REVIEW ARTICLE
LOPES, Luiz Thiago Oliveira [1], OLIVEIRA, Marcelus de Andrade [2], GONÇALVES, Willian Guilherme Lobato [3], DAHER, Donizete Vago [4], BRITO, Irma da Silva [5], DENDASCK, Carla Viana [6], DIAS, Cláudio Alberto Gellis de Mattos [7], FECURY, Amanda Alves [8], ARAÚJO, Maria Helena Mendonça de [9]
LOPES, Luiz Thiago Oliveira. et al. Sequels of COVID-19: An integrative literature review. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year 08, Ed. 08, Vol. 01, pp. 68-87. August 2023. ISSN: 2448-0959, Access link: https://www.nucleodoconhecimento.com.br/health/sequels-of-covid-19, DOI: 10.32749/nucleodoconhecimento.com.br/health/sequels-of-covid-19
ABSTRACT
The strong affinity between the Spike protein of the SARS-CoV-2 virus and the angiotensin-converting enzyme 2 receptor is postulated as one of the main reasons for the high viral transmission rate, leading the WHO to declare COVID-19 as a Public Health Emergency of International Concern and to adopt measures to contain viral spread. Moreover, due to the virus’s pathophysiological mechanism, non-specific symptoms, atypical progression, especially in the elderly and immunocompromised, and a faster and more lethal progression are observed. Additionally, as knowledge about the natural history of the virus infection has advanced, persistent symptoms and/or sequelae causing organic dysfunctions and negatively impacting patients’ quality of life have been noted. In light of this, the objective of this article was to present an integrative review of the main sequels of COVID-19 in the years 2021 and 2022. To achieve this, full articles were searched in the Scientific Electronic Library Online, Biblioteca Virtual em Saúde, and PubMed research databases, in both Portuguese and English languages, using the PRISMA methodology (Preferred Reporting Items for Systematic Reviews and Meta-Analyses), resulting in the selection of 14 articles. Among the results, the following stand out: the pathogenesis of persistent COVID-19 is based on the theory of immune phenomena secondary to infection, abnormal immune response, and the presence of the virus in immunologically privileged sites; prevalent complications include fatigue, dyspnea, subjective cognitive impairment, neurological sequelae, central nervous system inflammatory diseases, and post-viral olfactory dysfunction; evidence of a causal relationship between COVID-19 and subacute thyroiditis was presented; a higher number of complications and hospitalizations were demonstrated in vitamin D-deficient patients; as well as the presence of neuropsychiatric symptoms in the healthcare professional population. In conclusion, a scarcity of studies directly addressing COVID-19 sequelae was noted, highlighting the need for further research to create more specific diagnostic protocols.
Keywords: SARS-CoV-2, COVID-19, Sequels and Rehabilitation, Post-COVID-19 Syndrome.
1. INTRODUCTION
Viruses rely on the infrastructure and metabolism of the host cell throughout their replication cycle, particularly the cytoskeleton and the cell membrane (CORTINES, 2019). They utilize, to varying degrees, the cell’s synthesis system, leading to the transfer of the viral genome to others. Viruses are composed, at least, of a nucleic acid genome, either RNA or DNA, and a protein coat. Many of them have an additional outer membrane called an envelope (ANDINO, 2017; MAERTENS, 2022).
Viral transmission occurs indirectly through contact with secretions/excretions from an infected animal or directly through mechanical or biological vectors. There is also a vertical transmission (colostrum, perinatal, or transplacental) from the mother to the offspring. The other forms are referred to as horizontal transmission (ANDINO, 2017; LI, 2022).
The virus reproduction process involves mechanisms of adhesion, penetration, and viral uncoating; synthesis of polyproteins, genomic replication, assembly, and exocytosis of new virions (DE ALMEIDA et al., 2020).
Regarding the SARS-CoV-2 virus, the replicative cycle begins with the interaction of the Spike glycoprotein, located on the viral envelope, with the cellular receptor Angiotensin-Converting Enzyme 2 (ACE2) present on the surface of the target cell. This interaction is responsible for the virus tropism towards the host cell, leading to its adhesion (DE ALMEIDA et al., 2020; LAMERS, 2022).
Based on evidence, it is postulated that SARS-CoV-2 infection can start in the upper respiratory tract, such as the nasal epithelium. Thus, the endocytosis pathways, associated with viral adhesion and penetration steps, will depend on the expression of endocytic proteins, such as GTPase (abundant in the nasal epithelium), and proteins involved in macropinocytosis (present in pneumocytes) (LAMERS, 2022; GONZALEZ et al., 2023).
SARS-CoV-2 can be classified as a virus belonging to the Coronaviridae family and the betacoronavirus group, similar to MERS (Middle East Respiratory Syndrome) and SARS (Severe Acute Respiratory Syndrome), responsible for causing an acute respiratory disease known as COVID-19 (OMS, 2022).
Given the widespread distribution of ACE2 in multiple organs, there is a possible reason for the high transmission rate of SARS-CoV-2, which spread to almost all continents, leading to the World Health Organization (WHO) declaring it a Public Health Emergency of International Concern (PHEIC) on January 30, 2020 (YESUDHAS et al., 2021).
Following this point, there was a need to adhere to measures to contain viral spread. Thus, the main measures adopted were personal distancing of at least one meter, the use of personal protective masks, and the isolation of infected individuals. Additionally, the WHO provides basic rules to follow to avoid contagion, emphasizing points such as avoiding closed spaces and large gatherings, hand hygiene with soap and water or alcohol, and avoiding touching eyes, mouth, and nose (OMS, 2022).
In line with the mentioned pathophysiological mechanism, it is possible to observe that the presented symptoms result from an inflammatory process affecting the endothelium of various organs. The exaggerated release of pro-inflammatory cytokines such as interleukins 1 and 6 (IL-1 and IL-6) and interferon-α (TNF-α) causes damage to endothelial functions, resulting in thrombosis, fluid extravasation, and loss of the pulmonary, hepatic, renal, cardiac, and central nervous system endothelial barrier (LIBBY, 2020).
Most infected individuals will have mild presentations of the disease, with symptoms such as fever, malaise, mild shortness of breath, fatigue, myalgia, cough, sore throat, headache, nasal congestion, diarrhea, nausea, and vomiting. On the other hand, vulnerable patients, such as immunocompromised and elderly individuals, may have an atypical condition with a rapid and severe progression, potentially leading to death. Thus, the main symptoms are characteristic of an Influenza-like Illness (ILI); however, when there is progression to a severe syndrome, it is termed Severe Acute Respiratory Syndrome (SARS), characterized by dyspnea/respiratory distress or persistent chest pressure or O2 saturation less than 95% in ambient air or cyanosis in lips and face (ISER et al., 2020).
As knowledge about the natural history of SARS-CoV-2 infection has advanced, systemic involvement sequelae have been observed, characterized by modifications in the functioning and/or form of cells and/or organs, resulting in permanent or non-permanent dysfunctions in the individual (CHAVES et al., 2021).
In this regard, sequelae in the Central Nervous System (CNS) have already been observed, manifested as behavioral changes, anosmia, and an increased incidence of stroke. In the cardiovascular system, there are reports of acute cardiac injury, myocarditis, vascular inflammation, arrhythmias, as well as elevation of cardiac enzymes associated with systemic or localized inflammatory response in arterial plaques. In the liver, hepatic failure and microvascular steatosis can occur. In the kidneys, possibilities of tubular necrosis and renal failure. Coagulation disorders, such as thrombotic alterations, an increased likelihood of severe thrombocytopenia, and disseminated intravascular coagulation, can also be found (CAMPOS et al., 2020).
The study of post-acute infection indicates that persistent symptoms and/or sequelae may manifest differently, depending on the severity of the acute condition, showing differences between patients who were hospitalized in the Intensive Care Unit (ICU) and those outside the ICU (ALBU et al., 2021).
2. OBJECTIVE
To present an integrative literature review, covering the years 2021 and 2022, on the main sequelae of COVID-19.
3. METHOD
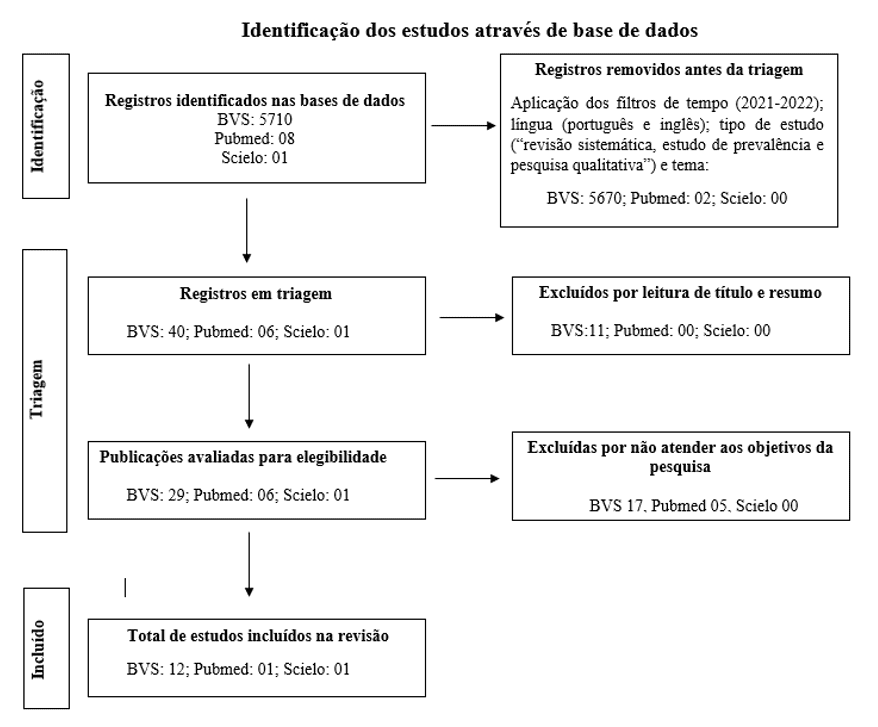
An integrative literature review was carried out on the sequelae of COVID-19, in the research databases Scientific Electronic Library Online – SciELO, Biblioteca Virtual em Saúde-VHL and PubMed. To achieve this, initially, on October 19, 2022, the health descriptors “SARS-CoV-2”, “COVID-19” and “Sequelas e Reabilitação” were used, joined by the logical connector “AND”. Furthermore, time filters were applied, setting the publication period between 2021 and 2022; language, for publications in Portuguese and English; and type of study, with which articles from “Systematic Review”, “Prevalence Study” and “Qualitative Research” were selected.
At the end of these stages, 23 articles were obtained from the VHL, 03 articles from PubMed and 01 article from SciELO. Finally, an article selection stage was carried out with the inclusion criteria being articles that were available in full and that corresponded to the research objectives and the exclusion criteria being articles that were incomplete or that did not meet the objective. Thus, 06 articles remained in the VHL, and 01 in SciELO.
In a second stage, on December 8, 2022, a new search was carried out, this time using the descriptor “Post-COVID-19 Syndrome”, repeating all the steps previously described. At the end of this stage, 06 articles were added to the VHL and 01 to PubMed, totaling the sample space for the integrative review of 14 articles.
Finally, on December 28, 2022, with the aim of better systematizing the choice of articles for this review, the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) methodology was used. This methodology provides a flowchart (Figure 1) in three stages: “Identification”, “Screening” and “Included”, where in each of them the number of excluded articles in each database is recorded, and those that will continue for the subsequent stage of analysis until the final quantity that will be used in the review.
In the “Identification” stage, time, language, type of study and topic filters were applied. In the “Triage”, publications were excluded after reading the title and abstract and, after reading the full text, publications that did not meet the research objectives. The “Included” stage consolidates the total number of articles, in each database, to be worked on in the review (MOHER et al., 2009).
Figure 1: PRISMA flowchart, from the research carried out on October 19, 2022 and December 8, 2022
4. RESULTS
The main results related to the pathophysiology of persistent COVID-19 are based on the theory of immunological phenomena secondary to infection, abnormal immune response and the presence of viruses in immunologically privileged locations.
The prevalent complications were fatigue, dyspnea, subjective cognitive impairment, neurological sequelae, Post-viral Olfactory Dysfunction (PVOD), inflammatory diseases of the CNS (encephalitis, meningoencephalitis or encephalomyelitis) with clinical presentations different from their classic forms and symptoms of anxiety, insomnia and depression in the population of health professionals.
Adding to this, evidence of a causal relationship between COVID-19 and Subacute Thyroiditis (SAT) was found. Furthermore, SARS-CoV-2 shows signs of having the capacity to trigger a greater number of complications and hospitalizations in patients with vitamin D deficiency. Such findings were summarized in Table 01 together with the methods and conclusions obtained in the articles selected for this review.
Table1. Summary of results found in articles selected in 2021 and 2022
| AUTHOR, YEAR | TYPE OF METHOD | RESULTS | CONCLUSION |
| MARTÍN-GARRIDO, 2022 | Systematic review | Meta-analysis with 47,910 patients, included 15 publications until 01/01/2021. 55 long-term effects detected: 80% (95% CI: 65-92%) of those infected developed one or more long-term symptoms: fatigue (58%), headache (44%), difficulty paying attention (27% ), hair loss (25%) and dyspnea (24%). | The quality of evidence from the studies included in this review is low, with a high risk of bias and extensive heterogeneity in terms of disease prevalence. Furthermore, its external validity is very limited, with no control groups and limited studies including children. There is a need to carry out new controlled prospective cohort studies that include different populations and risk contexts. |
| ALBU et al., 2021 | Single-Center Cross-Sectional Observational Study | Patients with fatigue (86.6%), dyspnea (66.7%), subjective cognitive impairment (46.7%) and neurological sequelae (33.3%). Post-ICU presented sequelae of critical illness myopathy and polyneuropathy, stroke and encephalopathy and lower forced vital capacity compared to non-ICU patients. Cognitive impairment in 63.3% of patients. | The variability of post-COVID19 physical and neuropsychological impairment requires a complex triage process for ICU and non-ICU patients. The high impact of persistent symptoms on activities of daily living and quality of life indicates the need for rehabilitation. |
| KOZATO et al., 2021 | Case report | Symptoms of respiratory failure before developing psychotic symptoms (paranoid thoughts with auditory and tactile hallucinations). | The Case demonstrates the importance of early identification and treatment of neuropsychiatric complications resulting from COVID-19 within a hospital environment. There is a need for research in this area to help prevent and treat these complications. |
| FONTES et al., 2022 | Telephone consultation with 99 survivors. The questionnaires were applied: EuroQol Five-Dimensional Five-Level and World Health Disability Assessment Schedule 2.0 – 12 items. | Population studied with an average age of 63 years. The average EuroQol Visual Analogue Scale was 65%, with only 35.3% of survivors having no or no problems carrying out their usual activities. The World Health Disability Assessment Schedule 2.0 – 12 items, showed a marked inability to resume usual work or community activities and mobility. | The use of both tools suggested that the health status of survivors would be worse than their perception.
Early identification of sequelae can help define flows and priorities for rehabilitation and reintegration after severe COVID-19. |
| CÉNAT et al., 2021 | Meta-analysis | Most studies were carried out in China (k = 45) and in the general population (k = 41), the remainder were in other countries and in healthcare professionals, respectively. The data allowed comparisons between the general population and healthcare professionals for all mental health symptoms and for comparisons between genders (male and female) and geographic regions (China and other countries) for depression and anxiety. The prevalence of depression (15.97%), anxiety (15.15%), insomnia (23.87%), post-traumatic stress disorder (21.94%), psychological distress (13.29%). Differences between groups were found only in healthcare professionals (z = 2.69, p < 0.05) who had a higher prevalence of insomnia than others. | The results suggest that the short-term mental health consequences of COVID-19 are equally high across affected countries and across genders. However, reports of insomnia are significantly higher among healthcare professionals than in the general population. |
| SOUSA et al., 2022 | Systematic Literature Review | The prevalence of sequelae were: depression (27.5%), anxiety and insomnia (35.8%) and stress (51.9%). In three of the included studies, healthcare professionals reported post-traumatic stress, somatization, and obsessive-compulsive symptoms. | The COVID-19 pandemic has a significant psychological impact on healthcare professionals, with significant prevalence of depression, anxiety, insomnia and stress. |
| ALEMANNO et al., 2021 | Cross-sectional, quantitative study using a questionnaire | Of the 87 patients, 80% had neuropsychological deficits and 40% had mild to moderate depression. Impairment of visuospatial/executive functions, naming, short and long-term memory, abstraction and orientation were evident. Cognitive impairments correlated with the age of the patients. | Patients with severe functional impairments had significant cognitive and emotional deficits that are mainly related to aging. These findings must be integrated for the correct neuropsychiatric care of patients with COVID-19 in the subacute phase of the disease and show the need for psychological support and long-term treatment for post-COVID-19 patients. |
| ZAMANI et al., 2022 | Systematic review | 26 patients were diagnosed with meningoencephalitis. Neck stiffness and photophobia were described in 4 patients. Declining consciousness was the most common clinical finding, including 6 cases of delayed recovery of consciousness post-sedation. 11 cases of acute hemorrhagic leukoencephalitis were found, with associated seizures and dysautonomia. 12 patients were diagnosed with acute necrotizing encephalitis, including 5 cases with hemorrhage. A total of 49 studies reported 109 patients with encephalitis in the context of SARS-CoV-2 infection. Of the total of 109 patients, 12 cases with encephalitis were suspected of autoimmune encephalitis, of which 7 were confirmed. Cognitive, psychiatric, consciousness and motor disorders were the most frequent neurological presentations, followed by cranial nerve deficits and seizures. | Our pooled evidence suggests that Covid-19-related encephalitis presents with a delayed presentation of mainly psychiatric, consciousness, motor and/or cranial symptoms.
Acute demyelinating, hemorrhagic or necrotizing cephalopathies are frequently reported in adults with Covid-19 and should be considered in the management of neuro Covid patients. It is crucial to develop comprehensive guidelines and considerations to address neuroinflammation in the context of Covid-19, tracking and evaluating in recovered patients months and years after infection. |
| ZELADA-RIOS et al., 2021 | Systematic Review and Case Report | Seven cases (77.8%) with moderate/severe acute disseminated encephalomyelitis. Other neurological findings were pyramidal signs (44.4%), brainstem signs (11.1%), cerebellar signs (22.2%), seizures (33.3%) and peripheral nerve involvement (11.1% ).
In adults, 73.68% were men (14 cases). The average number of days from COVID-19 infection to ADEM diagnosis was 23.2 days (4 to 60 days). Regarding COVID-19 symptoms, 66.7% were severe, 22.2% were mild and 11.1% were asymptomatic. |
The clinical and neuroimaging presentation of ADEM was similar to pre-COVID-19 reports, but with more frequent severe cases and some demographic changes due to the influence of ADEM epidemiology.
COVID 19 (elderly and men). No association was found between the severity of COVID-19 and the severity of ADEM at hospitalization. The recovery rate was very low in adults but high in children. |
| MANZANO et al., 2021 | Systematic review | Forty-six patients (28 men, median age 49.5 years, 1/3 >50 years) were analyzed, derived from 26 case reports or series from 8 countries together with 4 patient cases from the authors’ hospital files. COVID-19 infection was laboratory confirmed in 91% of cases, and the severity of the infection required intensive care in 67%. ADEM occurred in 31 cases, while AHLE occurred in 15. | In contrast to ADEM and AHLE cases from the pre-pandemic era, post-COVID-19 reports generally showed older age at onset, severe antecedent infection, high hemorrhage on neuroimaging, neurological impairments, and high mortality rate. Results are limited by nonstandardized case reporting, truncated follow-up information, and presumed publication bias. |
| WANG et al., 2022 | Systematic review | A total of 48 COVID-19 patients diagnosed with ADEM/AHLE were used for analyzes of the 37 case reports and case series published between December 1, 2019 and June 5, 2020. | In conclusion, the clinical picture of ADEM associated with COVID-19 was shown and it was revealed that this association is rare. SARS-CoV-2 – ADEM appears to share most of the symptoms of classic ADEM, with moderate discrepancies. |
| ZHANG et al., 2021 | Systematic Review and Meta Analysis | Since post-viral olfactory dysfunction is the most common cause of smell disorders and since coronaviruses are one of many pathogens, it is reasonable to consider smell disorders in COVID-19 as a classification of PDO. | The study attempted to provide evidence to prove the effectiveness and safety of olfactory training in patients with smell disorders related to COVID-19, and a continuation of the study is necessary for this objective. |
| CHRISTENSEN et al., 2022 | Short narrative systematic review | 17 cases of subacute thyroiditis (SAT) associated with COVID-19 were found in 15 publications. The most common clinical features were: neck pain and tenderness (13/17; 82%) and tachycardia (8/17; 47%). | It is important to consider subacute thyroiditis in those with COVID-19 and order thyroid function testing in this setting. |
| AFAGHI et al., 2021 | Retrospective cohort study | Cases over 60 years old were 6.2 times more likely to die from COVID-19, compared to younger people. Male patients were approximately 2 times more likely to die from the disease than female patients. The low level of vitamin D indicated that vitamin D deficiency had approximately 3.3 times greater chance of death. | Low vitamin D independently increased the risk of mortality in patients hospitalized with COVID-19. |
Source: authors, 2022.
5. DISCUSSION
According to Martín-Garrido (2022), persistent COVID-19 or Long COVID-19 Syndrome is defined as the presence of signs and symptoms that continue or develop after acute COVID-19 and is a significant finding that affects different organs and body systems. According to the aforementioned author, it is postulated that the explanation of pathophysiogenesis is based on three theories: immunological phenomena secondary to infection, abnormal immunological response and the presence of viruses in privileged locations.
Regarding immunological phenomena secondary to infection and abnormal immune response, the term “cytokine storm” has been used to describe the high level of inflammatory cytokines present in patients with severe COVID-19. This inflammatory state can both worsen pre-existing conditions and cause new ones, leading to the consequences of COVID-19 (BRITISH SOCIETY FOR IMMUNOLOGY, 2020).
Regarding the presence of viruses in privileged locations, SARS-CoV-2 can cause long-term problems through direct tissue damage, generating fibrosis, or through collateral damage due to excess inflammation or the consequence of thrombotic complications (BRITISH SOCIETY FOR IMMUNOLOGY, 2020). In this way, the theories mentioned about pathophysiogenesis are in line with what was presented by Gárcia-Salido (2020).
Martín-Garrido (2022) shows that in a group aged between 17 and 87 years, the five most common symptoms were fatigue (58%), headache (44%), difficulty paying attention (27%), hair loss (25%) and dyspnea (24%). Albu et al. (2021), in addition to the findings found by Martín-Garrido (2022), demonstrated a higher prevalence of fatigue (86.6%), dyspnea (66.7%), subjective cognitive impairment (46.7%) and neurological sequelae ( 33.3%) in patients infected with the COVID-19 virus.
The most frequent sequel was fatigue, cited both by Martín-Garrido (2022) and Albu et al. (2021). One of the possible explanations would be the severity of the clinical condition, the cytokine storm in the acute phase and the medications used, such as corticosteroids (LAM et al., 2009). Another result would be that this sequel directly impacts quality of life, mainly by influencing physical and cognitive activities that are essential in everyday life (CEBAN et al., 2022). Finally, fatigue is one of the main influencers of psychological complications, according to Albu et al. (2021).
Regarding psychological disorders, Kozato et al. (2021) documented the case of a man with no prior history of any psychiatric disorder, but with type 2 diabetes mellitus, systemic arterial hypertension, non-alcoholic fatty liver disease, smoking and alcoholism in the past, who, after acquiring the COVID-19 infection, needed to stay 8 days in the ICU and developed panic attacks, insomnia, auditory and tactile hallucinations.
Regardless of gender, group or region, there was a high prevalence of depression, anxiety, insomnia and psychiatric disorders (KULAGA, 2021; FONTES et al., 2022; CÉNAT et al., 2021). However, neuropsychiatric symptoms can be triggered by several microorganisms in addition to COVID-19.
According to Sousa et al. (2022), the presence of isolated or concomitant symptoms of depression, anxiety, insomnia, stress and post-COVID-19 somatization in healthcare professionals is notable. These data are supported by the study carried out by Pappa et al. (2020) in which these symptoms were the main complications found in these professionals during the COVID-19 pandemic. Therefore, this is a population particularly vulnerable to psychiatric disorders, as they are directly involved in the diagnosis and management of patients, being placed under extreme demands that threaten professional resilience.
In the review by Alemanno et al. (2021), when investigating the impact of COVID-19 on the cognitive functions of hospitalized patients and using neuropsychological assessment instruments such as the Mini Mental State Examination (MMSE), Montreal Cognitive Assessment (MoCA) and Hamilton Rating Scale for Depression (HRSD), a correlation was observed between cognitive impairments and age, with severity being greater in older patients.
Changes were observed in the visuospatial/executive domains, naming, short and long-term memory, abstraction, orientation, depression and anosmia, however, according to Schou et al. (2021), it is unclear whether early cognitive deficits are related to the long-term effects of COVID-19.
Regarding sequelae related to the CNS, Zamani et al. (2022) aimed to determine the profile and possible mechanisms for triggering inflammatory diseases in the context of COVID-19, namely: immune-mediated inflammation with migration of inflammatory agents to the CNS; intrathecal or systemic synthesis of autoantibodies resulting from molecular mimicry/immunological hyperactivity; direct hematogenous viral invasion by disruption of the blood-brain barrier; direct neuronal invasion via the cribriform plate/bulb or other cranial nerves, this mechanism having a direct relationship with olfactory involvement.
These pathophysiological mechanisms explain the results found by Zelada-rios et al. (2021), who described and qualitatively evaluated the relationship between Acute Disseminated Encephalomyelitis (ADEM) and COVID-19, relating the degree of severity of the infection with the outcomes. In general, classic ADEM has a higher incidence in children, however in cases preceded by SARS-COV-2 infection there was a predominance of the adult population.
This discrepancy would be a consequence of children’s lower propensity for infection, as well as the development of asymptomatic or mild disease. In any case, the percentage of pediatric cases, 30% of the total, suggests the need for neurological monitoring in the post-COVID-19 evaluation of children. As for the adult public, it was found that the average age was around 50 years old, when in the classic ADEM it would be between 33 and 41 years old (Zelada-Rios et al., 2021), this fact was explained by the higher frequency of cases of COVID-19 in the elderly population and the influence of infection severity on the development of ADEM.
Furthermore, Manzano et al. (2021) found a relationship between the development of ADEM and Acute Hemorrhagic Leukoencephalitis (AHLE) after SARS-COV-2 infection. Thus, with respect to time, the development of ADEM and AHLE occurred within 15 to 30 days, with encephalopathy (confusion, lethargy and difficulty waking up after sedation), focal motor, focal sensory, cranial, cerebellar and of seizure the main neurological signs and symptoms.
Thus, it was evidenced that post-COVID-19 ADEM cases share several symptoms of the classic model, with the following differences: onset of COVID-19 and ADEM symptoms (25 days post-COVID-19 and 7-14 days in the classic), more advanced age distribution of patients (median of 44 years in post-COVID-19 and more commonly in children in the classic), lower recovery rate, distribution of the most frequent brain lesions in the periventricular white matter and corpus callosum and lower frequency of lesions in the deep substantia nigra (MANZANO et al., 2021; WANG et al., 2022; ZELADA-RIOS et al., 2021).
Zhang et al. (2021) identified the main mechanisms of smell disturbances in SARS-COV-2 infection: olfactory cleft syndrome with mucosal obstruction, post-viral anosmia syndrome, cytokine storm and impairment of sense due to direct damage to olfactory neurons and /or impaired perception in the smell center of the brain. Furthermore, as the coronavirus is one of the many pathogens that cause Post Viral Olfactory Dysfunction (PVOD) and given the strong impact of anosmia on patients’ quality of life, it is necessary to establish a protocol for its treatment, as was also said by Chaves et al. (2021).
The study by Christensen et al. (2022) demonstrated the causal relationship between COVID-19 and subacute thyroiditis (SAT). The clinical characteristics found in SAT were varied and general, such as palpitations, anxiety, heat intolerance, insomnia, weight loss, agitation, irregular menstruation, fever, asthenia, tremors, hyperreflexia and goiter. The lack of specificity of the clinical picture makes diagnosis difficult in the initial course of COVID-19, corroborating the findings that 16 of the 17 cases found by Christensen et al. (2022) were diagnosed at times when the patient no longer had respiratory symptoms, much less Systemic Inflammatory Response Syndrome (SIRS). In this case, the mechanism of how SAT is triggered by the Sars-Cov-2 virus is not yet known.
Lastly, Siamak et al. (2021) presented satisfactory results on the relationship between low levels of vitamin D and worsening of COVID-19 infection. In this study, patients were divided into groups of vitamin D deficiency, insufficiency and sufficiency. A greater number of complications and length of stay were found in patients with vitamin D deficiency. Furthermore, 46.8% of deficient patients died, compared to 29.4% of those who were insufficient and 5.5% of those who were sufficient. These data support the understanding that higher serum concentrations of vitamin D are associated with reduced risk and severity of COVID-19 (MERCOLA et al., 2020). However, it has not been proven that deficiency of this vitamin can occur as a sequelae of COVID-19.
6. CONCLUSION
The sequelae of COVID-19 are disorders generated by the SARS-CoV-2 virus that remain for a long time even after the infectious condition has resolved, affecting patients’ lives and their daily tasks.
Fatigue and dyspnea were the most cited sequelae in the studies evaluated. However, others may be evident, such as psychological and neurological disorders. This variety of sequelae and severity, regardless of the course of the infection, demonstrates the need for a thorough evaluation within a specific rehabilitation center.
Furthermore, there is evidence that there are factors that can worsen the disease and increase the chances of complications, such as vitamin D deficiency, which is an object of analysis for future studies.
Therefore, the development of new scientific research is necessary to specify the sequelae and deepen knowledge about them, understanding their behavior over the years. This practice should aim to create effective protocols for diagnosing patients who acquired COVID-19 and were left with sequelae.
REFERENCES
AFAGHI, Siamak et al. Prevalence and clinical outcomes of vitamin D deficiency in COVID-19 hospitalized patients: a retrospective single-center analysis. The Tohoku Journal of Experimental Medicine, v. 255, n. 2, p. 127-134, 2021.
ALBU, Sergiu et al. What’s going on following acute covid-19? Clinical characteristics of patients in an out-patient rehabilitation program. NeuroRehabilitation, v. 48, n. 4, p. 469-480, 2021.
ALEMANNO, Federica et al. COVID-19 cognitive deficits after respiratory assistance in the subacute phase: A COVID-rehabilitation unit experience. Plos one, v. 16, n. 2, p. e0246590, 2021.
ANDINO, Raul; DIAMOND, Michael. Editorial overview: Viral pathogenesis: Strategies for virus survival—Acute versus persistent infections. Current Opinion in Virology, v. 23, p. v, 2017.
British Society for Immunology. Long-term immunological health consequences of COVID-19, 2020 [acesso em 12 junho de 2023]. Disponível em: https://www.immunology.org/coronavirus/immunology-and-covid-19/report-long-term-immunological-health-consequences-covid-19
CAMPOS, Mônica Rodrigues et al. Burden of disease from COVID-19 and its acute and chronic complications: reflections on measurement (DALYs) and prospects for the Brazilian Unified National Health System. Cadernos de Saúde Pública, v. 36, 2020.
CEBAN, Felicia et al. Fatigue and cognitive impairment in post-COVID-19 Syndrome: A systematic review and meta-analysis. Brain, behavior, and immunity, v. 101, p. 93-135, 2022.
CÉNAT, Jude Mary et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry research, v. 295, p. 113599, 2021.
CHAVES, Ieda Bezerra et al. Sequelas do COVID 19 em gustação e olfato: uma breve revisão bibliográfica. Revista Científica Multidisciplinar Núcleo do Conhecimento. Ano. 06, Ed. 11, Vol. 01, pp. 150-166. Novembro 2021.
CHRISTENSEN, Jacob et al. Risk factors, treatment, and outcomes of subacute thyroiditis secondary to COVID‐19: a systematic review. Internal Medicine Journal, v. 52, n. 4, p. 522-529, 2022.
CORTINES, Juliana Reis; PREVELIGE JR, Peter. Editorial overview: Virus structure and expression. Current opinion in virology, v. 36, p. iii-v, 2019.
DE ALMEIDA, J. O. et al. COVID-19: Fisiopatologia e alvos para intervenção terapêutica. Rev. Virtual Quim. ISSN, v. 12, n. 6, p. 1464-1497, 2020.
FONTES, Liliana Cristina da Silva Ferreira et al. Impacto da COVID-19 grave na qualidade de vida relacionada com a saúde e a incapacidade: uma perspectiva de follow-up a curto-prazo. Revista Brasileira de Terapia Intensiva, v. 34, p. 141-146, 2022.
GARCÍA-SALIDO, Alberto. Revisión narrativa sobre la respuesta inmunitaria frente a coronavirus: descripción general, aplicabilidad para SARS-COV-2 e implicaciones terapéuticas. In: Anales de Pediatría. Elsevier Doyma, 2020. p. 60. e1-60. e7.
GONZALEZ-GARCIA, Pablo et al. From Cell to Symptoms: The Role of SARS-CoV-2 Cytopathic Effects in the Pathogenesis of COVID-19 and Long COVID. International Journal of Molecular Sciences, v. 24, n. 9, p. 8290, 2023.
ISER, Betine Pinto Moehlecke et al. Definição de caso suspeito da COVID-19: uma revisão narrativa dos sinais e sintomas mais frequentes entre os casos confirmados. Epidemiologia e Serviços de Saúde, v. 29, 2020.
KOZATO, Nana; MISHRA, Monisha; FIRDOSI, Mudasir. New-onset psychosis due to COVID-19. BMJ Case Reports CP, v. 14, n. 4, p. e242538, 2021.
KULAGA, Stephanie S.; MILLER, Christopher WT. Viral respiratory infections and psychosis: a review of the literature and the implications of COVID-19. Neuroscience & Biobehavioral Reviews, v. 127, p. 520-530, 2021.
LAM, Marco Ho-Bun et al. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: long-term follow-up. Archives of internal medicine, v. 169, n. 22, p. 2142-2147, 2009.
LAMERS, Mart M.; HAAGMANS, Bart L. SARS-CoV-2 pathogenesis. Nature reviews microbiology, v. 20, n. 5, p. 270-284, 2022.
LI, Na; RANA, Tariq M. Regulation of antiviral innate immunity by chemical modification of viral RNA. Wiley Interdisciplinary Reviews: RNA, v. 13, n. 6, p. e1720, 2022.
LIBBY, P. Lüscher T. COVID-19 is, in the end, an endothelial disease. Eur Heart J, v. 41, p. 3038-3044, 2020.
MAERTENS, Goedele N.; ENGELMAN, Alan N.; CHEREPANOV, Peter. Structure and function of retroviral integrase. Nature Reviews Microbiology, v. 20, n. 1, p. 20-34, 2022.
MANZANO, Giovanna S. et al. Acute disseminated encephalomyelitis and acute hemorrhagic leukoencephalitis following COVID-19: systematic review and meta-synthesis. Neurology-Neuroimmunology Neuroinflammation, v. 8, n. 6, 2021.
MARTÍN-GARRIDO, I.; MEDRANO-ORTEGA, F. J. Beyond acute SARS-CoV-2 infection: A new challenge for Internal Medicine. Revista Clínica Española (English Edition), 2022.
MERCOLA, Joseph; GRANT, William B.; WAGNER, Carol L. Evidence regarding vitamin D and risk of COVID-19 and its severity. Nutrients, v. 12, n. 11, p. 3361, 2020.
MOHER, David et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine, v. 151, n. 4, p. 264-269, 2009.
OMS. Organização Mundial de Saúde. Conselhos sobre doença coronavírus (COVID-19) para o público. 2022 Disponível em: < https://www.who.int/pt/emergencies/diseases/novel-coronavirus-2019/advice-for public?adgroupsurvey={adgroupsurvey}&gclid=Cj0KCQiAkMGcBhCSARIsAIW6d0Aq800D4W_6rzawkloiA663gy1wyD9gQgOARMqeG5_zj-ZTgL2CRyAaAu9vEALw_wcB >. Acesso em: 12 Jan 2023.
PAPPA, Sofia et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain, behavior, and immunity, v. 88, p. 901-907, 2020.
SCHOU, Thor Mertz et al. Psychiatric and neuropsychiatric sequelae of COVID-19–A systematic review. Brain, behavior, and immunity, v. 97, p. 328-348, 2021.
SOUSA, Liliana et al. Impacto psicológico da COVID-19 nos profissionais de saúde: revisão sistemática de prevalência. Acta Paulista de Enfermagem, v. 34, 2021.
WANG, Yumin et al. SARS-CoV-2-associated acute disseminated encephalomyelitis: a systematic review of the literature. Journal of Neurology, v. 269, n. 3, p. 1071-1092, 2022.
YESUDHAS, Dhanusha; SRIVASTAVA, Ambuj; GROMIHA, M. Michael. COVID-19 outbreak: history, mechanism, transmission, structural studies and therapeutics. Infection, v. 49, p. 199-213, 2021.
ZAMANI, Raha; POUREMAMALI, Rozhina; REZAEI, Nima. Central neuroinflammation in Covid-19: a systematic review of 182 cases with encephalitis, acute disseminated encephalomyelitis, and necrotizing encephalopathies. Reviews in the Neurosciences, v. 33, n. 4, p. 397-412, 2022.
ZELADA-RÍOS, Laura et al. Acute disseminated encephalomyelitis and COVID-19: A systematic synthesis of worldwide cases. Journal of Neuroimmunology, v. 359, p. 577674, 2021.
ZHANG, Yu et al. Smell disorders in COVID-19 patients: role of olfactory training: A protocol for systematic review and meta-analysis. Medicine, v. 100, n. 8, 2021.
[1] Student of the Medicine Course at the Federal University of Amapá (UNIFAP). ORCID: https://orcid.org/0009-0004-3070-4823. Lattes CV: http://lattes.cnpq.br/3498035518296432. Email: [email protected].
[2] Student of the Medicine Course at the Federal University of Amapá (UNIFAP). ORCID: https://orcid.org/0009-0006-9251-1263. Lattes CV: http://lattes.cnpq.br/2490105327753523. Email: [email protected].
[3] Student of the Medicine Course at the Federal University of Amapá (UNIFAP). ORCID: https://orcid.org/0009-0004-2383-7695. Lattes CV: http://lattes.cnpq.br/0973533830971228. Email: [email protected].
[4] Nurse. Post-Doctorate in Public Health with double degree from the Postgraduate Program of the Faculty of Nursing of UERJ, RJ and the Escola Superior de Enfermagem de Coimbra, Portugal. PhD in Public Health from the State University of Campinas. Master’s degree in Education from the State University of Rio de Janeiro. Professor at the Aurora de Afonso Costa School of Nursing at the Fluminense Federal University. Professor of the Academic Program in Health Care Sciences at UFF. ORCID: http://orcid.org/0000-0001-6249-0808. Lattes Curriculum: http://lattes.cnpq.br/6800822152435035. Email: [email protected].
[5] Nurse. Post-doctorate at the Abel Salazar Institute of Biomedical Sciences: Porto, Portugal. Professor at the Higher School of Nursing of Coimbra Higher School of Nursing of Coimbra, Portugal. ORCID: https://orcid.org/0000-0002-8825-4923. Lattes CV: http://lattes.cnpq.br/4260250781663255. Email: [email protected].
[6] PhD in Psychology and Clinical Psychoanalysis. PhD in progress in Communication and Semiotics from the Pontifical Catholic University of São Paulo (PUC/SP). Master’s degree in Religious Sciences from Universidade Presbiteriana Mackenzie. Master’s degree in Clinical Psychoanalysis. Degree in Biological Sciences. Degree in Theology. He has been working for over 15 years with Scientific Methodology (Research Method) in the Scientific Production Guidance of Masters and Doctoral Students. Specialist in Market Research and Research focused on the Health area. ORCID: 0000-0003-2952-4337. Lattes CV: http://lattes.cnpq.br/2008995647080248.
[7] Biologist. PhD and Master’s degree in Behavior Theory and Research from the Federal University of Pará. Professor and Researcher at the Federal Institute of Amapá – IFAP and the PROF-EPT Postgraduate Program. ORCID: http://orcid.org/0000-0003-0840-6307. Lattes CV: http://lattes.cnpq.br/8303202339219096. Email: [email protected].
[8] Biomedical. PhD and Master’s degree in Tropical Diseases from the Federal University of Pará. Professor at the Federal University of Amapá. Professor of the Postgraduate Program in Health Sciences at the Federal University of Amapá. ORCID: https://orcid.org/0000-0001-5128-8903. Lattes CV: http://lattes.cnpq.br/9314252766209613. Email: [email protected].
[9] Advisor. Doctor, Master’s Degree in Teaching in Health Sciences. Student of the Doctoral Course in Health Care Sciences at Universidade Federal Fluminense, School of Nursing Aurora de Afonso Costa. Niterói, Rio de Janeiro, Brazil. Professor of the Medicine Course at the Federal University of Amapá (UNIFAP), Macapá, Amapá, Brazil. ORCID: https://orcid.org/0000-0002-7742-144X. Lattes CV: http://lattes.cnpq.br/8427706088023830. Email: [email protected].
submitted: May 19, 2023.
Approved: June 21, 2023.















