ORIGINAL ARTICLE
SOUZA, Diogo Henrique Vaz de [1], SAKAMOTO, Silvio Pedro da Silva [2], TERADA, Andrea Sayuri Silveira Dias [3], BORGES, Alexandro Luiz Souto [4], TONIOLLO, Marcelo Bighetti [5]
SOUZA, Diogo Henrique Vaz de. et al. Occlusal load and biomechanics of implant-supported fixed partial dentures: bone stress analysis. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year 07, Ed. 12, Vol. 02, pp. 109-124. December 2022. ISSN:2448-0959, Access link in: https://www.nucleodoconhecimento.com.br/dentistry/implant-supported, DOI: 10.32749/nucleodoconhecimento.com.br/dentistry/implant-supported
ABSTRACT
Osseointegration emerged in the 1950s, created by Per-Ingvar Branemark, when it was conceptualized as an intimate connection between the implant and the surrounding bone, and with this discovery, it was proposed as a treatment for total or partial edentulism. implants supported. Excessive loads generated by poor adjustment of occlusal forces are recurrent and common, and may generate resorption in the supporting bone; in situations of excess occlusal load, when these loads are distributed at different intensities, on different dental occlusal tables, could this be a reason for the failure of implant-supported rehabilitation? What about the absence of occlusal loading? Could this be a reason for the failure of implant-supported prosthetic rehabilitation? What will be the way to avoid exacerbated stress on occlusal tables, leading to a better generation of treatment prognosis, especially in cases of Fixed Partial Dentures (FPD) with suspended artificial teeth? This study aims, using the finite element methodology, to build a clinical situation of an implant-supported partial denture (FPD) of fixation of 3 elements of regular length, where the location of the occlusal loads (newtons) (total 750N) in the (FPD) ( Fixed Partial Denture) defined in the experimental groups, with higher loads being selected on the occlusal surface of the molar tooth in relation to the premolar, and with different occlusal forces on adjacent teeth, according to an occlusal load proposed in the research. Thus, the occlusal load was distributed, in different intensities, between each tooth of the CAD (Computer Aided Design) model. The biomechanical behavior and stresses of the fragile structures analyzed vary according to the occlusal load exerted and, therefore, controlling such occlusal loads is very relevant. The tensions are always greater and more evident in the posterior regions, whether in the cortical bone or in the medullary bone, especially when occlusal loads are applied unevenly with overload on the posterior elements of the fixed partial denture; therefore, one should always try to preserve these more distal elements.
Keywords: Fixed partial denture, Dental occlusion, Cortical bone, Cancellous bone.
1. INTRODUCTION
Osseointegration emerged in the 1950s created by Per-Ingvar Branemark, and was discovered in a study with bones, at which time it was conceptualized as the intimate connection between the implant and the surrounding bone. (BRANEMARK, et al., 1977) Despite the brilliant discovery, limitations continue to exist and distance the behavior of natural teeth from bone-integrated dental implants. This fact directly reflects the difficulty and importance of occlusal adjustment on artificial teeth in order to preserve the implant-supported rehabilitation. (JACOBS and VAN STEENBERGHE, 1993)
Some authors Frost (1994), Glickman (1971), Rios et al. (2008) mention that deleterious effects generated by poor adjustment of occlusal loads are recurrent and common, which generates different reactions in supporting bone; loads without excess can preserve the bone quality, but they can also generate resorptions due to inactivity.
Hämmerle and Tarnow (2018), Stoichkov and Kirov (2018) and Meriç et al. (2011) stated that avoiding stress generation exacerbated by changing the distribution of occlusal loads tends to lead to a better treatment prognosis, especially in cases of Fixed Partial Denture (FPD) with suspended artificial teeth (pontic).
The literature shows that cases in which these abovementioned facts are not respected can lead to failures and/or fractures, (PEIXOTO and ALMAS, 2016; DEMENKO et al., 2016; MOSNEGUTU et al., 2015). and other numerous possible damages to the bone tissue, (FLANAGAN, 2008; SPRAY et al., 2000) teeth, (FLANAGAN, 2016) temporomandibular joint, (SANTANA-MORA et al., 2014) rehabilitations (GIBBS et al., 1981) and restorations. (ROQUE et al., 2016)
Sekita et al. (2016), Bagi et al. (2011) and Geng et al. (2001) stated that the way in which the stress generated in applying the occlusal load is dissipated can be a crucial point for the rehabilitation success or failure, as well as for the implant stability and the bone tissue peri-implant behavior. The increase in occlusal pressure generated by premature contacts between antagonistic teeth (for example) can cause excessive force in the peri-implant region and be the source of problems for rehabilitation at the time of the intercuspation position. (GIBBS et al., 1981) This tends to cause lower bone density in the region surrounding the implant, which causes crater-shaped resorptions. (SOHN et al., 2011, DUYCK, et al., 2001)
Professionals in the area are aware of the importance of occlusal adjustment, but greater understanding of the subject is necessary. According to Costa et al. (2011), balanced occlusion is necessary, a situation in which all dental contacts are established and distributed over the arch so that there is better force distribution.
Therefore, this study aimed to evaluate the biomechanical behavior in relation to stress dissipation in the bone tissue surrounding the implants according to variation in the applied occlusal load distribution, varying their location on implant-supported (Fixed Partial Denture) FPD.
2. MATERIAL AND METHODS
This study evaluated different types of occlusal loading on a (Fixed Partial Denture) FPD on two implants containing an intermediate pontic through three-dimensional analysis using the (Finite Element Method) FEM. Cylindrical implants inserted 2mm infra bone were used with 3.5mm transmucosal prosthetic abutments. The cortical bone and mucosa thickness were set at 2mm.The models and their respective parts (Computer Aided Designers) CADs were generated, meshed and had mechanical characteristics assigned. All models were considered isotropic, homogeneous and linearly elastic. Contact surfaces between the parts of the models were considered fixed (“bonded”). The infrastructures of the (Fixed Partial Dentures) FPDs were zirconia (“metal-free” – modulus of elasticity 269,000 (Mega Pascal) MPa and Poisson’s coefficient 0.25 – reference by Arinc, (2018) and Güngör and Yilmaz, 2016) and covered by feldspathic ceramic (modulus of elasticity 80,000 (Mega Pascal) MPa and Poisson’s coefficient 0.30 – reference from Arinc (2018) and Erkmen et al., 2011, with screw hole closure with composite resin. The assigned elasticity modulus and Poisson’s coefficient were based on a bibliographic reference by Toniollo et al. (2012). The supporting bone tissues, both cortical and medullary, had bone type I mechanical characteristics.Identical total occlusal load was applied to all models 750 (newton) N, obliquely close to 30 degrees, at the same occlusal points. The molars received an occlusal load greater than the premolars, with the location of this load varying between groups.- Group 1 (control): homogeneous occlusal loading distributed over the occlusal table of the entire implant-supported (Fixed Partial Denture) FPD, with 150 (newton) N in the premolar and 300 (Newton) N in each molar.- Group 2: occlusal loading located only in the most anterior and intermediate elements of the implant-supported (Fixed Partial Denture) FPD, with 200 (Newton) N in the premolar and 550 (Newton) N in the 1st molar (pontic).- Group 3: main occlusal loading located in the intermediate element (pontic) and in part of the anterior and posterior elements of the implant-supported (Fixed Partial Denture) FPD, with 550 (Newton) N in the 1st molar, 100 (Newton) N in the mesial of the 2nd molar and 100 (Newton) N in the distal premolar.- Group 4: occlusal loading located only in the most posterior and intermediate (pontic) elements of the implant-supported (Fixed Partial Denture) FPD, with 375 (Newton) N in the 1st molar and 375 (Newton) N in the 2nd molar.
Figure: 1: The 4 experimental groups, described below
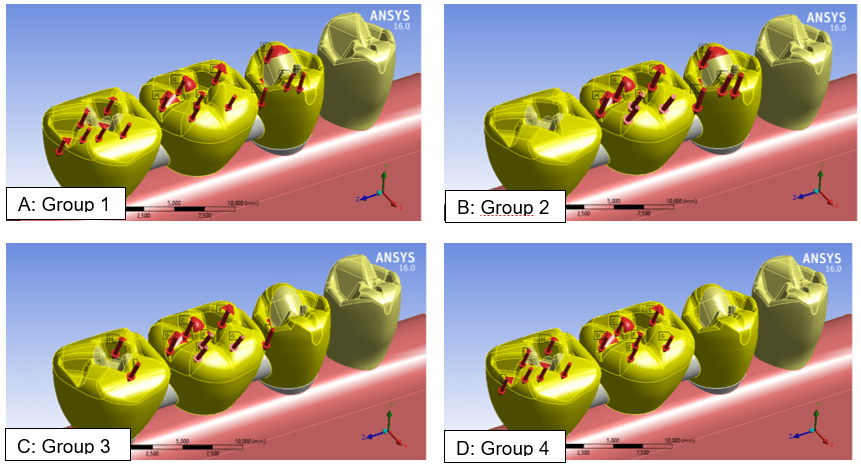
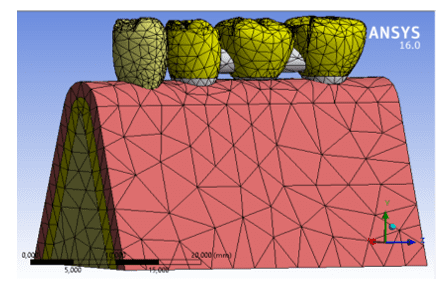
Figure 2: 3-D transparency view of the master model used for the experimental group
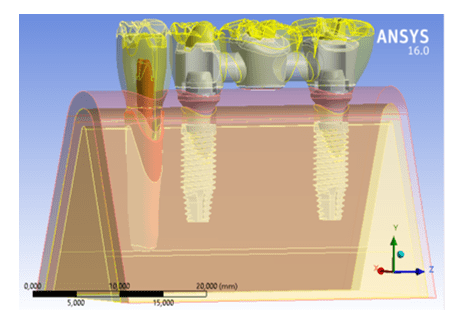
Figure 3: Finite element mesh generated on the master model
The evaluation was carried out using the (The Finite Element Method) FEM with simulations using the AnsysWorkbench 16.0 software program. The results were then quantitatively (absolute values of stresses developed in the proposed experimental groups) and qualitatively analyzed (location, intensity and dispersion of the generated stresses).
The scales of values obtained in the simulations varied according to the stresses obtained in each group, and thus the scales were standardized in their values and color references to enable better comparison between the experimental groups; in other words, a scale of unique values was used for the 4 experimental groups to analyze the cortical bone, and the same was performed to analyze medullary bone.
3. RESULTS
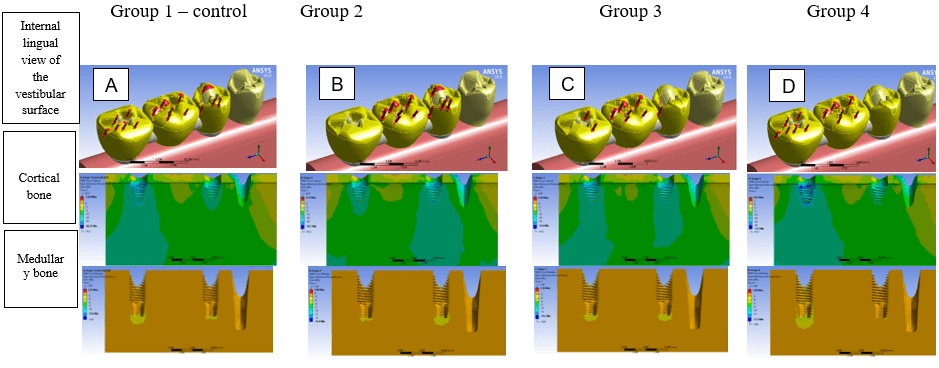
The simulations enabled obtaining (Minimum Principal stress) TMiP results in the supporting cortical and medullary bones according to the experimental groups simulated in the different occlusal loads. The results of the analyzed bone tissues from the internal lingual view of the vestibular surface (obtained by the longitudinal section of the model) are presented below (Figure 4). It is noteworthy that the most evident (Minimum Principal stress) TMiP are represented by the coldest and most negative colors, which will be analyzed in a module. Graph 1 shows the stress values obtained (Mega Pascal) (MPa) in bone tissues according to the experimental groups.
Figure 4: Results of experimental groups for stresses in cortical and medullary bones (internal lingual view of the vestibular surface); A: Group 1 (control) – homogeneous and distributed occlusal loading throughout the (Fixed Partial Denture) FPD; B: Group 2 – occlusal loading in the most anterior and intermediate element of the (Fixed Partial Denture) FPD; C: Group 3 – occlusal loading in the intermediate element and in part of the anterior and posterior elements of the (Fixed Partial Denture) FPD; D: Group 4 – occlusal loading in the most posterior and intermediate element of the (Fixed Partial Denture) FPD
Graph 1: (Minimum Principal stress) TMiP obtained in cortical and medullary bone tissues for the respective experimental groups
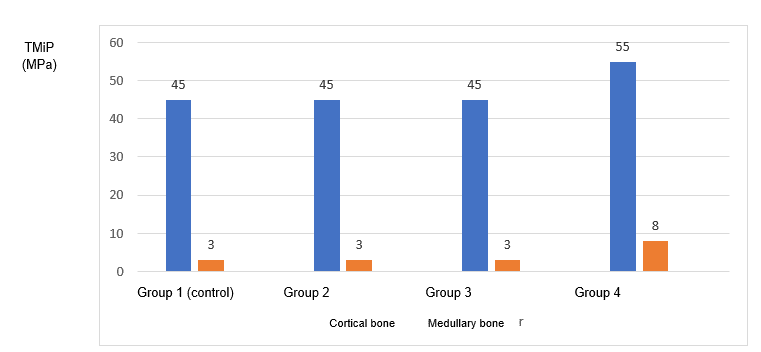
The results in Figure 4 show that cortical bone stress is especially concentrated in the cervical area of the implants, mainly in the more posterior implants. Figure 4D (Group 4) shows the highest stress values in which there is loading in the most posterior and intermediate elements, reaching up to 55 (Mega Pascal) MPa. The values in the other groups are around 45 (Mega Pascal) MPa (Graph 1).
The results (still in Figure 4) show that the stress in medullary bone is concentrated, as in cortical bone, notably in the more posterior areas, but always in the apical region of the implants. Groups 2 and 4 presented the highest (Minimum Principal stress) TMiP in the medullary bone (Figures 4B and 4D) with values close to 17 (Mega Pascal) MPa and 15 (Mega Pascal) MPa, respectively, which were disregarded for analysis as they come from inconsistencies in the mesh in specific insignificant areas. It can be seen that the relevant apical medullary bone stresses are clearer in Group 4 and did not exceed approximately 8 (Mega Pascal) MPa (Graph 1).
4. DISCUSSION
According to Flanagan (2017), the intensity of the bite force in the human species can reach an average of 800 (Newton) N, in which attention should be paid to the need for greater bone structure in order to withstand the generated stresses. Thus, the loads applied in the simulated posterior segment in the present study were 150 (Newton) N for the premolar and 300 (Newton) N for each molar, which totaled a load of 750 (Newton) N on the (Fixed Partial Denture) FPDs.
There is an ideal occlusion type to be used for each type and size of implant-supported prosthesis. (COSTA et al., 2011) The implant-supported fixed total dentures must be installed in mutually protected occlusion, seeking to perform the canine guide to avoid antagonization by contact of the posterior teeth during excursive mandibular movements. (CHAPMAN, 1989) Bilateral balanced occlusion can be used in cases where there is an antagonist arch with conventional removable prostheses so that prosthetic occlusal stability is achieved. (CHAPMAN, 1989)
Such concepts are mainly more suitable when considering excursive mandibular movements, or dynamic ones. However, there is also the relationship of static occlusal contacts regarding the relationship between working cusps and antagonistic elements. This relationship, conventionally known as occlusal contacts in maximum intercuspation, is also a delicate factor which can generate premature contacts and occlusal injuries when poorly adjusted.
In the present study, it was possible to simulate and predict the stress generated with occlusal loads similar to maximum intercuspation, and therefore the option to use contacts at the cusp tip and groove bottom was chosen. In turn, by varying the experimental groups in this study, it can be seen that its variation according to the group proposals exerted biomechanical reflexes on the support structures, even when using the same pre-established occlusal points. Varying the occlusal load in a more balanced way in all of the (fixed partial denture) FPD elements, or in the most anterior, middle or posterior direction and always keeping the total occlusal load equal to 750N generated different stress behaviors in the bone tissue.
Taking into account the results (Graph 1) of stresses (Minimum Principal stress) (TMiP) obtained in cortical bone, the highest compression stresses were in Group 4 (around 55 (Mega Pascal) MPa, against an average of 45 (Mega Pascal) MPa in the other groups), meaning that the poorly distributed occlusal load, mainly in the (Fixed Partial Denture) FPD posterior region, represented the most harmful or risky situation for cortical bone behavior, especially in the cortical bone surrounding the most posterior implant. It is also noticed that (as expected) there is greater reverberation of stresses along the cortical bone, converging with the loading location; but it is noteworthy that (as observed in Group 2) there is stress generated in this area, even with no occlusal load located directly in the area of the most posterior molar. This may be explained by lacking an element adjacent to it, which causes less stabilization of the (Fixed Partial Denture) FPD in the distal part. In analyzing Group 1-control, it is also noted that the area which most suffers from bone stress cervical to the implant is the most posterior, even with uniformly distributed occlusal loading. These observations reveal that the more you preserve the more posterior elements of a rehabilitation, especially those with a larger occlusal table, the more secure the biomechanics of the supporting peri-implant tissues will be. As stated, the maximum stress values in cortical bone were around 55 (Mega Pascal) MPa, which is not concerning in relation to the harmful levels, considered to be around 170 (Mega Pascal) MPa in the literature. (PELLIZZER et al., 2018; LINETSKIY et al., 2017; PAPAVASILIOU et al., 1996; YAMADA, 2013).
Taking into account the results (Graph 1) of stresses (Minimum Principal stress) (TMiP) obtained in medullary bone, it is observed that there were no significant values greater than approximately 8 (Mega Pascal) MPa in the experimental groups, despite the maximum values recorded. If this is correlated with references by Linetskiy et al. (2017), Teixeira et al. (2010) and Frost (2004), in which they mention a maximum tolerance to the medullary bone of around 10 (Mega Pascal) MPa, this study did not find possible injury or bone resorption areas.
A very small variation in stress located in the apical region surrounding the implants is perceived, which then reveals a relatively small biomechanical consequence in the medullary bone (in values) when there is a variation in occlusal loading in the proposed (Fixed Partial Denture) FPD. Although the variation in the absolute values obtained is small (graph 1), it is clear that there is a considerable difference in the coverage area of these stresses; this is because by observing Group 4 (Figure 4D), we can see there is a much larger area affected by the stresses reverberated around the apex of the most posterior implant than that observed (for example) around the apex of implants in Groups 2 and 3 (Figures 4B and 4C), and even in Group 1-control (Figure 6A).
Therefore, in observing correct occlusal adjustment, and mainly in seeking to preserve more (Fixed Partial Denture) FPD posterior areas (places where there are fewer bulkheads and/or adjacent structures to contain the proximal movement, and constituting a fact which may have been one of the factors causing greater tension in the more distal areas and associated with the larger occlusal table of the molars), is of great importance and requires attention to control the patient’s occlusion in implant-supported prostheses.
5. CONCLUSIONS
The biomechanical behavior and the stresses of the analyzed fragile structures vary according to the occlusal loading exerted, and therefore controlling such occlusal loads is very relevant.
Stresses are always greater and more evident in the posterior regions whether in cortical bone or medullary bone, especially when non-uniformly applying occlusal loads with overload on the (fixed partial denture) FPD posterior elements; therefore, an attempt to always preserve these most distal elements should always be made.
6. ACKNOWLEDGMENTS
The researchers involved in this project appreciate the incentives provided by the University of Rio Verde (UniRV) and (National Council for Technological and Scientific Development) (CNPq).
REFERENCES
ARINC, Hakan. Implant-supported fixed partial prostheses with different prosthetic materials: a three-dimensional finite element stress analysis. Implant Dentistry, v. 27, n. 3, p. 303-310, 2018. DOI: 10.1097/ID.0000000000000750. Acess in: 15 Aug. 2021.
BAGI, Cedo. M.; EDWIN, Berryman.; MOALLI, Maria. R. Comparative bone anatomy of commonly used laboratory animals: implications for drug discovery. Comparative Medicine, v. 61, n. 1, p. 76-85, 2011. PMID: 21819685. Acess in: 15 Aug. 2021.
BRANEMARK, Per. Ingvar.; HANSSON, B. O.; Adell, R.; BREINE, U.; LINDSTROM, J.; HALLEN, O.; OHMAN, A. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scandinavian journal of plastic and reconstructive surgery and hand surgery, v. 16, p. 132-141, 1977. PMID: 356184. Acess in: 20 Aug. 2021.
CHAPMAN, R. J. Principles of occlusion for implant prostheses: guidelines for position, timing, and force of occlusal contacts. Quintessence International, v. 20, n. 7, p. 473-480, 1989. PMID: 2697023. Acess in: 21 Aug. 2021.
COSTA, Patrícia. Dos. Santos.; GOMES, Érica. Alves.; PEREIRA, Cassiano. Costa. Silva.; JARDIM, Ellen. Cristian. Gaetti.; ZUIM, Paulo. Renato. Junqueira.; RANGEL, G. J. I. Occlusion in implant prosthodontics – part I. Innov. Implant J., Biomater. Esthet., v. 6, n. 2, p. 55-58, 2011. Disponible in: https://pesquisa.bvsalud.org/odontologia/resource/espt/lil-618580. Acess in: 01 Sep. 2021.
DEMENKO, Vladyslav.; IGOR, Linetskiy.; LARISA, Linetska.; VITALIJ, Nevist.; Shevchenko, ANDRII.; OLEG, Yefremov.; WEISSKIRCHER, Hans-Werner. Prognosis of implant longevity in terms of annual bone loss: a methodological finite element study. Computer Methods in Biomechanics and Biomedical Engineering, v. 19, n. 2, p. 180-187, 2016. DOI: https://doi.org/10.1080/10255842.2015.1005079. Acess in: 15 Sep. 2021.
DUYCK, Joke.; NAERT, Ignace.; RONOLD, Hans. Jacob.; OOSTERWYCK, Hans. Van.; SLOTEN, Van. Jos. The influence of static and dynamic loading on marginal bone reactions around osseointegrated implants: an animal experimental study. Clinical Oral Implants Research, v.12, n. 3, p. 207-218, 2001. DOI: https://doi.org/10.1034/j.1600-0501.2001.012003207.x. Acess in: 25 Sep. 2021.
ERKMEN, Erkan.; MERIÇ, Gökçe.; KURT, Ahmet.; TUNÇ, Yahya.; ESER, Atilin. Biomechanical comparison of implant retained fixed partial dentures with fiber reinforced composite versus conventional metal frameworks: a 3D FEA study. Journal of the Mechanical Behavior of Biomedical Materials, v. 4, p. 107-116, 2011. DOI: https://doi.org/10.1016/j.jmbbm.2010.09.011. Acess in: 25 Sep. 2021.
FLANAGAN, Dennis. A comparison of facial and lingual cortical thicknesses in edentulous maxillary and mandibular sites measured on computerized tomograms. Journal of Oral Implantology, v. 34, n. 5, p. 256–258, 2008. DOI: https://doi.org/10.1563/0.915.1. Acess in: 30 Oct. 2021.
FLANAGAN, Dennis. Bite force and dental implant treatment: a short review. Medical Devices, v. 10, p. 141-148, 2017. DOI: https://doi.org/10.2147%2FMDER.S130314. Acess in: 30 Oct. 2021.
FLANAGAN, Dennis. Diet and implant complications. Journal of Oral Implantology, v. 42, n. 3, p. 305-310, 2016. DOI: https://doi.org/10.1563/aaid-joi-D-15-00127. Acess in: 30 Oct. 2021.
FROST, Harold. M. A 2003 update of bone physiology and Wolff’s Law for clinicians. The Angle Orthodontist, v. 74, n. 1, p. 3-15, 2004. DOI: https://doi.org/10.1043/0003-3219(2004)074%3C0003:AUOBPA%3E2.0.CO;2. Acess in: 01 Nov. 2021.
FROST, Harold. M. Wolff’s law and bone’s structural adaptations to mechanical usage: an overview for clinicians. The Angle Orthodontist, v. 64, n. 3, p. 175-188, 1994. DOI: https://doi.org/10.1043/00033219(1994)064%3C0175:WLABSA%3E2.0.CO;2. Acess in: 01 Nov. 2021.
GENG, Jian-Ping.; TAN, Keson. B.; LIU, Gui-Rong. Application of finite element analysis in implant dentistry: a review of the literature. Journal of Prosthetic Dentistry, v. 85, n. 6, p. 585-598, 2001. DOI: https://doi.org/10.1067/mpr.2001.115251. Acess in: 01 Nov. 2021.
GIBBS, Charles. H.; MAHAN, Parker. E.; LUNDEEN, Harry. C.; BREHNAN, Kenneth.; WALSH, Edward. K.; SINKEWIZ, Susan. L.; GINSBERG, Sheila. B. Occlusal forces during chewing-influences of biting strength and food consistency. Journal of Prosthetic Dentistry, v. 46, p. 561-567, 1981.
GLICKMAN, Irving. Role of Occlusion in the Etiology and Treatment of Periodontal Disease. Dental Research, v. 50, n. 2, p. 199-204, 1971. DOI: https://doi.org/10.1177/00220345710500020501. Acess in: 20 Nov. 2021.
GÜNGÖR, Merve. Bankoğlu.; YILMAZ. Handan. Evaluation of stress distributions occurring on zirconia and titanium implant-supported prostheses: A three-dimensional finite element analysis. The Journal of Prosthetic Dentistry, v. 116, n. 3, p. 346-355, 2016. DOI: https://doi.org/10.1016/j.prosdent.2016.01.022. Acess in: 20 Nov. 2021.
HÄMMERLE, Christoph. H. F.; TARNOW, Dennis. The etiology of hard- and soft-tissue deficiencies at dental implants: a narrative review. Journal of Clinical Periodontology, v. 45, n. 20, p. 267-277, 2018. DOI: https://doi.org/10.1111/jcpe.12955. Acess in: 25 Nov. 2021.
JACOBS, Reinhilde., VAN STEENBERGHE, Daniel. Comparison between implantsupported prostheses and teeth regarding passive threshold level. International Journal of Oral & Maxillofacial Implants, v. 8, n. 5, p. 549-554, 1993. PMID: 8112795. Acess in: 25 Nov. 2021.
LINETSKIY, Igor.; DEMENKO, Vladyslav.; LINETSKA, Larissa.; YEFREMOV, Oleg. Impact of annual bone loss and different bone quality on dental implant success – A finite element study, Computers in Biology and Medicine, v. 1, p. 318-325, 2017. DOI: https://doi.org/10.1016/j.compbiomed.2017.09.016. Acess in: 25 Nov. 2021.
MERIÇ, Gökçe.; ERKMEN, Eran.; KURT, Ahmet.; TUNÇ, Yahya.; ESER, Atilin. Influence of prosthesis type and material on the stress distribution in bone around implants: a 3-dimensional finite element analysis. Journal of Dental Sciences, v. 6, n. 1, p. 25–32, 2011.: https://doi.org/10.1016/j.jds.2011.02.005. Acess in: 25 Nov. 2021. DOI
MOSNEGUTU, Adina.; WISMEIJER, Daniel.; GERAETS, Wil. Implant-supported mandibular overdentures can minimize mandibular bone resorption in edentulous patients: results of a long-term radiologic evaluation. International Journal of Oral & Maxillofacial Implants, v. 30, n. 6, p. 1378-1386, 2015. DOI: https://doi.org/10.11607/jomi.4009. Acess in: 30 Nov. 2021.
PAPAVASILIOU, George.; KAMPOSIORA, Phophi.; BAYNE, Stephen. C.; FELTON, David. A. Three-dimensional finite element analysis of stress-distribution around single tooth implants as a function of bony support, prosthesis type, and loading during function. The Journal of Prosthetic Dentistry, v. 76, n. 6, p. 633-640, 1996. DOI: https://doi.org/10.1016/S0022-3913(96)90442-4. Acess in: 30 Nov. 2021.
PEIXOTO, C. Davila.; ALMAS K. The implant surface characteristics and peri-implantitis. An evidence-based update. Odonto-stomatologie tropicale, v. 39, n. 153, p. 23-35, 2016. PMID: 27434917. Acess in: 01 Dec. 2021.
PELLIZZER, Eduardo. P.; LEMOS, Cleidiel. A. A.; ALMEIDA, Daniel. A. F.; BATISTA, Victor. E. Souza.; SANTIAGO JÚNIOR, Joel. F.; VERRI, Fellippo, R. Biomechanical analysis of different implant-abutments interfaces in different bone types: an in silico analysis. Materials Science and Engineering: C, v. 90, p. 645-650, 2018. DOI: https://doi.org/10.1016/j.msec.2018.05.012. Acess in: 01 Dec. 2021.
RIOS, H. F.; MA, D.; XIE, Y.; GIANNOBILE, W. V.; BONEWALD, S. E.; CONWAY, S. J.; FENG, J. Q. Periostin is essential for the integrity and function of the periodontal ligament during occlusal loading in mice. Journal of Periodontology, v. 79, n. 8, p. 1480-1490, 2008. DOI: https://doi.org/10.1902/jop.2008.070624. Acess in: 01 Dec. 2021. ROQUE, Miguel. A.; GALLUCCI, O. German.; LEE, J. Sang. Occlusal Pressure Redistribution with Single Implant Restorations, Journal of Prosthetic Dentistry, v. 26, n. 4, p. 275-279, 2016. DOI: https://doi.org/10.1111/jopr.12552. Acess in: 01 Dec. 2021.
SANTANA-MORA, Urbano.; MARTÍNEZ-ÍNSUA, Arturo.; SANTANA-PENÍN, Urbano.; PALOMAR, Amaya. P. del.; BANZO, José. C.; MORA, María. J. Muscular activity during isometric incisal biting. Journal of Biomechanics, v. 47, n. 16, p. 3891-3897, 2014. DOI: https://doi.org/10.1016/j.jbiomech.2014.09.007. Acess in: 01 Dec. 2021.
SEKITA, Aiko.; MATSUGAKI, Aira.; TAKUYA, Ishimoto.; TAKAYOSHI, Nakano. Synchronous disruption of anisotropic arrangement of the osteocyte network and collagen/apatite in melanoma bone metastasis. Journal of Structural Biology, v. 197, n. 3, p. 260-270, 2016. DOI: https://doi.org/10.1016/j.jsb.2016.12.003. Acess in: 05 Dec. 2021.
SOHN, Byoung-Sup.; HEO, Seong-Joo.; KOAK, Jai-Young.; KIM, Seong-Kyun.; LEE, Su-Young. Strain of implants depending on occlusion types in mandibular implant-supported fixed prostheses. The Journal of Advanced Prosthodontics, v. 3, n. 1, p. 1-9, 2011. DOI: https://doi.org/10.4047/jap.2011.3.1.1. Acess in: 06 Dec. 2021.
SPRAY, J. Robert.; BLACK, C. Gary.; MORRIS, Harold. F.; OCHI, Shigeru. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann Periodontol, v. 5, n. 1, p. 119-128, 2000. DOI: https://doi.org/10.1902/annals.2000.5.1.119. Acess in: 07 Dec. 2021.
STOICHKOV, Biser.; KIROV, Dimitar. Analysis of the causes of dental implant fracture: a retrospective clinical study. Quintessence International, v. 49, n. 4, p. 279-286, 2018.
TEIXEIRA, Marcelo. Fontes.; RAMALHO, Saturnino. Aparecido.; SARTORI MATTIAS, Ivete. Aparecida.; LEHMAN, Roberto. Brunow. Finite Element Analysis of 2 Immediate Loading Systems in Edentulous Mandible: Rigid and Semirigid Splinting of Implants. Implant Dentistry, v. 19, n. 1, p. 39-49, 2010. DOI: 10.1097/ID.0b013e3181cc7ffc. Acess in: 07 Dec. 2021.
TONIOLLO, Marcelo. Bighetti.; MACEDO, Ana. Paula.; RODRIGUES, Renata. Cristina. Silveira.; RIBEIRO, Ricardo. Faria.; MATTOS, Maria. Glória. Chiarello. Three-Dimensional Finite Element Analysis of Stress Distribution on Different Bony Ridges With Different Lengths of Morse Taper Implants and Prosthesis Dimensions. Journal of Craniofacial Surgery, v. 23, n. 6, p. 1888-1892, 2012. DOI: 10.1097/SCS.0b013e31826cf199 Acess in: 08 Dec. 2021.
YAMADA, Hiroshi. Strength of biological materials. 2. ed. Baltimore: Williams & Wilkins, 1970. 2013. p. 19-75.
[1] Bachelor’s Degree in Dentistry. ORCID: 0000-0003-0283-5653.
[2] Dentistry Student. ORCID: 0000-0003-3736-3473.
[3] PhD in Health Sciences from the Faculty of Medicine of Ribeirão Preto, University of São Paulo, specialist in Forensic Dentistry from the Faculty of Dentistry of Ribeirão Preto. ORCID: 0000-0002-9557-6664.
[4] Postdoctoral degree from the University of Indiana, Doctorate in Restorative Dentistry from UNESP, Master in Oral and Maxillofacial Prosthesis from UNESP, Graduated in Dentistry from Universidade Estadual Paulista “Júlio de Mesquita Filho”). ORCID: 0000-0002-5707-7565.
[5] Advisor. ORCID: 0000-0003-2167-4568.
Sent: September, 2022.
Approved: December, 2022.