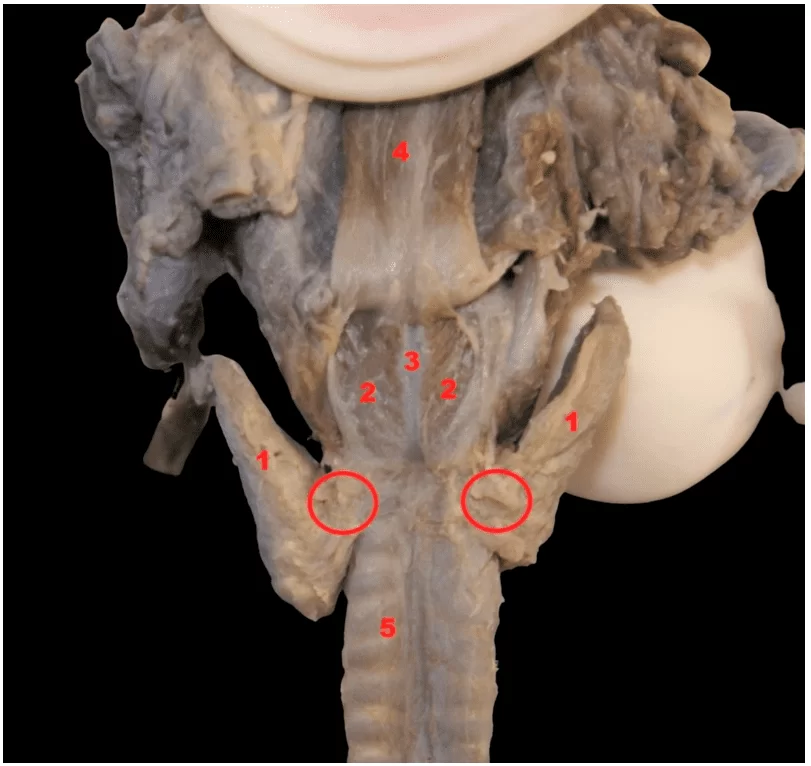
Legend
- Lobes of the thyroid gland
- Posterior cricoarytenoid muscles
- Cricoid cartilage
- Esophagus
- Trachea
4. RESULT
The BL of 24 thyroid glands dissected from human fetal cadavers belonging to the laboratory of human anatomy of the Department of Morphology of the Federal University of Sergipe, were obtained in accordance with the Law, which allows the use of unclaimed cadavers in research. Of the 24 glands, 12 were from male fetuses and 12 from female fetuses. The age of the fetuses ranged from 20.3 to 36.8 weeks, with a mean of 26.3 weeks. In male fetuses, the age ranged from 22 to 36.8 weeks with an average of 27.3 weeks and in females, the average was 25.3 weeks and ranged from 20.3 to 31.7 weeks.
Table 1 shows the averages of the morphometric data of the BL and the thyroid gland of fetuses. The mean age in weeks was 26.3 (SD: 4.6) and median 26.1 (IQR: 21.9-29.5) with a mean fetal height of 330 mm (SD: 104.8 mm) and median of 337 mm (IIQ: 302-375 mm). The mean width of the thyroid gland was 13.1 mm (SD: 2.8 mm) and median 12.7 mm (IQR: 11.5-13.7). The mean weight of the thyroid gland was 0.3 g (SD: 0.2 g) and median 0.2 g (IQR: 0.2-0.5 g). The length of the thyroid lobe had a mean of 11.7 mm (SD: 2.1 mm) and a median of 11.9 mm (IQR: 10.4-13.3 mm) on the right side and a mean of 10.8 mm (SD: 2.6 mm) and median of 11.6 mm (IQR: 8.9-12.6 mm) on the left side. The mean thyroid lobe width was 4.6 mm (SD: 1.2 mm) and median 4.6 mm (IQR: 3.8-5 mm) on the right side and mean 4.7 mm (SD: 1.4 mm) and median of 4.2 mm (IQR: 3.7-6.3 mm) on the left side. The width of the isthmus of the thyroid gland had a mean of 5.5 mm (SD: 2.1 mm) and a median of 5.1 mm (IQR: 4.3-6.4 mm), while its height had a mean of 4.8 mm (SD: 1.9 mm) and median of 4.6 mm (IQR: 3.5-5.7 mm). The average length of the BL was 1.5 mm (SD: 0.6 mm) and a median of 1.4 mm (IQR: 1-2 mm) on the right side and an average of 1.2 mm (SD: 0. 4 mm) and median of 1.1 mm (IIQ: 1-1.4 mm) on the left side, while height had a mean of 2.8 mm (SD: 0.7 mm) and a median of 2.8 mm (IQR: 2.3-3 mm) on the right side and a mean of 2.6 mm (SD: 0. 7 mm) and median of 2.7 mm (IQR: 2.4-3.2 mm) on the left side.
Table 1. Morphometry of the thyroid gland and BL
| n | % | Mean | SD | Median | Q1 | Q3 | |
| Sex | |||||||
| Female | 12 | 50 | |||||
| Male | 12 | 50 | |||||
| Age (weeks) | 26.3 | 4.6 | 26.1 | 21.9 | 29.5 | ||
| Fetal height (mm) | 330.0 | 104.8 | 337.0 | 302.0 | 375.0 | ||
| Width of the thyroid gland (mm) | 13.1 | 2.8 | 12.7 | 11.5 | 13.7 | ||
| Thyroid gland weight (g) | 0.3 | 0.2 | 0.2 | 0.2 | 0.5 | ||
| Thyroid lobe length (mm) | |||||||
| Right | 11.7 | 2.1 | 11.9 | 10.4 | 13.3 | ||
| Left | 10.8 | 2.6 | 11.6 | 8.9 | 12.6 | ||
| Thyroid lobe width (mm) | |||||||
| Right | 4.6 | 1.2 | 4.6 | 3.8 | 5.0 | ||
| Left | 4.7 | 1.4 | 4.2 | 3.7 | 6.3 | ||
| Width of the isthmus of the thyroid gland (mm) | 5.5 | 2.1 | 5.1 | 4.3 | 6.4 | ||
| Height of the isthmus of the thyroid gland (mm) | 4.8 | 1.9 | 4.6 | 3.5 | 5.7 | ||
| Length of the suspensory ligament of the thyroid (mm) | |||||||
| Right | 1.5 | 0.6 | 1.4 | 1.0 | 2.0 | ||
| Left | 1.2 | 0.4 | 1.1 | 1.0 | 1.4 | ||
| Height of the suspensory ligament of the thyroid (mm) | |||||||
| Right | 2.8 | 0.7 | 2.8 | 2.3 | 3.0 | ||
| Left | 2.6 | 0.7 | 2.7 | 2.4 | 3.2 |
Source: Authors, 2023.
Legend: n – absolute frequency. % – percentage relative frequency. SD – standard deviation. Q1 – First Quartile. Q3 – Third Quartile. IIQ – Interquartile Range
Figure 1 shows the correlations between the length of the BL and: the width and weight of the thyroid gland (A and B); length and width of the thyroid gland lobes (C, D, E, F); and width and height of the thyroid isthmus (G, H). It can be seen that significant correlations occurred at the 5% level for thyroid gland width (R: 0.7, positive and strong) and gland weight (R: 0.65, positive and median). Correlations also occurred for left lobe length (R: 0.47, positive and median) and right and left thyroid lobe width (R: 0.52 and 0.53, positive and median).
Figure 1. Correlation between right thyroid suspensory ligament length and thyroid gland morphometry
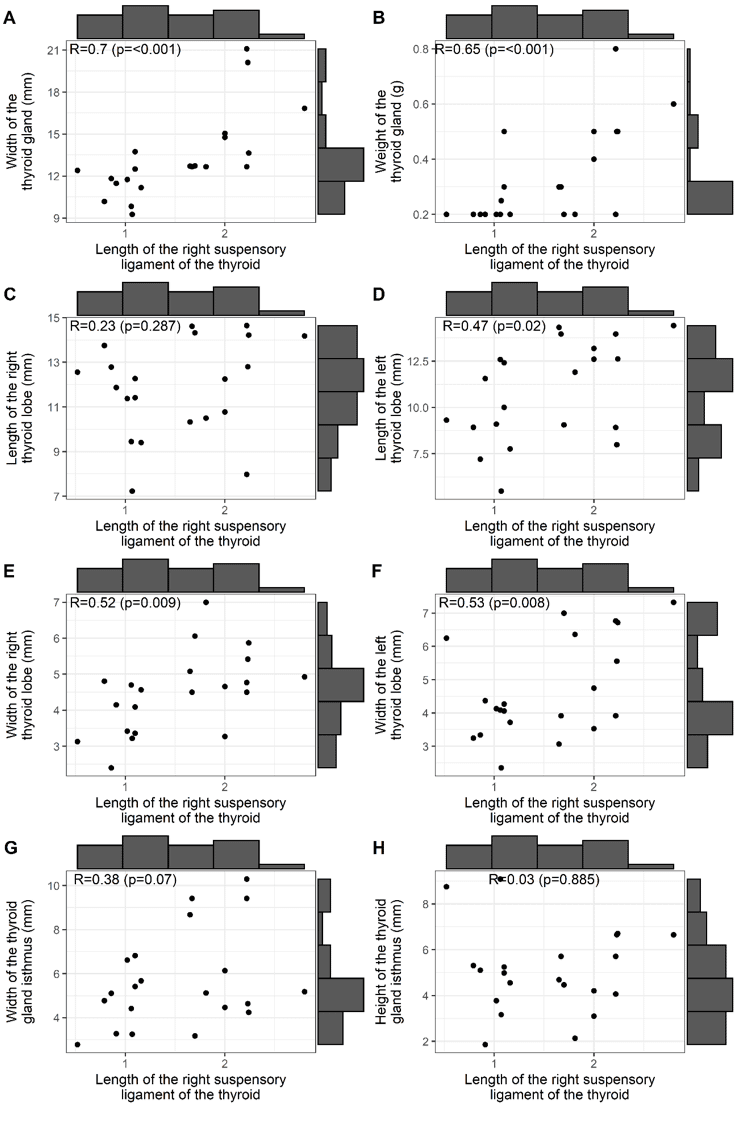
Figure 2 shows the correlations between the length of the BL and: the width and weight of the thyroid gland (A, B); the lengths of the right and left lobes of the thyroid gland (C, D); the widths of the right and left lobes of the thyroid gland (E, F); the width and height of the isthmus of the gland (G, H). It can be noted that only correlations at the 5% level were significant for the width of the thyroid gland (R: 0.51, positive and median) and the width of the isthmus of the thyroid gland (R: -0.56, negative and median).
Figure 2 – Correlation of the BL length with: width and weight, length and width of the right and left lobes and the width and height of the isthmus of the thyroid gland
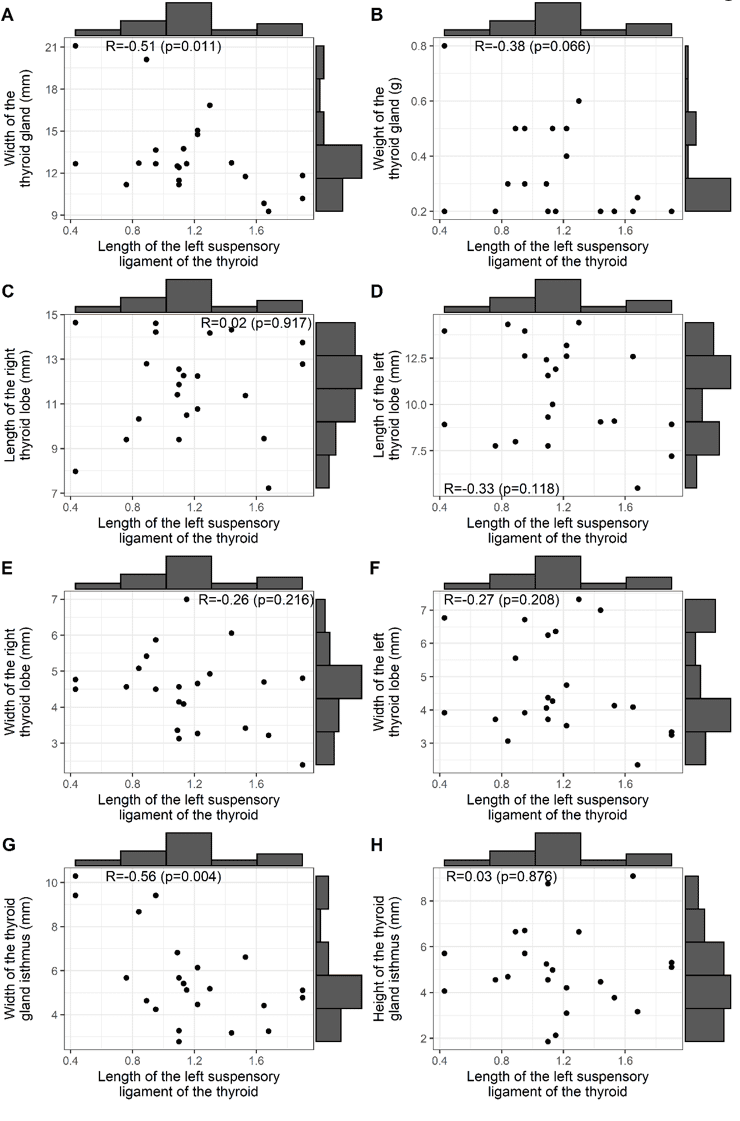
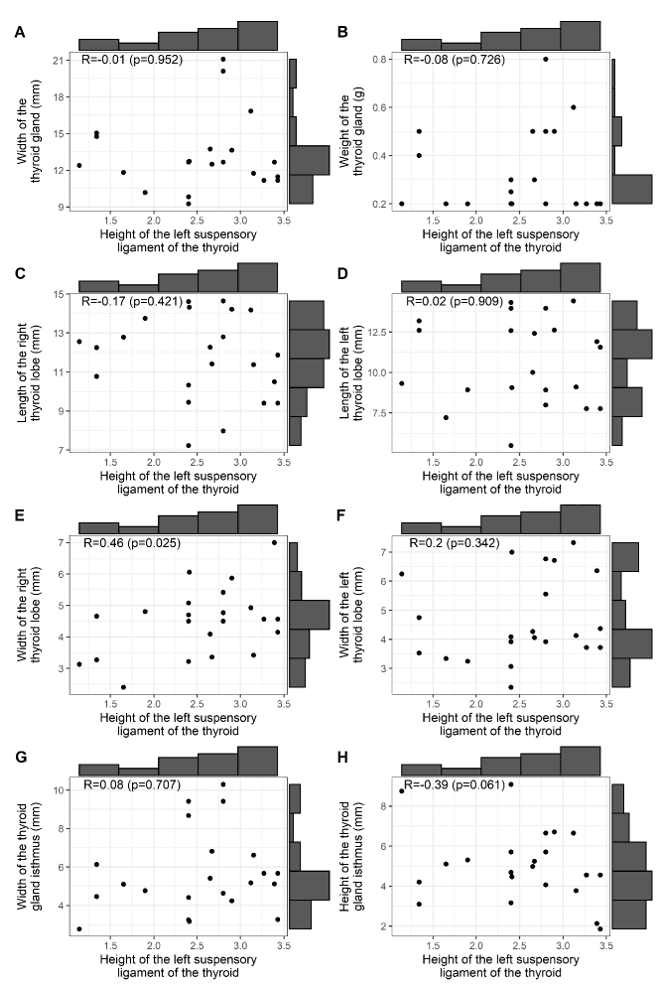
Figure 3 shows the correlations between the height of the right BL of the thyroid gland, with: the width and weight of the thyroid gland (A, B); the lengths of the right and left lobes of the thyroid gland (C, D); the widths of the right and left lobes of the thyroid gland (E, F); the width and height of the isthmus of the gland (G, H). Note that there was no significant correlation between the height of the BL and the morphometric findings of the thyroid gland and the isthmus of the gland.
Figure 3 – Correlation of BL height with: width and weight, lengths and widths of the right and left lobes, and width and height of the isthmus of the thyroid gland
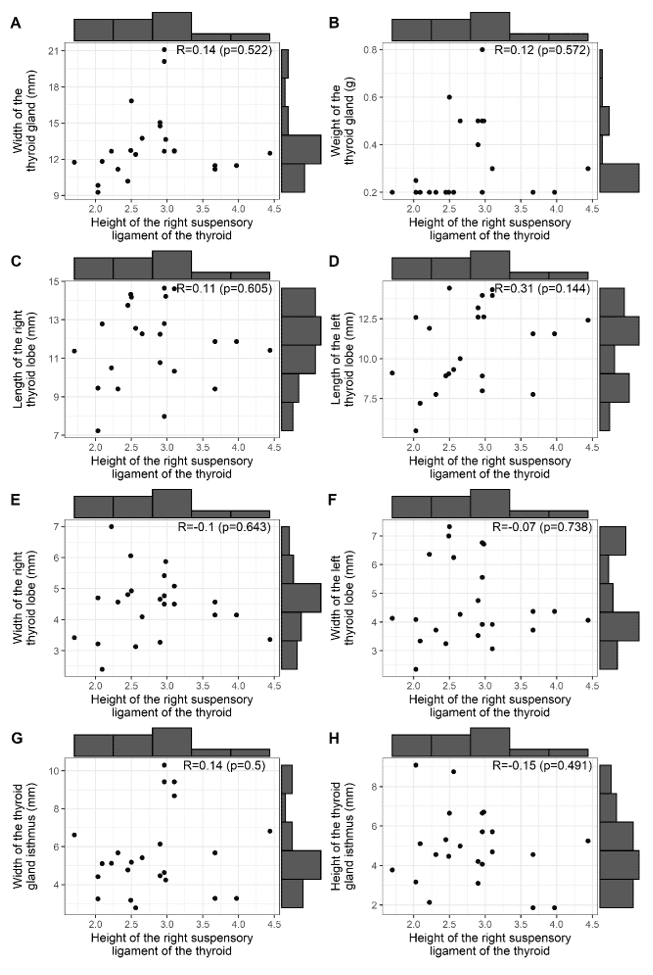
Figure 4 represents the correlations between the height of the left BL of the thyroid gland and: the width and weight of the thyroid gland (A, B); the lengths of the right and left lobes of the thyroid gland (C, D); the widths of the right and left lobes of the thyroid gland (E, F); the width and height of the isthmus of the gland (G, H). Note that there was no significant correlation between the height of the BL and the morphometric findings of the thyroid gland and the isthmus of the gland.
Figure 4 – Correlation of the height of the left thyroid gland BL with: the width and weight of the thyroid gland, the lengths of the right and left lobes of the thyroid gland, the widths of the right and left lobes of the thyroid gland and the width and height of the gland isthmus
5. DISCUSSION
The thyroid gland, although easily detached from the trachea by forceps, was not separated, according to BL Sasou, Nakamura, Kurihara (1998), they described the BL as a whitish band of connective tissue connecting the thyroid gland to the tracheal wall, when the thyroid gland was separated from the trachea and lifted anteriorly. For Sritharan et al., (2016), it would be a dense condensation of the pre-tracheal vascular fascia that connected the thyroid to the cricotracheal structures posteriorly. In our study, the BL was also observed as a whitish band of connective tissue that connected the thyroid gland to the tracheal wall. For SERPELL, (2010) this relatively avascular fibrous layer, the true BL, would be found medially and deeply to the recurrent laryngeal nerve (RLN).
Sasou, Nakamura, Kurihara, (1998); Serpell, (2010); Sritharan et al. (2016), described the BL in adults as a dense fibrous band from the cricoid cartilage to the first and third tracheal rings, firmly fixing the thyroid gland to the larynx and tracheal wall. They found a ligament length that ranged from 8 to 14 mm (mean of 11.5 mm) and width from 2 to 7 mm (mean of 4.4 mm). In the present study, in human fetuses, the length of the BL ranged from 0.52 to 2.24 mm on the right (mean of 1.5 mm) and on the left from 0.43 to 1.68 mm (mean of 1.2 mm) height ranged from 1.7 to 4.44 mm (mean 2.8 mm) on the right and 1.14 to 3.43 mm (mean 2.6 mm) on the left. In the literature, a relationship between injury to the RLN and the BL has often been pointed out. RLN injury is one of the most serious complications of thyroidectomy, and the BL has been referred to as the most frequent site of nerve injury. According to the American Society for Head and Neck Surgery, voice changes after thyroidectomy have ranged from 30 to 87%, while NLR damage is underestimated (3 to 5%) and appears to be approaching 10% (JEANNON et al., 2009; FRANCIS et al., 2014; FUNDAKOWSKI et al., 2018). For Chiang et al., (2010); Chiang et al., (2011), post-thyroidectomy voice disorders generally approach a proportion of 10%. Before the use of intraoperative neurostimulation, the only test approved for RLN injury was postoperative laryngoscopy and evaluation of the vocal cords, whenever the injury escaped intraoperative recognition. The ability to define the exact time and region of injury intraoperatively was made possible by a loss of signal during NLR stimulation (MARCUS et al., 2003; SNYDER et al., 2008; CHIANG et al., 2010; CHIANG et al. al., 2011; DIONIGI et al., 2015; STOPA et al., 2017; WU et al., 2017; LIU et al., 2018; MANTALOVAS et al., 2022). According to SNYDER et al. (2008), injured nerves are usually intact intraoperatively (0.45%) and have been attributed to a type of functional nerve injury during thyroidectomy. Chiang et al., (2008) mentioned that functional nerve injuries constitute more than 75% of all injuries. This type of damage would occur as a result of traction pressures acting on the BL during central rotation of the thyroid gland.
Intraoperatively, the RLN can be identified by various techniques, such as palpation, intraoperative monitoring, and direct inspection provided by key anatomical landmarks such as the BL, tracheoesophageal sulcus, inferior thyroid artery, and the midpoint of the posterior border of the thyroid gland or Zukerkandl’s tubercle. The relationship of the nerve to these landmarks is variable (Henry et al., 2017), but improves the sensitivity of intraoperative nerve monitoring (PATRA et al., 2022).
Authors such as Sasou, Nakamura, Kurihara (1998); Botelho et al., (2012), proposed the BL as a reliable anatomical landmark to locate the RLN intraoperatively. However, this has not yet been widely accepted and implemented as standard practice (ASGHARPOUR et al., 2012). Some data showed wide variations in the location of the RLN in relation to the BL: the nerve would course superficially to the BL, with a variation from zero to 100% (CAKIR et al., 2006; NOUSSIOS et al., 2020); meanwhile, the penetrating pattern would vary from 0 to 31.6% (CAKIR et al., 2006; HUNT et al., 1968; LEOW, WEBB, 1998; SASOU, NAKAMURA, KURIHARA, 1998; PRADEEP et al., 2012).
6. CONCLUSION
Knowledge of the BL biometry, and its anatomical relationship with the thyroid gland and RLN, are essential to prevent, in particular, RLN injuries, during thyroidectomy or parathyroidectomy.
REFERENCES
ARDITO, G. et al. Revisited anatomy of the recurrent laryngeal nerves. Am J Surg, v. 187, n. 2, p. 249-53, 2004.
ASGHARPOUR, E. et al. Recurrent laryngeal nerve landmarks revisited. Head Neck, v. 34, n. 9, p. 1240-6, 2012.
BOTELHO, J.B. et al. Estudo das relações anatomocirúrgicas entre os nervos laríngeos recorrentes e o ligamento de Berry [Anatomic and surgical study of the recurrent laryngeal nerve and its involvement with the ligament of Berry]. Rev Col Bras Cir, v. 39, n. 5, p. 364-7, 2012.
CAKIR, B.O. et al. Reliable surgical landmarks for the identification of the recurrent laryngeal nerve. Otolaryngol Head Neck Surg, v. 135, n. 2, p. 299-302. 2006.
CHIANG, F.Y. et al. Standardization of intraoperative neuromonitoring of recurrent laryngeal nerve in thyroid operation. World J Surg, v. 34, n. 2, p. 223-9, 2010.
CHIANG, F.Y. et al. The mechanism of recurrent laryngeal nerve injury during thyroid surgery–the application of intraoperative neuromonitoring. Surgery, v. 143, n. 6, p. 743-9, 2008.
CHIANG, F.Y. et al. Does extensive dissection of recurrent laryngeal nerve during thyroid operation increase the risk of nerve injury? Evidence from the application of intraoperative neuromonitoring. Am J Otolaryngol, v. 32, n. 6, p. 499-503, 2011.
DELBRIDGE, L. et al. Total thyroidectomy: the technique of capsular dissection. Aust N Z J Surg, v. 62, n. 2, p. 96-9, 1992.
DIONIGI, G. et al. Continuous Intraoperative Neuromonitoring (C-IONM) Technique with the Automatic Periodic Stimulating (APS) Accessory for Conventional and Endoscopic Thyroid Surgery. Surg Technol Int, v. 26, p. 101-14, 2015.
FRANCIS, D.O. et al. Epidemiology of vocal fold paralyses after total thyroidectomy for well-differentiated thyroid cancer in a Medicare population. Otolaryngol Head Neck Surg, v. 150, n. 4, p. 548-57, 2014.
FUNDAKOWSKI, C. E. et al. Surgical management of the recurrent laryngeal nerve in thyroidectomy: American Head and Neck Society Consensus Statement. Head Neck, v. 40, n. 4, p. 663-675, 2018.
HENRY, B. M. et al. The Reliability of the Tracheoesophageal Groove and the Ligament of Berry as Landmarks for Identifying the Recurrent Laryngeal Nerve: A Cadaveric Study and Meta-Analysis. Biomed Res Int, 2017.
HUNT, P.S.; POOLE, M.; REEVE, T.S. A reappraisal of the surgical anatomy of the thyroid and parathyroid glands. Br J Surg, v. 55, n. 1, p. 63-6, 1968.
JEANNON, J.P. Diagnosis of recurrent laryngeal nerve palsy after thyroidectomy: a systematic review. Int J Clin Pract, v. 63, n. 4, p. 624-9, 2009.
LEOW, C.K.; WEBB, A.J. The lateral thyroid ligament of Berry. Int Surg, v. 83, n. 1, p. 75-8, 1998.
LIU X. et al. Laryngeal nerve morbidity in 1.273 central node dissections for thyroid cancer. Surg Oncol, v. 27, n. 2, p. A21-A25, 2018.
LORÉ, J.M. J.R.; KIM, D.J.; ELIAS, S. Preservation of the laryngeal nerves during total thyroid lobectomy. Ann Otol Rhinol Laryngol, v. 86, n. 6 Pt 1, p. 777-88, 1977.
MANTALOVAS, S. Surgical Significance of Berry’s Posterolateral Ligament and Frequency of Recurrent Laryngeal Nerve Injury into the Last 2 cm of Its Caudal Extralaryngeal Part (P1) during Thyroidectomy. Medicina (Kaunas), v. 58, n. 6, p. 755, 2022.
MARCUS, B. et al. Recurrent laryngeal nerve monitoring in thyroid and parathyroid surgery: the University of Michigan experience. Laryngoscope, v. 113, n. 2, p. 356-61, 2003.
NGO, NYEKI A. R. et al. Recurrent laryngeal nerve landmarks during thyroidectomy. Eur Ann Otorhinolaryngol Head Neck Dis, v. 132, n. 5, p. 265-9, 2015.
NOUSSIOS, G. et al. The Anatomical Relationship of Inferior Thyroid Artery and Recurrent Laryngeal Nerve: A Review of the Literature and Its Clinical Importance. J Clin Med Res, v. 12, n. 10, p. 640-646, 2020.
PATRA, A. et al. Identification of valid anatomical landmarks to locate and protect recurrent laryngeal nerve during thyroid surgery: a cadaveric study. Surg Radiol Anat, 2022.
PRADEEP, P.V.; JAYASHREE, B.; HARSHITA, S.S. A Closer Look at Laryngeal Nerves during Thyroid Surgery: A Descriptive Study of 584 Nerves. Anat Res Int, 2012.
RANDOLPH, G.W. et al. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope. v. 121, Suppl 1:S1-16, 2011.
SASOU, S.; NAKAMURA, S.; KURIHARA, H. Suspensory ligament of Berry: its relationship to recurrent laryngeal nerve and anatomic examination of 24 autopsies. Head Neck, v. 20, n. 8, p. 695-8, 1998.
SERPELL, J.W. New operative surgical concept of two fascial layers enveloping the recurrent laryngeal nerve. Ann Surg Oncol, v. 17, n. 6, p. 1628-36, 2010.
SNYDER, S.K. et al. Elucidating mechanisms of recurrent laryngeal nerve injury during thyroidectomy and parathyroidectomy. J Am Coll Surg, v. 206, n. 1, p. 123-30, 2008.
SNYDER, W.S. et al. Report of the Task Group on Reference Man. Oxford: Pergamon Press, v. 23, n. 75, p. 80015-8, 1975. Disponível em: https://doi.org/10.1016/S0074-2740.
SRITHARAN, N. et al. The Ligament of Berry. In: RANDOLPH, G.W. (Ed.). The Recurrent and Superior Laryngeal Nerves. Switzerland: Springer, p. 103-113, 2016. Disponível em: https://doi.org/10.1007/978-3-319-27727-1_10.
STOPA, M.; BARCZYŃSKI, M. Prognostic value of intraoperative neural monitoring of the recurrent laryngeal nerve in thyroid surgery. Langenbecks Arch Surg, v. 402, n. 6, p. 957-964, 2017.
THOMPSON, N.W., OLSEN, W.R., HOFFMAN, G.L. The continuing development of the technique of thyroidectomy. Surgery, v. 73, n. 6, p. 913-27, 1973.
WU, C.W. et al. Recurrent laryngeal nerve injury with incomplete loss of electromyography signal during monitored thyroidectomy-evaluation and outcome. Langenbecks Arch Surg, v. 402, n. 4, p. 691-699, 2017.
[1] Advisor. Titular Professor of Clinical Anatomy. ORCID: https://orcid.org/0000-0002-2300-3330. Currículo Lattes: http://lattes.cnpq.br/6911783083973582.
[2] Medical Clinic Resident. ORCID: https://orcid.org/0000-0002-5298-537X. Currículo Lattes: http://lattes.cnpq.br/6291628187714859.
[3] Medical Clinic Resident. ORCID: https://orcid.org/0000-0001-9211-7000. Currículo Lattes: http://lattes.cnpq.br/4619345212343744.
[4] Medical Student. ORCID: https://orcid.org/0000-0001-5924-8658. Currículo Lattes: http://lattes.cnpq.br/1862815448788019.
[5] Medical Student. ORCID: https://orcid.org/0000-0001-6974-169X. Currículo Lattes: http://lattes.cnpq.br/7562287657874077.
[6] Medical Student. ORCID: https://orcid.org/0009-0006-0486-3980. Currículo Lattes: http://lattes.cnpq.br/4418868415307533.
[7] Adjunct Professor of Clinical Anatomy. ORCID: https://orcid.org/0000-0002-2146-3499. Currículo Lattes: http://lattes.cnpq.br/3543011108453552.
[8] Titular Professor of Molecular Biology. ORCID: https://orcid.org/0000-0001-5705-6433. Currículo Lattes: http://lattes.cnpq.br/3337321488338686.
[9] Titular Professor of the Medical School. ORCID: https://orcid.org/0000-0002-7776-1831. Currículo Lattes: http://lattes.cnpq.br/6858508576490184.
Submitted: May 10, 2023.
Approved: June 27, 2023.















