ORIGINAL ARTICLE
RIBEIRO, Eliane de Oliveira Aranha [1], TABAL, Gabriella Bezerra [2], SOARES, Keuly Sousa [3], PRESTES, Gimol Benchimol Resende [4], SALINO, Alessandra Valle [5], QUEIRÓZ, Ana Karoline de Souza [6]
RIBEIRO, Eliane de Oliveira Aranha. Et al. Features And Dental Approach In Alagille Syndrome: Case Report. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year 06, Ed. 03, Vol. 16, pp. 158-170. March 2021. ISSN: 2448-0959, Access Link: https://www.nucleodoconhecimento.com.br/dentistry/dental-approach
ABSTRACT
Alagille syndrome (AS) is an autosomal dominant, multi-siemic, complex and infrequent disease with great variation in the penetrance of clinical characteristics. Describing these characteristics, oral findings and dental treatment of a patient with AS, emphasizing the care to be adopted, was the objective of this report. A 31-year-old female patient attended the Dental Clinic of Special Patients of the State University of Amazonas (UEA) for routine dental care. In the anamnesis reported presenting the As, being transplanted liver and use as medication Tacrolimus (Prograf®) continuously. On physical examination, a slightly yellowish skin, prominent forehead and nose was observed, and small exophthalmia was observed. In the intra-oral clinical examination, yellowish dentition was observed, presence of root rest of the 36 and dental calculus in the region of the upper and lower molars. The proposed and executed treatment was exodontia, supragingival scraping, prophylaxis and oral hygiene guidance. Outpatient dental treatment can be performed in patients with AS, provided that the peculiarities of the syndrome are observed. The role of the dentist in the promotion of oral health is relevant, in order to avoid the presence of infectious foci, especially in immunosuppressed patients.
Keywords: Alagille syndrome, clinical features, dental treatment.
INTRODUCTION
Alagille syndrome (AS) is an autosomal dominant, multi-simemic and complex disease with great variation in the penetrance of clinical characteristics (MITCHELL et al., 2018). Uncommonly affects 1 in 30/50,000 live births and was first described in 1970 based on liver, cardiac, facial clinical findings, among others (GILBERT et al., 2019).
According to Sousa and Resende (2018), the five major signs are: chronic cholestase (temporary, persistent or intermittent jaundice; itching beginning at 6 months; xantomas in the areas of skin friction); dysmorphic facy (protruding forehead; sunken eyes with discrete hypertelorism; pointed chin; flattened nose with bulb-shaped tip); cardiovascular anomalies (peripheral branch snoosis of the pulmonary artery, present in 90% of cases, with or without association with complex anomalies); defects of the vertebral arches (vertebrae in butterfly wing); and posterior embryotoxon (sign present in 10% of the general population, consists of thickening of the line formed by descemet membrane and the angle of the anterior chamber of the eye, evident by slit lamp or by gonioscopy). It is said to be complete when there is simultaneous presence of at least four signs, while the presence of only three of them characterizes the syndrome as incomplete. Alkaline phosphatase and gamma-glutamyltransferase enzymes (GT or GGT range) are very high in most cases.
Other less frequent clinical findings in the syndrome were also presented by Alagille et al. (1987), such as hypogonadism, shortening of the distal phalanges, deforming polyarticular arthritis, growth retardation, mental retardation, renal impairment (mesangiolipidosis, renal tubular acidosis, nephrocalcinosis) and altered volume and tone of the voice.
Diagnosis may be difficult due to the variable expressiveness of clinical manifestations (GUEGAN et al., 2012). A large portion of the patients affected by the syndrome have no family history, which reinforces the characteristic of incomplete penetrance, besides the possibility of a new genetic mutation (SOUSA; RESENDE, 2018). The prognosis of the disease and the risk of mortality depend on the severity of organ involvement. Early mortality is usually caused by heart disease or severe liver disease and subsequent mortality is often caused by strokes (SALEH et al., 2016).
With regard to facial features there are mild but recognizable dysmorphic features, including prominent forehead, deep eyes with moderate hypertelorism, ascending oblique palpebral fissures, depressed nasal bridge, straight nose with bulbous tip, large ears, prominent jaw, and pointed chin. In some children, the shape of the face is remarkably triangular. The prominent forehead seems less obvious in the adult, while the protrusion of the jaw and pointy chin are more obvious. It was considered that the facial phenotype differs in relation to whether the eyes are closed or not. Those who do not have deep eyes usually have narrow ascending oblique palpebral fissures, with remarkable hypertelorism (CIOCCA; ÀLVAREZ, 2012).
Regarding the oral cavity, the main effects are due to liver dysfunctions: enamel hypoplasia, tooth pigmentation due to bilirubin accumulation, generalized delay in eruption, greater susceptibility to the development of caries, among others (SHEEHY et al., 2000; LIN et al., 2003; AMARAL et al., 2008).
The severity of this syndrome varies from individual to other, and may present mild symptoms to the need for liver transplantation (TORRES et al. 2006).
AS can lead to a terminally ill liver disease, requiring treatment through liver transplantation. In transplantation, the greatest complication is the possibility of rejection. One of the main causes of this, in addition to tissue incompatibility, is pre- and postoperative infection. The oral cavity has pathogenic bacteria that can produce bacteremia with the potential to cause infections in other organs of the body (AL-MUTAWA, 2002). Demonstrating the relevance of monitoring and preserving oral health of these patients.
Therefore, the present study aims to describe the clinical characteristics of this pathology, its oral findings and the dental treatment of a patient with AS, emphasizing the care to be adopted.
CLINICAL CASE
Patient A.C.C.S.F. 31 years old, female gender, melanoderma, natural and coming from Manaus-AM, attended the Dental Clinic of Special Patients of the State University of Amazonas (UEA) for routine dental care.
In the anamnesis reported presenting sa, being transplanted liver, using as medication Tacrolimus (Prograf®), immunosuppressive medication that inhibits the activation of T lymphocytes, and that makes use of this drug since transplantation. He reported having a “bothering tooth.”
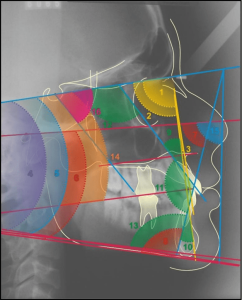
On physical examination, a prominent slightly yellowish skin, forehead and nose and small exophthalemia were observed (Figure 1).
Figure 1 – Facial clinical features

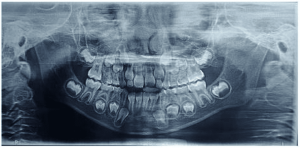
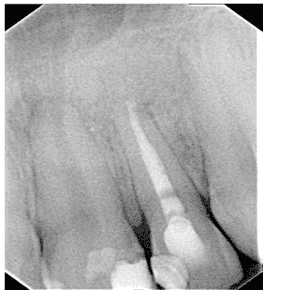
In the intra-oral clinical examination, yellowish dentition was observed, presence of root rest of 36 and dental calculus in the region of the upper and lower molars (Figure 2 and 3).
Figure 2 – Initial clinical examination showing the presence of left lower root rest (36)
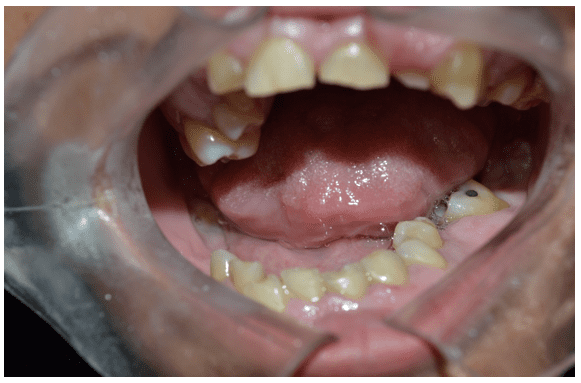
Figure 3 – Initial clinical examination

Source: Personal archive
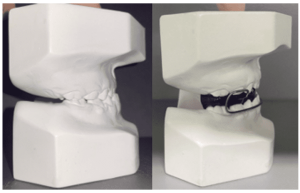
The proposed and executed treatment was exodontia, supragingival scraping, prophylaxis and oral hygiene guidance. To perform the procedures, complementary preoperative laboratory tests (complete blood count, coagulogram, creatinine and glycemia) and radiographic tests were requested. In the next consultation, the patient brought the tests that were within normal standards. Antibiotic prophylaxis was then performed with Amoxicilin 2 grams, 1 hour before the surgical procedure and surgical removal of the element (Figure 4 and 5). In the following consultation, supragingival scraping, prophylaxis and oral hygiene guidance were done.
Figure 4 – Surgical removal of tooth 36.
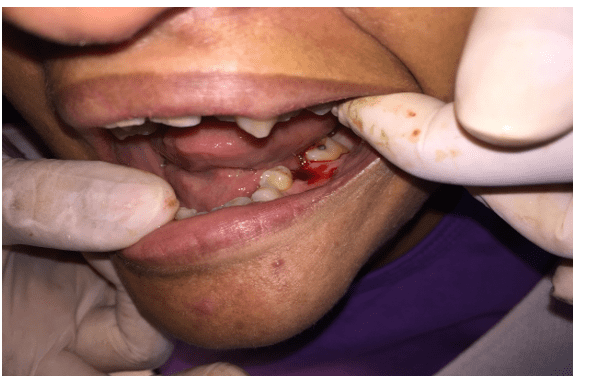
Figure 5 – Periapical radiography of the lower molars.

DISCUSSION
Over the years, the number of liver transplant surgeries has increased and with this, patient survival has improved significantly. Immunosuppressive therapies, using drugs such as cyclosporine, tacrolimus and sirolimus, act to prevent rejection of the received organ. The desired immunosuppressive effect is to prevent rejection of the graft by the immune system, while preserving the control of infections and neoplasms (PILLAI and LEVITSKY, 2009). These data corroborate our study, since the patient in this report has age group and drug therapy compatible with the literature cited.
The most frequent complications affecting immunosuppressed patients originate from opportunistic infections, which tend to evolve rapidly to acute systemic conditions (OLCZAK et al., 2010; VIVAS, 2012). After performing the transplant, the patient is subordinated to immunosuppressive treatments throughout life, which can promote the development of fungal and viral infections, with oral candidiasis and herpes simplex lesions being the most common (SCULLY, 1992). It is up to the dentist to observe the presence of these alterations and treat them. Depending on the severity, the immunosuppressive drug may have the dose adjusted or even be modified by the doctor.
Due to immunosuppressive treatment or the drugs used, transplant patients may present with a variety of oral lesions. This site where we can find numerous microorganisms, which may include those of viral or fungal origin, malignancies, gingival hyperplasia, among many other alterations (SEYMOUR et al., 1997).
Saalman et al. (2010) described a study in which eight transplanted children using tacrolimus presented oral lesions (edema and cleft lips, angular cheilitis and nodules on the back of the tongue). Diverging from these authors, this report is found, since no indications of oral alterations were observed on clinical examination, even the patient using tracolimus.
Drug gingival hyperplasia associated with the use of cyclosporine and calcium channel-blocking drugs such as nyphedidin and amlodipine is already a well-known episode. Wright et al. (2005) presented in their literature review on gingival augmental related to cyclosporine use, that the predominance of this alteration can vary from 8 to 100% of patients undergoing transplantation surgery. Vivas (2002) conducted a study at the Hospital AC Camargo, São Paulo (SP), in which of the 13 patients evaluated, 8 used cyclosporine and 5 other patients used tracrolimus and calcium channel blockers. No patient who had gingival hyperplasia used only tracolimus (1 used nyfedipine and the other 4 used amlodipine). This report corroborates the literature, showing that tracolimus does not cause gum hyperplasia, but rather the calcium channel blocking drugs that are used concomitantly.
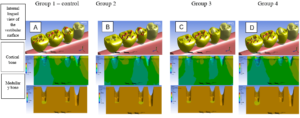
Dental manifestations are not a primary feature of the syndrome, but occur invariably as a complication of long-term cholestasis and are related to hyperbilirubinemia.As a consequence of cholestatic during odontogenesis, enamel opacities, hypomineralization and tooth enamel hypoplasia may arise. Both primary and permanent dentition can be strongly affected if developed before resolution of jaundice. Authors report the presence of claw cusps in both deciduous and permanent teeth in patients with AS (PRAVEEN et al., 2011; CHATTERJEE and MASON, 2007). Others report macrodontic upper incisors and, in some cases, taurodontic deciduous teeth with enlarged pulp cavity (CALLEA et al., 2013; COZZANI and FONTANA, 2012). And others have noted that patients with AS have hypodontia and oral xantomas (BERNICZEI-ROKYO et al., 2014). In contrast to these references, this case study is found, since none of these changes were observed.
One of the main dental alterations that can be found in patients with cholestatic diseases is bilirubin tooth pigmentation. Studies presented by Hosey et al. (1995), Wondimu et al. (2001) and Lin et al. (2003), revealed a prevalence of this intrinsic pigmentation in 50 to 61.3% of patients. These data are compatible with the patient, where there was a change, even if mild, in dental staining.
The oral cavity harbors pathogenic substances that can cause acute inflammation of organs such as pneumonia, gastritis, peptic ulcers and infectious endocarditis, which can be harmful to transplant patients. Therefore, it is recommended that the patient make preventive dental consultations.Before surgery, all carious cavities should be treated and restored or removed, the periodontum should be healthy and oral hygiene should be very good. Infected teeth are believed to increase the overall systemic inflammatory load of the body because of the release of oral bacterial metabolites into the bloodstream and via inflammatory and immunological responses from the host (OFFENBACHER et al., 2008). The treatment of patients with AS does not differentiate usal in any procedure, unless prophylactic antibiotic care is taken care of (TORRES et al., 2006). This should be carried out in partnership with the doctor, as there may be a need for specific drug prescription (BERNICZEI-ROKYO et al., 2014). Ratifying these studies, the patient’s surgical dental treatment was performed with the prescription of antibiotic prophylaxis, as well as oral hygiene guidelines.
Adjusting oral conditions, with the removal of odontogenic foci before transplantation, can reduce complications during the medical procedures necessary for solid organ recipients (GULLEÇ et al., 2003). Oral hygiene instruction is an effective strategy for the reduction of periodontopathogenic microorganisms, reducing the incidence of bacteremias and subsequent complications during the immunosuppression period, as well as the removal of local infectious foci, according to the dental performance performed in the patient of this study.
CONCLUSION
Outpatient dental treatment can be performed in patients with AS, provided that the peculiarities of the syndrome are observed. The role of the dentist in the promotion of oral health is relevant, in order to avoid the presence of infectious foci, especially in immunosuppressed patients. The dentist also needs to be aware of cardiovascular and hepatic problems related to the syndrome; efficient treatment, contributing to the overall well-being of the patient.
REFERENCES
ALAGILLE, D. et al. Syndromic paucity of interlobular bile ducts (Alagille syndrome or arteriohepatic dysplasia): review of 80 cases. J Pediatr; v.110, p. 195-200, 1987.
AL-MUTAWA, S. et al. Oral findings in Alagille syndrome. Medical Principles and Practice, v.11, n. 3, p.161-163, 2002.
AMARAL TH, de Guerra CS, Bombonato-Prado KF, et al. Tooth pigmentation caused by bilirubin: a case report and histological evaluation. Spec Care Dentist., v. 28, n.6, p. 254–57, 2008.
BERNICZEI-ROYKO, A. et al. Medical and dental management of Alagille syndrome: a review. Med Sci Monit, v.20, p. 476-480, 2014.
CALLEA M, et al. Síndrome de Alagille: uma revisão. J Int Dent Med Research. v.6, n.1, p. 54–58, 2013.
CIOCCA, M.; ÀLVAREZ, F. Síndrome de Alagille. Arch Argent Pediatr, v. 110, n.6, p. 509-515, 2012.
CHATTERJEE, M.; MASON, C. Talon cusps presenting in a child with Alagille’s syndrome – a case report. J Clin Pediatr Dent., v. 32, n. 1, p. 61–64, 2007.
COZZANI, M.; FONTANA, M. Macrodontic maxillary incisor in alagille syndrome. Dent Res J., v. 9, n. 8, p. 251–254, 2014.
GILBERT, M. et al. Hum Mutat. 2019 Dec;40(12):2197-2220.
GUEGAN, K. et al. JAG1 mutations are found in approximately one third of patients presenting with only one or two clinical features of Alagille syndrome. Clin Genet., v. 82, p.33–40, 2012.
GULLEÇ, A.T. et al. Superficial fungical infections in 102 patients renal transplant recipients: a case control study. J Am Acad Dermatol.,v. 49, p.187-192, 2003.
HOSEY, M.T. et al. Oral findings in children with liver transplants. Int J Paediatr Dent., v. 5, n.1,p. 29-34, 1995.
LIN YT, LIN YT, CHEN CL. A survey of the oral status of children undergoing liver transplantation. Chang Gung Med J. v. 26, n.3, p. 184-188, 2003.
MITCHELL, E. et al. Alagille syndrome. Clin Liver Dis., v. 22, p.625–41, 2018.
OFFENBACHER, S. et al. Rethinking periodontal inflammation. J Periodontol, v. 79, p. 1577– 1584, 2008.
OLCZAK, B. et al. Oral candidiasis in immunosuppressed children and young adults after liver or kidney transplantation. Pediatr Dent. v. 32, n. 3, p.189-94, 2010.
PILLAI, A.A.; LEVITSKY J. Overview of immunosuppression in liver transplantation. World J Gastroenterol. v. 15, n.34, p. 4225-4233, 2009.
PRAVEEN P, et al. Cúspide de garra em um dente decíduo. J Dent Sci Res. v. 2, n.1, p. 34–40, 2011.
SAALMAN, R. et al. Long‐standing oral mucosal lesions in solid organ‐transplanted children‐a novel clinical entity. Transplantation 89: 606– 611. 2010.
SALEH, M. et al. Alagille syndrome: clinical perspectives. Appl Clin Genet., v.9, p.75-82, 2016.
SCULLY C. Oral Infectinos in the immunocompromised patient. Br Dent J. v.172, n.11, p. 401-407, 1992.
SEYMOUR, R.A. et al. Oral lesions in organ transplant patients. J Oral Pathol Med., v.26, n.7, p. 297-304, 1997.
SHEEHY EC, et al. Oral Health in children undergoing liver transplantation. Int J Pediatr Dent., v.10, n.2, p. 109-19, 2000.
SOUSA, A. C .M.; RESENDE, L. R. Síndrome de Alagille – relato de caso. Resid Pediatr. v.8, n.2, p.85-88, 2018.
TORRES, C.P. et al. Síndrome de Alagille: relato de caso. J. Health Sci. Inst., v. 24, n.2, p.149-153, 2006.
VIVAS, A. P. M. Avaliação de manifestações bucais em pacientes pediátricos submetidos ao transplante hepático.2012 Dissertação (Mestrado em Patologia Bucal) – Faculdade de Odontologia da Universidade de São Paulo, São Paulo, 2012.
WONDIMU, B.; NEMETH, A.; MODEER, T. Oral health in liver transplant children administered cyclosporin A or tacrolimus. International journal of paediatric dentistry, v. 11, n. 6, p. 424-429, 2001.
WRIGHT G., WELBURY RR., HOSEY MT. Cyclosporin‐induced gingival overgrowth in children. Int J Paediatr Dent., v.15, n.6, p. 403-411, 2005.
[1] Master Professor at the State University of Amazonas.
[2] Undergraduate student of the State University of Amazonas.
[3] Specialist Professor at the Amazonas State University.
[4] PhD Professor, Amazonas State University.
[5] PhD Professor, Amazonas State University.
[6] Dentist, Specialist in Patients with Special Needs.
Submitted: February, 2021.
Approved: March, 2021.