ORIGINAL ARTICLE
JESUS, Elaine Andrade de [1], ARAGÃO, Iapunira Catarina Sant’Anna [2], ARAGÃO, Felipe Matheus Sant’Anna [3], FEITOSA, Vera Lúcia Correa [4], REIS, Francisco Prado [5], ARAGÃO, José Aderval [6]
JESUS, Elaine Andrade de. et al. Assessment of postural balance in patients with stroke. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year 08, Issue 07, Vol. 02, pp. 23-41. April 2023. ISSN: 2448-0959, Access link: https://www.nucleodoconhecimento.com.br/health/assessment-of-postural, DOI: 10.32749/nucleodoconhecimento.com.br/health/assessment-of-postural
ABSTRACT
The Cerebral Vascular Accident (CVA) results in disabilities of paretic limbs, but few studies have investigated the impacts of CVA on perception deficits as well as related functional changes. Motor function alterations caused by CVA, such as the presence of associated reactions, loss of postural control mechanisms, and tone disorders, shift the body’s center of gravity, generating a risk of falls. The aim of the present study was to evaluate postural balance changes in patients affected by CVA using the POMA-Brazil Scale (Performance Oriented Mobility Assessment). A cross-sectional study was conducted to assess postural balance changes in patients diagnosed with CVA undergoing rehabilitation at the UNIT Health Center, CEMISE Physiotherapy Service, and Maria Virgínia Leite Franco Rehabilitation Center in Aracaju, Sergipe. The B-POMA subscale consists of 13 tasks (sitting balance, rising from a chair, immediate standing balance, standing balance, eyes closed balance, 360-degree turning balance, resistance to displacement (Nudge Test), neck turning, unipedal stance balance, spinal extension, reaching upward, leaning forward, and sitting), aimed at detecting fall risk factors in elderly individuals with disabilities or chronic illnesses. Descriptive statistics were used for numerical variables, frequency distribution for demographic and clinical variables, and individuals per task, with the application of the chi-square test and the Student’s t-test. Among the tasks measured according to the B-POMA subscale, sitting balance was the most frequent qualitative response (97.5%), followed by immediate standing, eyes closed, and leaning forward. Unipedal stance balance was the least common normal task (25%), and 360-degree turning was the most adaptive (62.5%). Balance changes are associated with cerebral vascular accidents in terms of dynamic equilibrium. This study demonstrated that unipedal stance balance was the most affected task, 360-degree turning balance was the most adaptive, and sitting balance was the least affected. There were no significant differences in balance scores based on sex, age, and time of injury.
Keywords: Cerebral Vascular Accident, Postural Balance, Hemiplegic, Stroke Rehabilitation, Proprioceptive Stimulation.
INTRODUCTION
A Cerebral Vascular Accident (CVA) is defined as a focal clinical condition of vascular origin and rapid development that affects brain function (ARAÚJO et al., 2008). The sudden interruption of cerebral vascular flow, whether hemorrhagic or ischemic, results in physical consequences (plegia or paresis), alterations in tone, sensory, psycho-affective (depression, aggression, anxiety), and cognitive (memory problems, attention, perceptual deficits, language disorders, concentration, and planning difficulties) (TEIXEIRA-SALMELA et al., 2003; CORRIVEAU et al., 2004; BENSOUSSAN et al., 2006). According to MARCUCCI et al. (2007), it is also the main cause of chronic disability in adults.
Balance and postural control are fundamental components for the performance of activities and motor skills (CHAGAS, MONTEIRO, 2004; ONIGBINDE, AWOTIDEBE, AWOSIKA, 2009). Motor function alterations caused by CVA, such as the presence of associated reactions, loss of postural control mechanisms, and tone disorders, shift the body’s center of gravity, generating a risk of falls, regardless of age and time of injury (SIMOCELI et al., 2003).
According to TYSON et al. (2006) and LO, STEPHENSON, LOCKWOOD (2017), this also implies impairment in activities of daily living and mobility. After a CVA, the difficulty of permanent balance is often due to unequal weight distribution on the unaffected side of the body (BOHANNON, 1987; BARCLAY-GODDARD et al., 2004). Muscle activation in hemiparetic patients is replaced by the contraction of agonist and antagonist muscles or delayed activation of agonist muscles, generating compensatory activity of the affected limb (KIRKER et al., 2000).
The clinical picture of CVA, depending on its severity, can produce aggravations and sequels capable of compromising balance functions. These aggravations and sequels are frequently present in patients who have suffered a CVA and are responsible for functional alterations (CHENG et al., 2004; TYSON et al., 2006; FUJISAWA, TAKEDA, 2006; MARCUCCI et al., 2007; de OLIVEIRA et al., 2008; SILVA et al., 2008; MENEGHETTI et al., 2009; CLAYTON et al., 2021). According to TESSEM, HAGSTRØM, FALLANG (2007) and LIU et al. (2021), the recovery of postural balance after a CVA is considered essential to achieve independence in other vital functions. Generally, individuals affected by CVA experience postural control alterations that make them prone to fall risk (CHENG et al., 2004); thus, GOMES (2003) translated and validated the Poma Scale, an instrument to assess balance alterations in patients with CVA and Parkinson’s disease. Therefore, the present research aimed to evaluate postural balance changes in patients affected by CVA using the POMA-Brazil Scale.
METHODOLOGY
A descriptive cross-sectional study was conducted to assess postural balance changes in patients diagnosed with CVA who were undergoing rehabilitation at the UNIT Health Center, CEMISE Physiotherapy Service, and Centro de Reabilitação Maria Virgínia Leite Franco, all located in Aracaju, Sergipe. Out of the total of 125 CVA patients, 40 adult spastic hemiparetic patients with six months of injury were included in the study, and patients with acute and chronic CVAs who were non-ambulatory, had dementia, cognitive disorders, aphasia, double hemiparesis/plegia, and/or tetraparesis/plegia were excluded. All participants were informed and signed the Informed Consent Form (ICF). The study was approved by the Ethics and Research Committee of Universidade Tiradentes, protocol no: 031209.
To detect fall risk factors in elderly individuals with disabilities or chronic illnesses, GOMES (2003) translated and validated the POMA-Brazil Scale (Performance Oriented Mobility Assessment), an instrument that consists of two parts, one for assessing balance and another for gait. This scale is part of a protocol of test application recommendations, aiming at the detailed detection of fall risk factors in elderly individuals, based on the number of chronic disabilities (Annex 1). The patient starts the sitting balance test in a chair with a backrest and without arm support, with the back and feet supported, with 90º hip and knee flexion, in a well-lit area, flat and regular ground. For each test, instructions were given and the tasks of the B-POMA subscale were demonstrated, without the need for prior training. This subscale was the instrument used to assess balance changes in patients affected by CVA. It consists of 13 tasks (sitting balance, rising from a chair, immediate standing balance, standing balance, eyes closed balance, 360-degree turning balance, resistance
to displacement (Nudge Test), neck turning, unipedal stance balance, spinal extension, reaching upward, leaning forward, and sitting). It presents three levels of qualitative responses for its tasks, and each level has a specific score: normal (3 points), adaptive (2 points), and abnormal (1 point), allowing a score from 13 (worst balance state) to 39 points (best balance state). Descriptive statistics were used for numerical variables, frequency distribution for demographic and clinical variables, and individuals per task. The Student’s t-test was used to compare the time of injury of CVA patients with balance scores.
RESULTS
Out of the 40 spastic hemiparetic patients included in the study, 53% (21) were male and 48% (19) were female, with ages ranging from 35 to 79 years. The numerical values of the variables: age, number of associated diseases, time of CVA injury, and body mass index (BMI) are shown in Table 1. Of these patients, 12 were obese, five males and seven females, and 14 were overweight, 10 males and four females.
Table 1. Descriptive analysis of numerical variables of the studied patients
| Age | Number of Diseases | BMI | Injury Time (months) | |
| Mean | 59,65 | 1,43 | 28,22 | 34,03 |
| Standard Deviation | 9,88 | 0,64 | 4,49 | 3,95 |
BMI – Body Mass Index.
Source: Authors, 2023.
Among the tasks measured according to the B-POMA subscale, sitting balance (97.5%) was the most frequent qualitative response. Meanwhile, the unipedal stance balance task (25%) was the least common. The relative frequency and the absolute number of participating individuals in tasks within the levels of each category are presented in Figure 1.
Figure 1: Distribution of relative frequency, participation per balance task within each qualitative response according to the B-POMA scale (Brazil), of patients with CVA
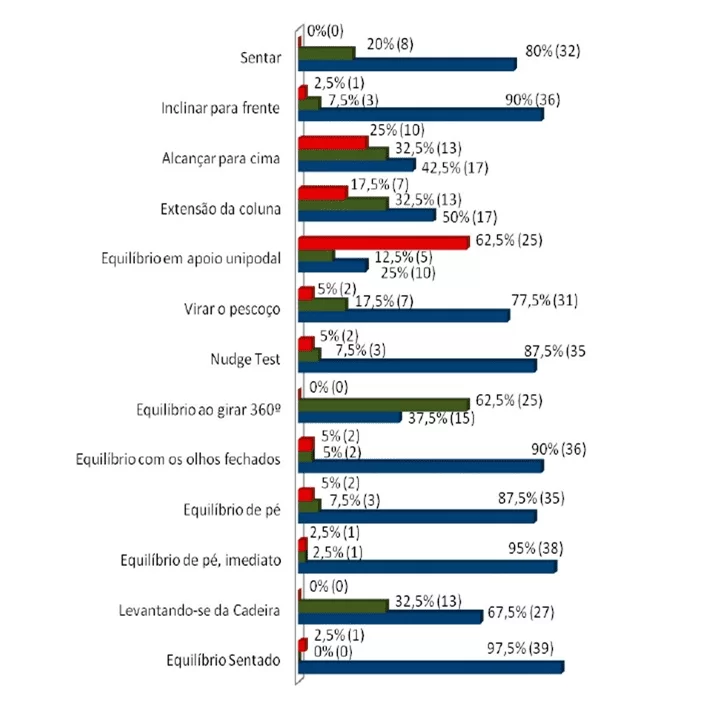
According to the qualitative scores of the B-POMA subscale (abnormal, adaptive, and normal), in males, out of the 13 tasks performed, seven were executed without abnormalities and thus considered normal (sitting, leaning forward, Nudge Test task, 360-degree turning balance, immediate standing balance, rising from a chair, and sitting balance). Three male patients did not show adaptation (eyes closed balance, standing balance, immediate standing balance, and sitting balance), and two tasks were qualitatively normal (immediate standing balance and sitting balance). In females, three tasks did not score in the abnormal response (sitting, 360-degree turning balance, and rising from a chair), and one scored in the adaptive response (sitting balance). It can be highlighted that in the normal response, no task achieved a score of 100%.
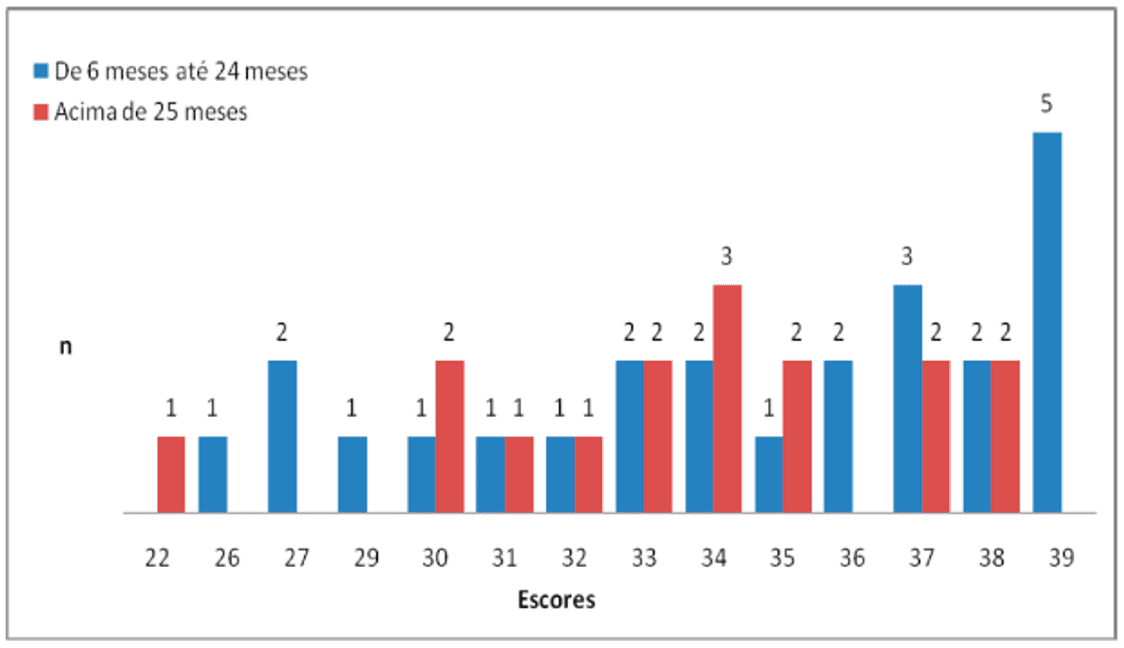
When comparing the injury time of CVA patients, from 6 to 24 months (n=24, 60%) and above 25 months (n=16, 40%), with balance scores, no significant difference occurred (p=0.29) (Figure 2).
Figure 2. Distribution of individuals by balance score in relation to injury time in B-POMA
DISCUSSION
With the exception of single-leg standing balance, which was the most impaired among the qualitative normality measures, the results of the other variables analyzed through the B-POMA subscale showed good adaptation, and some had high frequency. DE OLIVEIRA et al. (2008) warned that care should be taken as tasks considered easy to perform might mask evaluation results. Similar to sitting balance, other tasks demonstrated good participation frequency within this category: immediate standing balance, standing balance, eyes closed balance, Nudge Test, neck rotation, leaning forward, and sitting. According to Perlmutter, Lin, Makhsous (2010), sitting balance depends on trunk musculature, and dysfunction increases with task complexity.
Verheyden et al. (2009) reported that trunk exercises aim to improve sitting balance and selective trunk movements, also benefiting selective performance in lateral trunk flexion. RYERSON et al. (2008) and VAN CRIEKINGE et al. (2020) stated that the trunk position formation might be a crucial strategy during intervention to enhance trunk stability, being a precursor to balance and functional activities in post-stroke patients. GEIGER et al. (2001) explained that thigh support measure (base of support) significantly increases the involvement of the affected lower limb, improving this support and sitting balance.
TYSON et al. (2006) drew attention to the scarcity of detailed information regarding balance changes in stroke patients. Tessem, Hagstrøm, Fallang (2007) reported that individuals affected by stroke experience significantly uneven weight distribution on the unaffected side. According to MORISHITA et al. (2009), this leads to the patients’ body axis being inclined towards the non-paretic side, causing alterations in standing balance. ROERDINK et al. (2009) described that patients with severe motor limitations of the paretic leg use an effective strategy of asymmetrical weight support and lateralized control. GEIGER et al. (2001) had previously noted that there is greater agility and speed in skills and overload when rising on the compromised leg.
In light of these findings, attention can be drawn to the tasks of standing and immediate standing balance. In the present study, these tasks, in general, were frequently performed with good frequency, and it was more frequent in males.
According to SLABODA et al. (2009) and KARUKA, SILVA, NAVEGA (2011), stroke survivors rely on multiple visual and sensory inputs, and when these are present, they offer difficulties in resolving conflicts between somatosensory and visual inputs. The present study generally indicated a higher frequency of normal qualitative completion for the eyes closed balance task (90%) compared to neck rotation (77.7%). The relative frequency values of these tasks were higher in males. It should be noted that the frequency values obtained for the adaptive qualitative response of neck rotation were also higher in males.
According to KIM et al. (2009), this type of response for eyes closed balance and neck rotation may be related to the fact that virtual reality might have an enhanced effect on balance and motor recovery in individuals with stroke. Furthermore, MANOR et al. (2010) suggested that strategies emphasizing postural tasks under reduced visual conditions could enhance functional recovery in these individuals.
According to HARRIS et al. (2005), reactive balance with body or ground disturbances (pushes) causes the individual to move and alternate their feet, seeking stability and thus achieving balance. In the Nudge Test task, the patients in the present study generally showed a participation frequency of 87.5%, with 5% of this frequency occurring in the abnormal qualitative response and 7.5% in the adaptive response. In terms of gender, males had a higher participation frequency in the normal and adaptive qualitative categories, with no abnormal qualitative response. Meanwhile, the female participants showed a low frequency in the adaptive category and 11% in the abnormal qualitative response.
An exception was the leaning forward task, with a frequency of 90% in the normal qualitative response, 2.5% in the abnormal response, and 7.5% in the adaptive response. In terms of gender, the abnormal qualitative response had a higher frequency among females, while it decreased for the adaptive and normal categories. CORDO, NASHNER (1982), CROSBIE (1995), and VARAS-DIAZ et al. (2022) emphasized that the lower limbs are crucial in balance tasks as the peak ground reaction force occurs at the end of upper limb reach. Therefore, these authors stated that stroke patients could be trained to actively improve the affected lower limb’s performance during forward displacement of the body axis, due to the arm’s length to reach an object without losing balance.
The adaptive qualitative response was most notable in the 360-degree turning balance task. This finding applied to both the general patients and the genders. No frequency was recorded in the abnormal category, and the adaptive frequency was higher in females. Literature has highlighted that when an individual fails to perform tasks physiologically, considered normal, they adapt by using other auxiliary mechanisms to complete them. According to HARRIS et al. (200
5), an individual performing an activity like 360-degree turning balance (dynamic) needs to alternate their lower limbs to move and maintain balance, explaining the periods of adaptations in dynamic balance.
GENTHON et al. (2008) emphasized that studies have confirmed this adaptive ability in stroke patients with spatial neglect. For these authors, this might be due to the insufficient and ineffective postural control of the paretic limb, leading the individual to seek adaptive stabilization of the unaffected limb, which might be unable to compensate for this deficiency, resulting in overall postural instability.
HAUER et al. (2003), GRAF et al. (2005), and DOMÍNGUEZ-CARRILLO et al. (2007) described that alterations in single-leg standing balance affect the characteristics of activities of daily living (ADLs), such as climbing stairs, transfers, changes in position and direction of the center of gravity, causing older adults to seek a defense mechanism to balance, expanding the base of support and reducing the height of the center of gravity. In this study, from a qualitative response standpoint, single-leg standing balance was, in general, among patients, both the most and least frequently performed task. In males, the adaptive response frequency was 18.2%, and in females, it was 5.5%. However, for the normal qualitative response, the best frequency occurred in females (27.8%).
HOWE et al. (2005) reported that rehabilitation in the acute phase after stroke, with the aim of reinforcing lateral weight transfers, does not seem to improve, attributing the improvement to standard care and natural recovery. In contrast, BOHANNON (1987), LISTON, BROUWER (1996), and NICHOLS (1997) emphasized that hemiparetics and hemiplegics have decreased balance, and postural oscillation might be twice that of individuals of the same age without impairments. All these findings undoubtedly result from motor disorganizations occurring in post-stroke patients.
Considering the level of scores obtained by patients, the data indicated that although men scored higher score levels (33 to 39), these findings were not statistically significant. Conversely, in females, lower scores predominated (22 to 32), and these were also not statistically significant. According to PETREA et al. (2009), women tend to have a greater deficit in their ADLs than men. For BASSI et al. (2010), different sex-associated pathophysiological mechanisms appear to have a significant effect on functional recovery after rehabilitation.
PAOLUCCI et al. (2006) and DUARTE et al. (2009) described that functional recovery has a better prognosis in men than in women, regardless of the acute or subacute phase. However, they did not clarify the reason for this sex-related difference in recovery, often attributing it to greater muscle strength among men. Furthermore, after injury, women have worse functional outcomes, more depression, and lower quality of life than men. Age range and time since injury have been two highlighted variables among authors.
MENEGHETTI et al. (2009) and AN, LEE, LEE (2014) pointed out that stroke-affected individuals have a high risk of falls regardless of the time since injury and age and that significant motor functional recovery occurs from 1 to 3 months after stroke (VERHEYDEN et al., 2008). Among the studied patients, more than 50% achieved scores ranging from 33 to 39, with 19 of them falling within the age range of 60-79 years. The lowest score levels occurred in the age ranges of 40-49 for females and 60-69 years for males.
Regarding the time since injury, 17 individuals with injuries ranging from 6 to 24 months and 11 with injuries above 25 months obtained scores between 33 and 39. Nonetheless, for both age and time since injury, statistically, there was no significance. It is relevant to note that some studies have reported that individuals with chronicity of injury may develop performance strategies in tasks (MENEGHETTI et al., 2009) and that stroke patients, while developing motor learning strategies, impair their ability to consciously control the mechanics of their movements (VERHEYDEN et al., 2008; MENEGHETTI et al., 2009), and postural stability increases within the first year after stroke (ORRELL, EVES, MASTERS, 2006; ORRELL, EVES, MASTERS, 2009).
CONCLUSION
Assessing postural balance changes in stroke-affected patients through the POMA subscale is of vital importance, as it allows for a detailed evaluation of physical performance and loss of functionality. It was also observed that single-leg standing balance was the most affected, 360-degree turning balance was the most adaptive, and sitting balance was the least affected.
REFERENCES
AN, S.; LEE, Y.; LEE, G. Validity of the performance-oriented mobility assessment in predicting falls of stroke survivors: a retrospective cohort study. Tohoku Journal of Experimental Medicine, v. 233, n. 2, p. 79-87, 2014.
ARAÚJO, A. P. S.; SILVA, P. C. F.; MOREIRA, R. C. P. S.; BONILHA, S. F. Prevalência dos fatores de risco em pacientes com acidente vascular encefálico atendidos no setor de neurologia da clínica de fisioterapia da Unipar Campus sede. Arquivo Ciência Saúde Unipar, v. 12, n. 1, p. 35-42, 2008.
BARCLAY-GODDARD, R.; STEVENSON, T.; POLUHA, W.; MOFFATT, M. E.; TABACK, S. P. Force platform feedback for standing balance training after stroke. Cochrane Database of Systematic Reviews, v. 4, CD004129, 2004 Oct 18.
BASSI, A.; COLIVICCHI, F.; SANTINI, M.; CALTAGIRONE, C. Gender-specific predictors of functional outcome after stroke rehabilitation: potential role of the autonomic nervous system. European Neurology, v. 63, n. 5, p. 279-284, 2010.
BENSOUSSAN, L.; MESURE, S.; VITON, J. M.; DELARQUE, A. Kinematic and kinetic asymmetries in hemiplegic patients’ gait initiation patterns. Journal of Rehabilitation Medicine, v. 38, n. 5, p. 287-294, 2006 Sep.
BOHANNON, R. W. Gait performance of hemiparetic stroke patients: selected variables. Archives of Physical Medicine and Rehabilitation, v. 68, n. 11, p. 777-781, 1987 nov.
CHAGAS, N. R.; MONTEIRO, A. R. M. Educação em saúde e família: o cuidado ao paciente, vítima de acidente vascular cerebral. Acta Sci Health Sci, v.26, n.1, p. 193-204, 2004.
CHENG, P. T.; WANG, C. M.; CHUNG, C. Y.; CHEN, C. L. Effects of visual feedback rhythmic weight-shift training on hemiplegic stroke patients. Clinical Rehabilitation, v. 18, n. 7, p. 747-753, 2004.
CLAYTON, K. D.; CHUMBLER, N. R.; CLARK, C. N.; YOUNG, S. N.; WILLIS, J. Patient-selected music rhythmically paired with in-patient rehabilitation: A case report on an individual with acute stroke. Physiotherapy Theory and Practice, v. 37, n. 2, p. 342-354, 2021.
CORDO, P. J.; NASHNER, L. M. Properties of postural adjustments associated with rapid arm movements. Journal of Neurophysiology, v. 47, n. 2, p. 287-302, Feb 1982.
CORRIVEAU, H.; HÉBERT, R.; RAÎCHE, M.; PRINCE, F. Evaluation of postural stability in the elderly with stroke. Archives of Physical Medicine and Rehabilitation, v. 85, n. 7, p. 1095-1101, Jul 2004.
CROSBIE, J. Postural and voluntary movement during reaching in sitting: The role of the lower limbs. Journal of Human Movement Studies, v. 28, p. 103-112, 1995.
DE OLIVEIRA, C. B.; DE MEDEIROS, I. R.; FROTA, N. A.; GRETERS, M. E.; CONFORTO, A. B. Balance control in hemiparetic stroke patients: main tools for evaluation. Journal of Rehabilitation Research and Development, v. 45, n. 8, p. 1215-1226, 2008.
DOMÍNGUEZ-CARRILLO, L. G.; ARELLANO-AGUILAR, G.; LEOS-ZIEROLD, H. Tiempo unipodal y caídas en el anciano [Unipedal stance time and fall risk in the elderly]. Cirugía y Cirujanos, v. 75, n. 2, p. 107-112, Mar-Apr 2007.
DUARTE, E.; MORALES, A.; POU, M.; AGUIRREZÁBAL, A.; AGUILAR, J. J.; ESCALADA, F. Test de control de tronco: predictor precoz del equilibrio y capacidad de marcha a los 6 meses del ictus [Trunk control test: early predictor of gait balance and capacity at 6 months after stroke]. Neurología, v. 24, n. 5, p. 297-303, Jun 2009.
FUJISAWA, H, TAKEDA, R. A new clinical test of dynamic standing balance in the frontal plane: the side-step test. Clinical Rehabilitation. v. 20, n. 4, p. 340-346, Apr 2006.
GEIGER, R. A, ALLEN J. B, O’KEEFE J, HICKS RR. Balance and mobility following stroke: effects of physical therapy interventions with and without biofeedback/forceplate training. Physical Therapy, v. 81, n. 4, p. 995-1005, Apr 2001.
GENTHON, N.., ROUGIER P., GISSOT A. S., FROGER J, PÉLISSIER J, PÉRENNOU D. Contribution of each lower limb to upright standing in stroke patients. Stroke, v. 39, n. 6, p. 1793-1799, Jun 2008.
GOMES, G. C. Tradução, adaptação cultural e exame das propriedades de medida da escala “Performance Oriented Mobility Assessment” – POMA para uma amostragem de idosos brasileiros institucionalizados [dissertação]. Campinas: Universidade Estadual de Campinas; 2003.
GRAF, A, JUDGE J. O., OUNPUU, S., THELEN, D. G. The effect of walking speed on lower-extremity joint powers among elderly adults who exhibit low physical performance. Archives of Physical Medicine and Rehabilitation, v. 86, n. 11, p. 2177-2183, Nov 2005.
HARRIS, J. E., ENG, J. J., MARIGOLD, D. S., TOKUNO C. D., LOUIS C. L. Relationship of balance and mobility to fall incidence in people with chronic stroke. Physical Therapy. v. 85, n. 2, p. 150-158, Feb 2005.
HAUER, K, PFISTERER, M, SCHULER, M, BÄRTSCH, P, OSTER, P. Two years later: a prospective long-term follow-up of a training intervention in geriatric patients with a history of severe falls. Archives of Physical Medicine and Rehabilitation. v. 84, n. 10, p. 1426-1432, Oct 2003.
HOWE, T. E, TAYLOR, I, FINN, P, JONES, H. Lateral weight transference exercises following acute stroke: a preliminary study of clinical effectiveness. Clinical Rehabilitation. v. 19, n. 1, p. 45-53, Jan 2005.
KARUKA, A. H, SILVA, J. A. M. G., NAVEGA M. T. Análise da concordância entre instrumentos de avaliação do equilíbrio corporal em idosos. Revista Brasileira de Fisioterapia. v. 15, n. 6, p. 460-466, Nov-Dez 2011.
KIM, J. H., JANG S. H., KIM, C. S., JUNG J. H., YOU, J. H. Use of virtual reality to enhance balance and ambulation in chronic stroke: a double-blind, randomized controlled study. American Journal of Physical Medicine & Rehabilitation. v. 88, n. 9, p. 693-701, Sep 2009.
KIRKER, SG, JENNER, JR, SIMPSON, DS, WING, AM. Changing patterns of postural hip muscle activity during recovery from stroke. Clinical Rehabilitation. v. 14, n. 6, p. 618-626, Dec 2000.
LISTON, RA, BROUWER, BJ. Reliability and validity of measures obtained from stroke patients using the Balance Master. Archives of Physical Medicine and Rehabilitation. v. 77, n. 5, p. 425-430, May 1996.
LIU, WJ, LIN LF, CHIANG, SL, LU LH, CHEN, CY, LIN, CH. Impacts of Stroke on Muscle Perceptions and Relationships with the Motor and Functional e v. 21, n. 14, p. 4740, Jul 2021.
LO, K, STEPHENSON, M, LOCKWOOD, C. Effectiveness of robotic assisted rehabilitation for mobility and functional ability in adult stroke patients: a systematic review. JBI Database of Systematic Reviews and Implementation Reports. v. 15, n. 12, p. 3049-3091, Dec 2017.
MANOR, B, HU K, ZHAO, P, SELIM, M, ALSOP, D, NOVAK, P, LIPSITZ, L, NOVAK, V. Altered control of postural sway following cerebral infarction: a cross-sectional analysis. Neurology. v. 74, n. 6, p. 458-464, Feb 2010.
MARCUCCI FCI, CARDOSO, NS, BERTELI, KS, GARANHANI, MR, CARDOSOS, JR. Alterações eletromiográficas dos músculos do tronco de pacientes com hemiparesia após acidente vascular encefálico. Arquivos de Neuropsiquiatria. v. 65, n. 3-B, p. 900-905, 2007.
MENEGHETTI, CHZ, DELGADO, GM, PINTO, FD, CANONICI, AP, GAINO, MRC. Equilíbrio em indivíduos com acidente vascular encefálico: Clínica Escola de Fisioterapia da Uniararas. Revista Neurociência. v. 17, n. 1, p. 14-18, 2009.
MORISHITA, M, AMIMOTO, K, MATSUDA, T, ARAI, Y, YAMADA, R, BABA, T. Analysis of dynamic sitting balance on the independence of gait in hemiparetic patients. Gait & Posture. v. 29, n. 4, p. 530-534, Jun 2009.
NICHOLS, DS. Balance retraining after stroke using force platform biofeedback. Physical Therapy. v. 77, n. 5, p. 553-558, May 1997.
ONIGBINDE, AT, AWOTIDEBE T, AWOSIKA H. Effect of 6 weeks wobble board exercises on static and dynamic balance of stroke survivors. Technology and Health Care. v. 17, n. 5-6, p. 387-392, 2009.
ORRELL, AJ, EVES, FF, MASTERS RS. Motor learning of a dynamic balancing task after stroke: implicit implications for stroke rehabilitation. Physical Therapy. v. 86, n. 3, p. 369-380, Mar 2006.
ORRELL, AJ, MASTERS RS, EVES FF. Reinvestment and movement disruption following stroke. Neurorehabilitation and Neural Repair. v. 23, n. 2, p. 177-183, Feb 2009.
PAOLUCCI, S, BRAGONI, M, COIRO, P, DE ANGELIS D, FUSCO FR, MORELLI D, VENTURIERO V, PRATESI L. Is sex a prognostic factor in stroke rehabilitation? A matched comparison. Stroke. v. 37, n. 12, p. 2989-2994, Dec 2006.
PERLMUTTER, S, LIN, F, MAKHSOUS, M. Quantitative analysis of static sitting posture in chronic stroke. Gait & Posture. v. 32, n. 1, p. 53-56, May 2010.
PETREA, RE, BEISER, AS, SESHADRI, S, KELLY-HAYES M, KASE CS, WOLF PA. Gender differences in stroke incidence and poststroke disability in the Framingham Heart Study. Stroke. v. 40, n. 4, p. 1032-1037, Apr 2009.
ROERDINK, M, GEURTS, AC, DE HAART, M, BEEK, PJ. On the relative contribution of the paretic leg to the control of posture after stroke. Neurorehabilitation and Neural Repair. v. 23, n. 3, p. 267-274, May 2009.
RYERSON, S, BYL, NN, BROWN, DA, WONG, RA, HIDLER, JM. Altered trunk position sense and its relation to balance functions in people post-stroke. Journal of Neurologic Physical Therapy. v. 32, n. 1, p. 14-20, Mar 2008.
SILVA, A, ALMEIDA, GJM, CASSILHAS, RC, COHEN, M, PECCIN, MS, TUFIK, S, MELLO MT. Equilíbrio, coordenação e agilidade de idosos submetidos à prática de exercícios físicos resistidos. Revista Brasileira de Medicina do Esporte. v. 14, n. 2, p. 88-93, Mar-Apr 2008.
SIMOCELI, L, BITTAR, RMS, BOTTINO, MA, BENTO, RF. Perfil diagnóstico do idoso portador de desequilíbrio corporal: resultados preliminares. Revista Brasileira de Otorrinolaringologia. v. 69, n. 6, p. 772-777, Nov-Dec 2003.
SLABODA, JC, BARTON, JE, MAITIN, IB, KESHNER, EA. Visual field dependence influences balance in patients with stroke. Annual International Conference of the IEEE Engineering in Medicine and Biology Society. p. 1147-1150, 2009.
TEIXEIRA-SALMELA, LF, SILVA, PC, LIMA, RCM, AUGUSTO, ACC, SOUZA ACS, GOULART F. Musculação e condicionamento aeróbio na performance funcional de hemiplégicos crônicos. Acta Fisiátrica. v. 10, n. 2, p. 54-60, 2003.
TESSEM, S, HAGSTRØM, N, FALLANG, B. Weight distribution in standing and sitting positions, and weight transfer during reaching tasks, in seated stroke subjects and healthy subjects. Physiotherapy Research International. v. 12, n. 2, p. 82-94, Jun 2007.
TYSON, SF, HANLEY, M, CHILLALA, J, SELLEY, A, TALLIS, RC. Balance disability after stroke. Physical Therapy. v. 86, n. 1, p. 30-38, Jan 2006.
VAN CRIEKINGE, T, HALLEMANS, A, HERSSENS, N, LAFOSSE, C, CLAES, D, DE HERTOGH, W, TRUIJEN, S, SAEYS, W. SWEAT2 Study: Effectiveness of Trunk Training on Gait and Trunk Kinematics After Stroke: A Randomized Controlled Trial. Physical Therapy. v. 100, n. 9, p. 1568-1581, Aug 2020.
VARAS-DIAZ, G, CORDO, P, DUSANE, S, BHATT, T. Effect of robotic-assisted ankle training on gait in stroke participants: A case series study. Physiotherapy Theory and Practice. v. 38, n. 13, p. 2973-2982, Nov 2022.
VERHEYDEN, G, NIEUWBOER, A, DE WIT, L, THIJS, V, DOBBELAERE, J, DEVOS H, SEVERIJNS D, VANBEVEREN S, DE WEERDT W. Time course of trunk, arm, leg, and functional recovery after ischemic stroke. Neurorehabilitation and Neural Repair. v. 22, n. 2, p. 173-179, Mar-Apr 2008.
VERHEYDEN, G, VEREECK, L, TRUIJEN, S, TROCH, M, LAFOSSE, C, SAEYS, W, LEENAERTS, E, PALINCKX, A, DE WEERDT, W. Additional exercises improve trunk performance after stroke: a pilot randomized controlled trial. Neurorehabilitation and Neural Repair. v. 23, n. 3, p. 281-286, May 2009.
APPENDIX
Poma-Brasil Application Recommendations Protocol.
Individuals should be tested in a well-lit environment with non-slip floors, preferably in the presence of handrails. The test begins with the individual seated in a chair with a seat height of 45 cm, without armrests and with a straight backrest, and a non-slippery seat. They should sit upright without leaning.
Sitting balance: This maneuver should take about five seconds so that those who have instability have a chance to demonstrate it.
Chair rise: The task of rising from the chair should be performed with the recommendation that, if possible, the upper limbs should not be used. When the individual uses their hands on the lower limbs to rise, even slightly, the response should be adaptive.
Standing balance: The evaluator should stand close to the individual’s side without showing signs of support. Care should be taken for possible dizziness due to low blood pressure levels. The tested individual’s feet should remain together as closely as possible.
Standing balance and eyes closed balance: Observe if there is no arm opening as a sign of instability or if there is excessive oscillation. The procedure should last approximately five seconds.
360-degree turning balance: The evaluator should stand nearby without showing signs of support. Care should be taken for possible dizziness due to vestibular issues.
Nudge Test: The tested individual should not receive any information about the procedure to prevent anticipatory adjustments. These adjustments are common in the elderly and physiological responses that inhibit an instability response. The maneuver is performed with two to three firm pressures, using the palm of the evaluator’s fingers on the tested individual’s sternum to destabilize their orthostatic balance. The evaluator should stay beside the tested individual to ensure their stability.
Neck rotation: The individual is asked to rotate the neck and lift the head. This is done by asking the individual to follow the movement of a pen in the evaluator’s hand, which remains in front of them.
Single-leg support: The individual is asked to stand on one leg and lift the other foot to the height of the opposite knee. They can use either leg, as this allows them to use the leg they are most confident with.
Spine extension: The tested individual is asked to look up and back toward the ceiling, leaning the spine. The evaluator should stand beside the tested individual to ensure their stability. The spine extension task receives a higher score when it shows an angle greater than 20°, estimated visually.
Reach upwards: In the task of upper reach, the individual is asked to stand on tiptoes and not just stretch to reach the object. If the task is only performed with stretching, the individual receives a medium response grade. This task involves asking the individual to reach for an object, such as a pen, raised to a height that exceeds their standing height with the arm extended.
Lean forward: The task of leaning forward is done by asking the individual to pick up a pen placed on the floor in front of them, a few centimeters from the front edges of the feet (hallux). Their base of support should be hip-width, with no increase or decrease.
Sitting: The individual is allowed to perform the task as they see fit. However, it is common for them to use their hands to increase their safety, as the chair is behind them. This behavior should not be considered as instability; only the smoothness of the movement should be evaluated.
[1] Master’s in Health and Environment and Assistant Professor at Faculdade São Luis de França. ORCID: https://orcid.org/0000-0002-6965-9984. Lattes Curriculum: http://lattes.cnpq.br/4050256889155260.
[2] Medical Clinic Resident. ORCID: https://orcid.org/0000-0002-5298-537X. Lattes Curriculum: http://lattes.cnpq.br/6291628187714859.
[3] Medical Clinic Resident. ORCID: https://orcid.org/0000-0001-9211-7000. Lattes Curriculum: http://lattes.cnpq.br/4619345212343744.
[4] Full Professor of Molecular Biology. ORCID: https://orcid.org/0000-0001-5705-6433. Lattes Curriculum: http://lattes.cnpq.br/3337321488338686.
[5] Full Professor at the School of Medicine. ORCID: https://orcid.org/0000-0002-7776-1831. Lattes Curriculum: http://lattes.cnpq.br/6858508576490184.
[6] Advisor. Full Professor of Clinical Anatomy. ORCID: https://orcid.org/0000-0002-2300-3330. Lattes Curriculum: http://lattes.cnpq.br/6911783083973582.
Sent: April 18, 2023.
Approved: June 27, 2023.
















