CASE REPORT
COSTA, Maria Beatriz Tavares da [1], CAMPOS, Gabrielly Caldeira [2], PESSOA, Juliana Victória de Sousa [3], ARAÚJO, Marhia Eduarda Vilela de [4], ARAUJO, Priscila Pinto Brandão de [5], HANAN, Simone Assayag [6]
COSTA, Maria Beatriz Tavares da. et al. Anterior open bite treatment using Balters class II bionator: a case report. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year 08, Issue 08, Vol. 02, pp. 55-93. August 2023. ISSN: 2448-0959, Access Link: https://www.nucleodoconhecimento.com.br/dentistry/open-bite-treatment, DOI: 10.32749/nucleodoconhecimento.com.br/dentistry/open-bite-treatment
ABSTRACT
There are several reasons for the onset of malocclusion, which promotes disharmonious development of the craniofacial structure and may involve various factors such as incorrect positioning of teeth, maxilla, mandible, lips, tongue, and/or cheeks, possibly accompanied by deleterious oral habits. Malocclusion is a common finding that affects facial aesthetics, smile, as well as masticatory and respiratory functions, occurring in a large portion of the world’s population. Hence, a correct and early diagnosis is necessary for malocclusion treatment. There are various available treatments aiming for early correction of malocclusions. This clinical case report will describe a possible treatment for correcting an anterior open bite during the mixed dentition associated with a deleterious oral habit. The Balters’ Bionator is a functional orthopedic dento-muco-supported appliance that harmonizes the muscles of the tongue, lips, and cheeks, and treats skeletal discrepancies. At the end of this orthopedic treatment stage, the patient achieved the objectives of this work and will continue her care in a pediatric dental clinical setting at the Federal University of Amazonas-UFAM for further analysis and additional dentomuco-skeletal corrections.
Keywords: Malocclusion, Deleterious oral habits, Open bite.
1. INTRODUCTION
Within dentistry, there are many reasons why teeth may not occlude correctly, such as bone positioning, teeth, lips, tongue, and/or cheeks, or the presence of deleterious oral habits or breathing patterns (BATISTA et al., 2018).
Malocclusion is a common finding in the Brazilian population, potentially affecting facial aesthetics and the smile, often associated with skeletal abnormalities that severely impact and compromise the quality of life (RÉDUA, 2020). Due to Anterior Open Bite (AOB), malocclusion causes an esthetic and functional compromise, and it can be categorized by the lack of contact between the upper and lower teeth, resulting in a lack of overlap between them (NAKAO et al., 2016).
Early treatment of malocclusions is aimed at altering a disharmonic relationship in skeletal development, predominantly during the growth phase, modifying the remaining facial growth to a more favorable size or position of the jaws, using functional appliances. Studies have shown that functional orthopedic appliances act by modifying and redirecting growth (AKSU et al., 2017).
Anterior Open Bite (AOB) deserves attention due to its complex dysplasia (MENDES et al., 2020). Among the different treatments available for mixed dentition malocclusions, the Balters’ Bionator stands out, which is a functional dento-muco-supported appliance, designed and introduced by Wilhelm Balters in the 1950s (BIGLIAZZI et al., 2015).
This appliance is particularly indicated for patients with orofacial dysfunctions, such as persistent sucking habits or habitual mouth breathing, and it should harmonize the muscles of the tongue, lips, and cheeks. The Balters’ Bionator is a functional orthopedic appliance that acts on the patient’s craniofacial structure (JUNGBAUER et al., 2023).
The success of orthodontic treatment with removable orthopedic appliances depends on various factors, such as accurate and individualized diagnosis, appliance selection, and mode of use, i.e., how many hours the appliance should be worn per day. However, the skill and experience of the orthodontist count for little without the patient’s proper adherence (ARREGHINI et al., 2017).
Diagnosis is essential for treatment planning in the study of facial disorders. Conventional cephalometry allows the identification of skeletal, dental, and soft tissue problems in patients with malocclusions and is still widely used to evaluate angular and linear measurements (ANTUNES et al., 2013).
The introduction of the cephalostat standardized lateral cephalography, enabling more precise dentoskeletal diagnoses and evaluation of facial profile. It allows combining cephalometric analysis results with the clinical and subjective examination of each professional, enabling the achievement of an ideal occlusion with functional stability and facial aesthetics (LANDÁZURI et al., 2013).
Considering the importance of early interception of malocclusions in childhood for proper bone growth, dental development, improved breathing and swallowing patterns, it becomes essential to present a clinical case report describing the use of a functional orthopedic appliance as an option for correcting open bite, incisor protrusion, aiming for maxillary transverse growth, and addressing the reduction of non-nutritive sucking.
2. CASE REPORT
2.1 THERAPEUTIC CONDUCT
Female patient, 6 years old, mixed race, elementary school student, Brazilian, residing in and a native of Manaus-Amazonas, convex profile, with an open bite and deleterious digital sucking habit, presented on September 2, 2022, to the discipline of Pediatric Dentistry II at the Faculty of Dentistry of the Federal University of Amazonas (FAO-UFAM), for dental treatment, accompanied by her mother, with the signing of the Informed Consent Form.
During the anamnesis, the guardian reported seeking dental care for the first time due to the main complaint of “Pain in the last tooth during chewing,” which was continuous and only ceased with the use of nonsteroidal anti-inflammatory medication – NSAID (Ibuprofen).
Following the protocol of the mentioned Clinic, the patient had her anamnesis collected, including the description of the main complaint, Current Disease History, Personal History, Family History, Investigation of Dietary and Oral Hygiene Habits, and Harmful Habits (GUEDES PINTO, 2016), allowing for a correct diagnosis of her complaint and screening of other observed intra and extraoral needs based on the data.
During the anamnesis, the guardian reported that at 7 months of gestation, she had concomitant hypertensive peaks with gestational diabetes, which led to a premature birth at 8 months due to cardiac arrhythmias. At one year of age, the patient in question contracted bronchial asthma, requiring a week of medical observation. The patient had food hypersensitivity; however, denied a similar aspect when it came to medications. At the time of the appointment, the child was on vitamin D supplementation. It is extremely important to mention in this report that the patient had harmful habits until the age of 4, using a pacifier and bottle, in addition to clenching her teeth, resulting in mouth breathing, tongue protrusion, and evident anterior open bite.
Regarding the patient’s family history, it was noted that her father and mother were hypertensive, as well as her paternal and maternal grandmothers. Her paternal and maternal great-grandmothers were also hypertensive and diabetic.
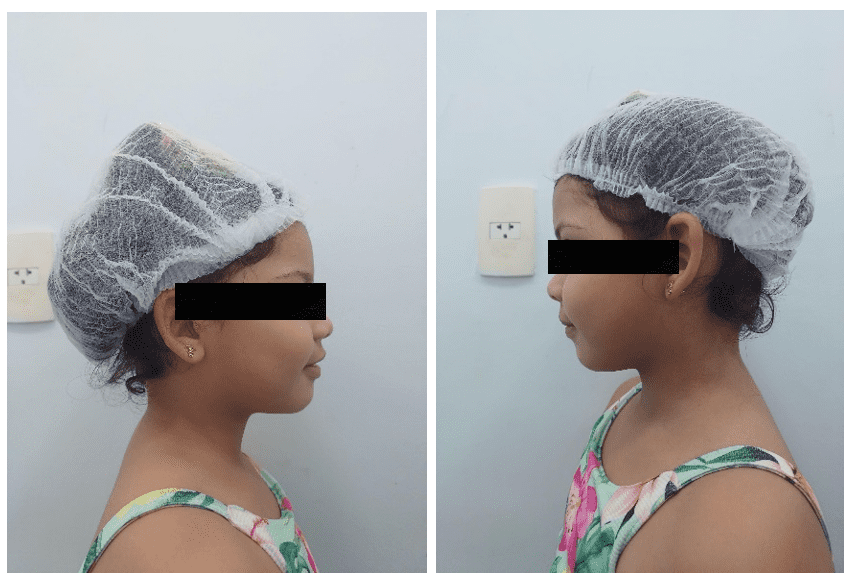
After the anamnesis, a physical extraoral examination of the patient was performed, including inspection of the Temporomandibular Joint (TMJ), palpation of the cervical-facial lymph nodes and sinuses, along with observation and documentation of facial profile and possible maxillary and mandibular misalignments. The child did not have buccal and labial sealing, with lingual interposition due to the sucking habit (Figures 1 and 2).
Figure 1: Convex facial profile – a. Left Lateral View and b. Right

Figure 2: Absence of passive lip seal – Frontal View

During the consultation, her guardian was informed about the need for adherence to the treatment and the diagnosis by a speech therapist aimed at speech adjustment.
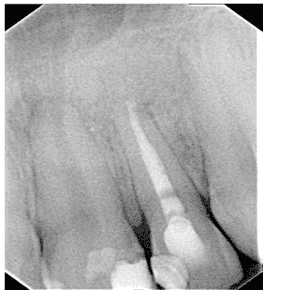
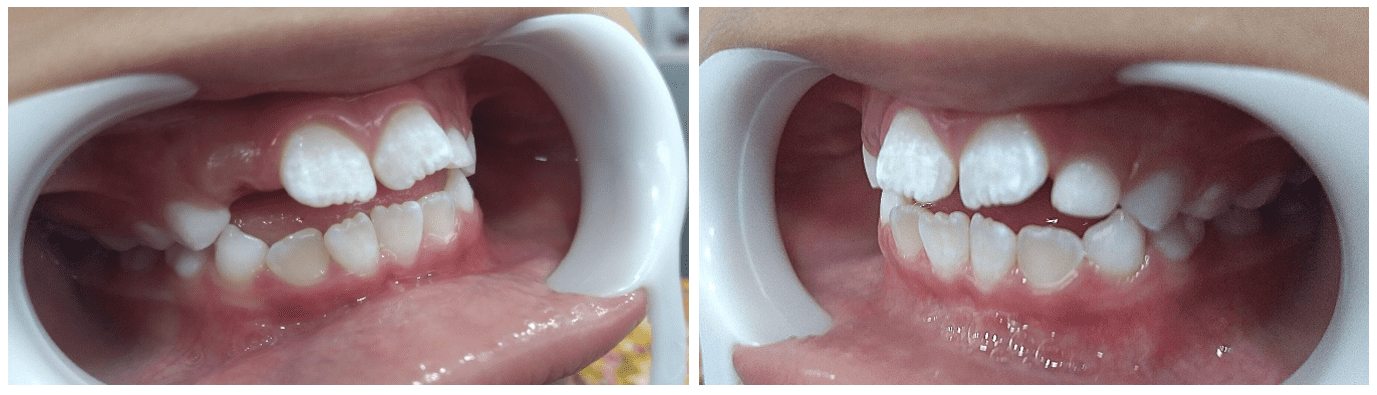
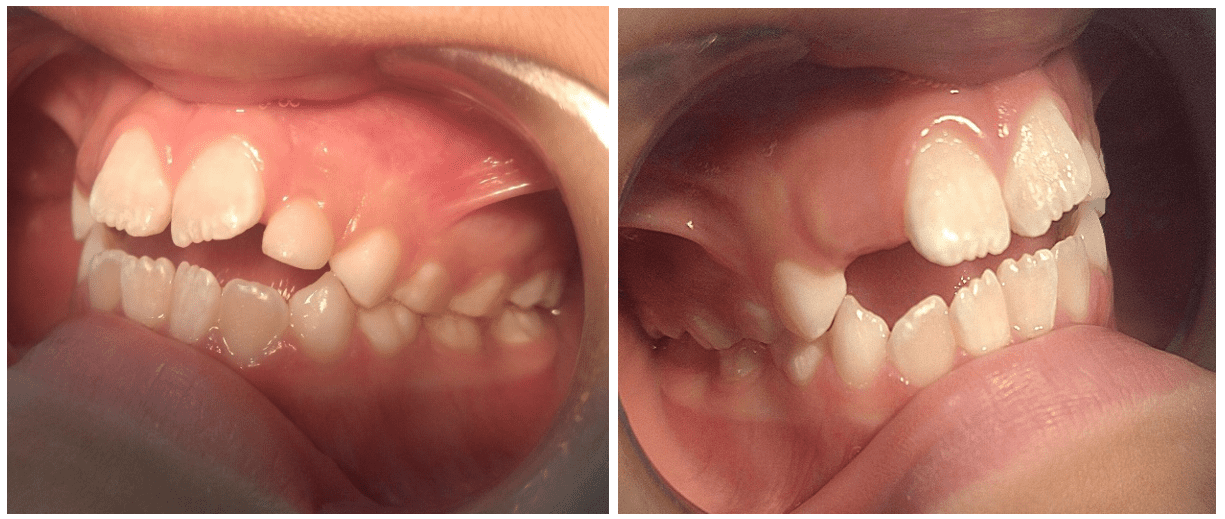
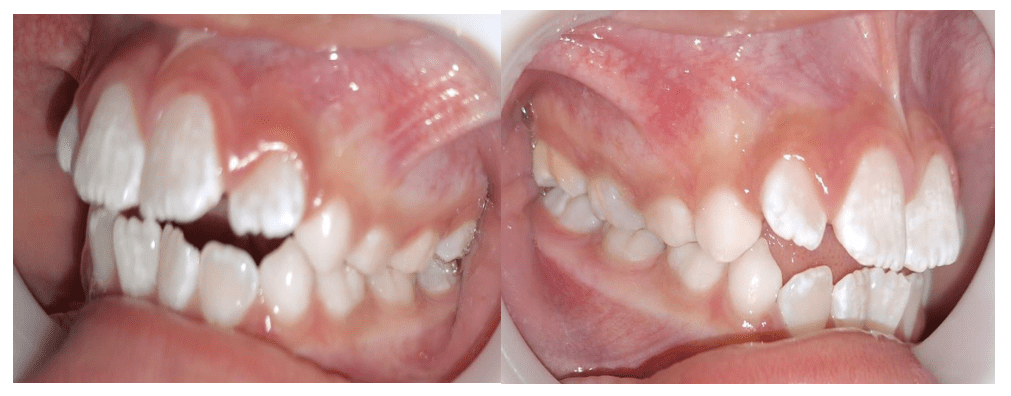
However, no pathological alterations were evidenced during the extraoral examination. In the intraoral physical examination, the soft tissues of the oral cavity were inspected and palpated, and the dental units were directly appreciated, previously cleaned through professional prophylaxis and dried under good lighting. Furthermore, the patient’s occlusion was analyzed, where the first permanent molar was observed in class I, with the mesio-vestibular cusp of the permanent upper first molar occluding in the mesio-vestibular groove of the lower first molar, according to Angle’s classification. It is important to emphasize that this is considered the normal dental relation; however, the presence of anterior open bite was observed from canine to canine, as well as maxillary protrusion in the premaxillary region, atretic palate, buccalization of the upper incisors, rotation, and crowding in the lower incisors region (Figures 3 and 4).
Figure 3: Anterior open bite and tongue interposition – Frontal intraoral view
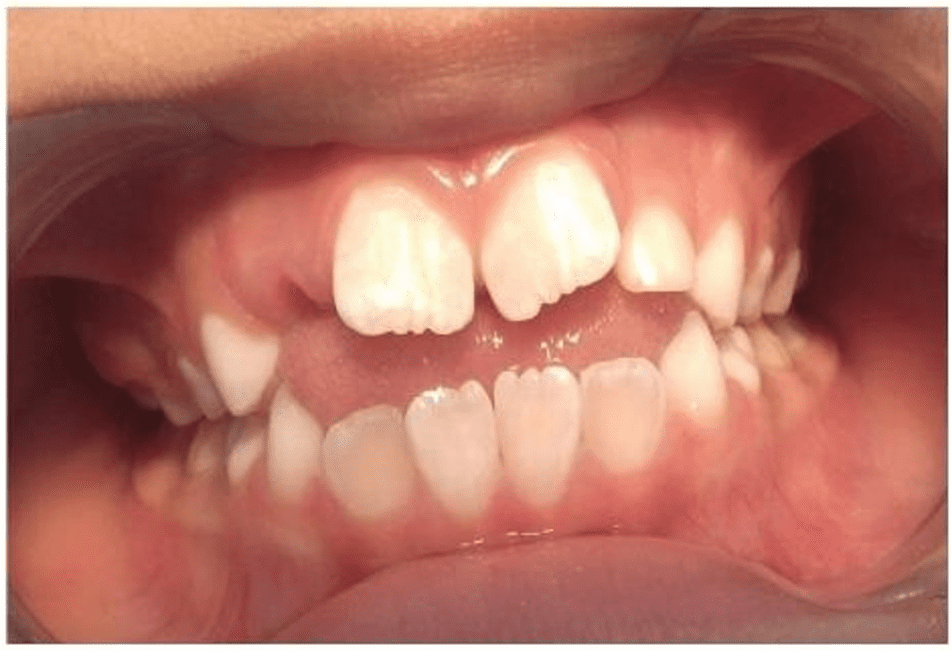
Figure 4: Angle Class I molar relationship – Intraoral Left and Right Lateral View
During this stage, soft tissue alterations and the registration of existing caries lesions, whether cavitated or not, active or inactive, were noted in an appropriate clinical record.
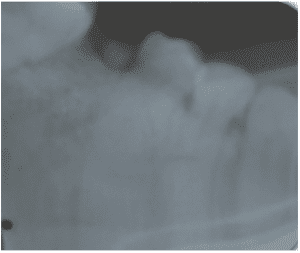
Throughout the treatment, complementary exams were requested: periapical, interproximal, panoramic, and cephalometric radiographs, aiming to assist in clinical diagnosis and support the establishment of the treatment plan for the referred case (GUEDES PINTO, 2016).
Figure 5: Panoramic radiograph showing clinical findings.

With the panoramic radiograph in hand, we were able to observe the strongly evidenced mixed dentition and a radiolucent image suggestive of a caries lesion in tooth 55, as well as the various stages of tooth formation and eruption (Figure 5).
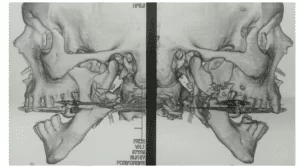
Figure 6: Initial lateral cephalometric radiograph
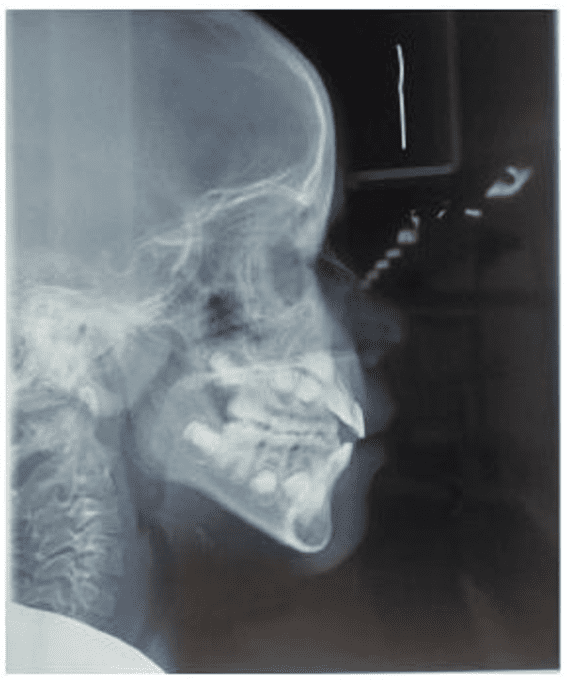
Figure 7: Initial Cephalometric Analysis
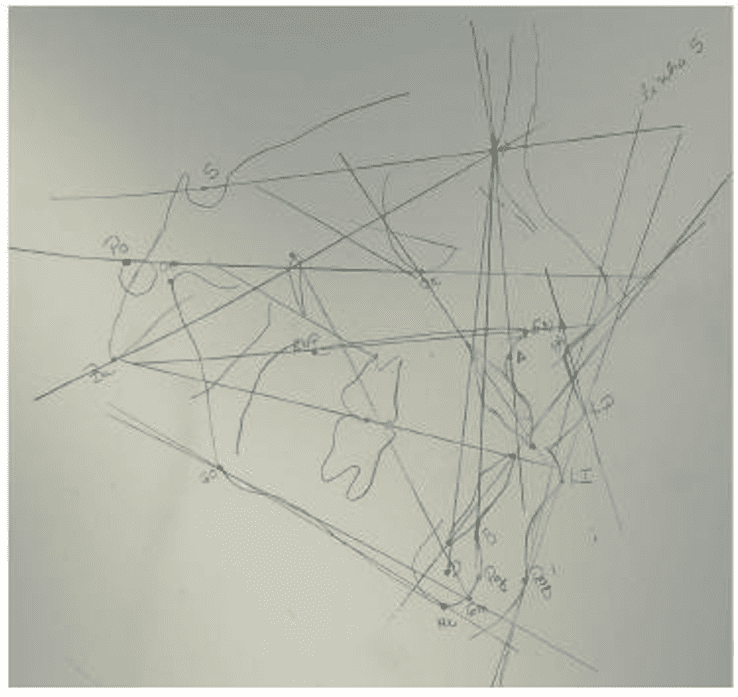
Table 1: Initial Cephalometric Analysis – Usp Standard
| Skeletal Cephalic Pattern | |||
| Measurement | Norm | Patient | Results |
| NS.GoMe | 32° | 32° | Horizontal growth tendency |
| FMA | 25° | 30° | Vertical growth tendency |
| NS.PLO | 14° | 22° | Vertical growth tendency |
| Eixo Facial | 90° | 90° | Normal growth pattern |
| Relation of Apical Bases | |||
| Measurement | Norm | Patient | Results |
| SNA | 82° | 90° | Maxillary Protrusion |
| SNB | 80° | 82° | Protruded Mandible |
| ANB | 2° | 8° | Class II Skeletal |
| FMIA | 68° | 55° | Vestibularization of Incisors |
| Dental Arches X Apical Bases | |||
| Measurement | Norm | Patient | Results |
| 1.NA | 22° | 30° | Upper incisor vestibularization |
| 1-NA | 4mm | 4mm | Upper incisor normal in relation to the skull base |
| 1.NB | 25° | 35° | Lower incisor vestibularization |
| 1-NB | 4mm | 6mm | Lower incisor protruded in relation to the skull base |
| IMPA | 87° | 96° | Lower incisor vestibularization |
| Bone Profile vs. Soft Tissue Profile | |||
| Measurement | Norm | Patient | Results |
| Nasolabial Angle | 95° a 110° | 116° | Upper Lip Imbalance |
| Angle Z | 80° | 73° | Convex Profile |
| Dental Arch Relationship | |||
| Skeletal Class II | |||
Source: Author, 2023.
After studying and discussing the current case, the treatment plan for the patient was defined. It consisted of restoration with glass ionomer cement on tooth 55, impressions, construction, and installation of the Bionator de Balters orthopedic appliance.
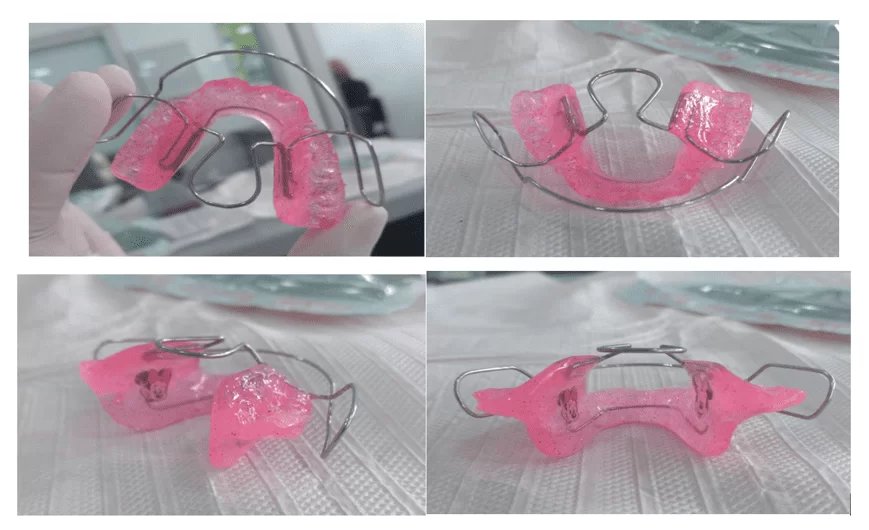
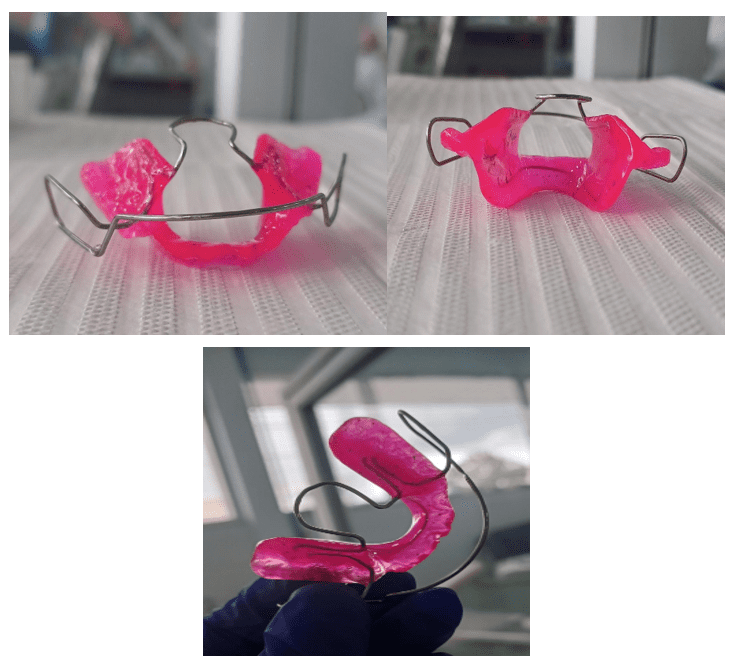
After adapting the oral environment, the functional orthopedic treatment began on September 16, 2022, following the clinical and laboratory steps for making the Class II Bionator de Balters appliance. The goals were to improve maxillary transverse growth, reduce vestibularization of incisors, stop digital suction, resulting in the closure of the open bite, and redirect maxillary and mandibular growth.
The initial clinical steps included selecting pediatric perforated aluminum trays (Tecnodent®, Comercial Vitória Martini, Indaiatuba, SP, Brazil) to ensure proper fit and adaptation to adjacent bone and tissue structures. Anatomical alginate Type I (Hydrogum®, Zermack, Badia Polesine, RO, Italy) was used for anatomical impressions, considering the manufacturer’s recommendations for good dimensional stability, high elasticity, and resistance, albeit with a short working time (around one minute) compensated by a similar setting reaction time, facilitating the obtaining of an adequate study model.
With the anatomical impression in hand, a copy was made for pouring with special Type IV stone plaster (Dent-Mix Asfer®, São Caetano do Sul, SP, Brazil), with manual vibratory movements during gradual insertion of the material into the tray. The choice of this material was based on its good resistance, low expansion, and working time according to the manufacturer, important during model transport to the professional responsible for subsequent laboratory steps.
After obtaining the model, occlusal registration was made using wax No. 7 (Asfer®, São Caetano do Sul, SP, Brazil) to better reproduce the patient’s occlusion during appliance fabrication. After registration, a wax plate was positioned between the two arches of the model, wrapped in plastic wrap for stability and proper positioning. It was sent to a dental laboratory for appliance fabrication, along with a description of its aspects and particularities. The patient was scheduled for a return visit after a week for installation.
One of the attractive features of the Bionator for pediatric dentistry is the possibility for the patient to choose the color, image, and appearance of the appliance, making it more appealing for the user and aiming for greater acceptance of its use.
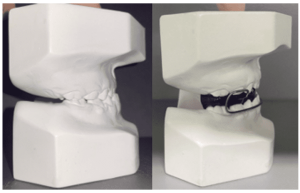
At the appointment scheduled after one week, on September 23, 2022, the installation and activation of the Class II Bionator orthopedic appliance were finally performed. Activation will be repeated throughout the treatment using the Bionator de Balters Class II orthopedic appliance at different mentioned periodic sessions (Figure 8).
Figure 8: First fabrication of the Bionator de Balters Class II Orthopedic Appliance
At the end of the appointment, the guardian was instructed about the activations and their periodicity, to be performed every 3 weeks. They were also informed about the risks if the device was not used correctly, signing a commitment time for the treatment.
At the request of the patient’s guardian, the activation needed to be advanced by a week, occurring two weeks after installation. During this appointment, favorable clinical signs were already noticeable, including the initial closure of the open bite, a slight rotation of the central incisors to return to the midline plane, albeit with evident crowding of the lower incisors. Additionally, there was an initial reduction in buccal inclination of both arches and the reestablishment of initial right and left posterior occlusal contacts, accompanied by appropriate initial canine key displacement (Figures 9 and 10).
One of the key points throughout the process and a significant gain during treatment was the rapid cessation of the sucking habit promoted after the appliance installation. The patient and their guardians strongly adhered to the treatment despite all its limitations, bringing about visible changes in both arches from the first follow-up due to the complete removal of the habit.
Figure 9: Initial closure of the open bite and improvement in incisor rotation – Intraoral Frontal View

Figure 10: Improvement of the canine key – Left and Right Intraoral Lateral View
After five weeks from the installation of the appliance, the patient returned for the second activation on November 28, 2022. Continuing, it was observed that the treatment experienced a slight setback in closing the mouth due to the discontinuation of Bionator use, caused by the appearance of localized gingival erythema due to intimate contact of the mucosa with the buccinator loop. However, it was still possible to observe the maintenance of some aspects in the initial maxillomandibular correction, along with molar interposition (Figures 11 and 12).
Figure 11: Maintenance of bite closure and canine key compared – Intraoral Frontal View
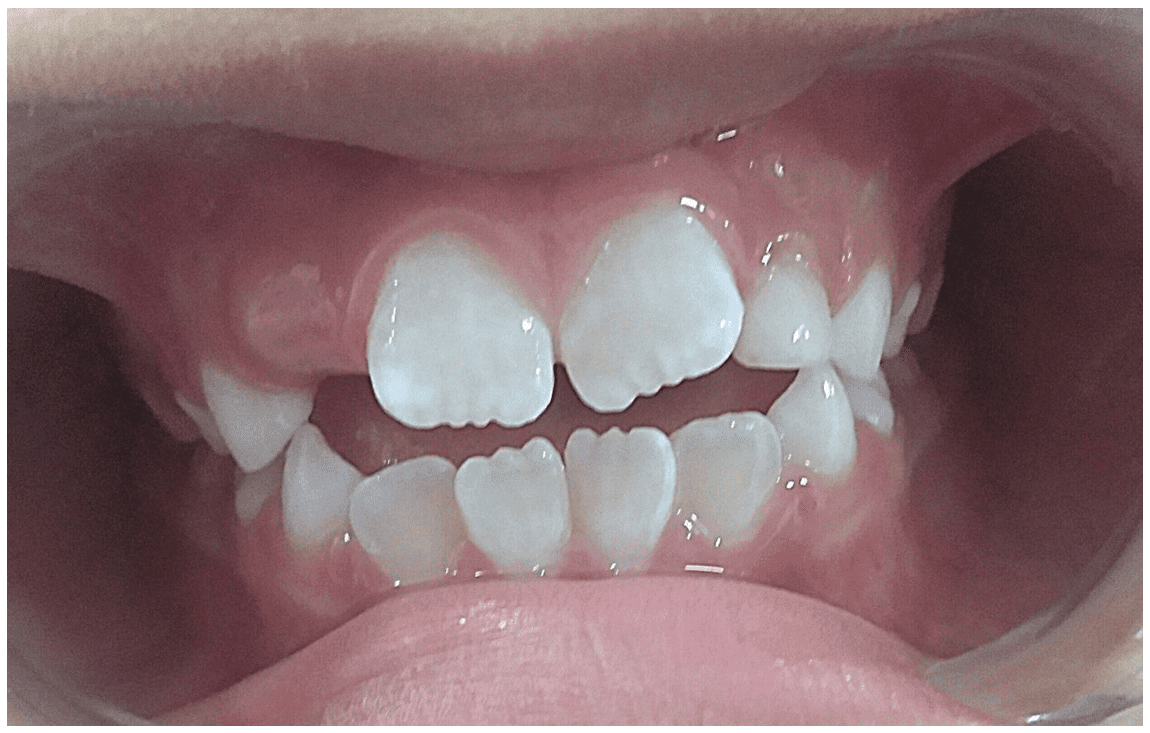
Figure 12: Maintenance of molar interposition – Right and Left Intraoral Lateral View
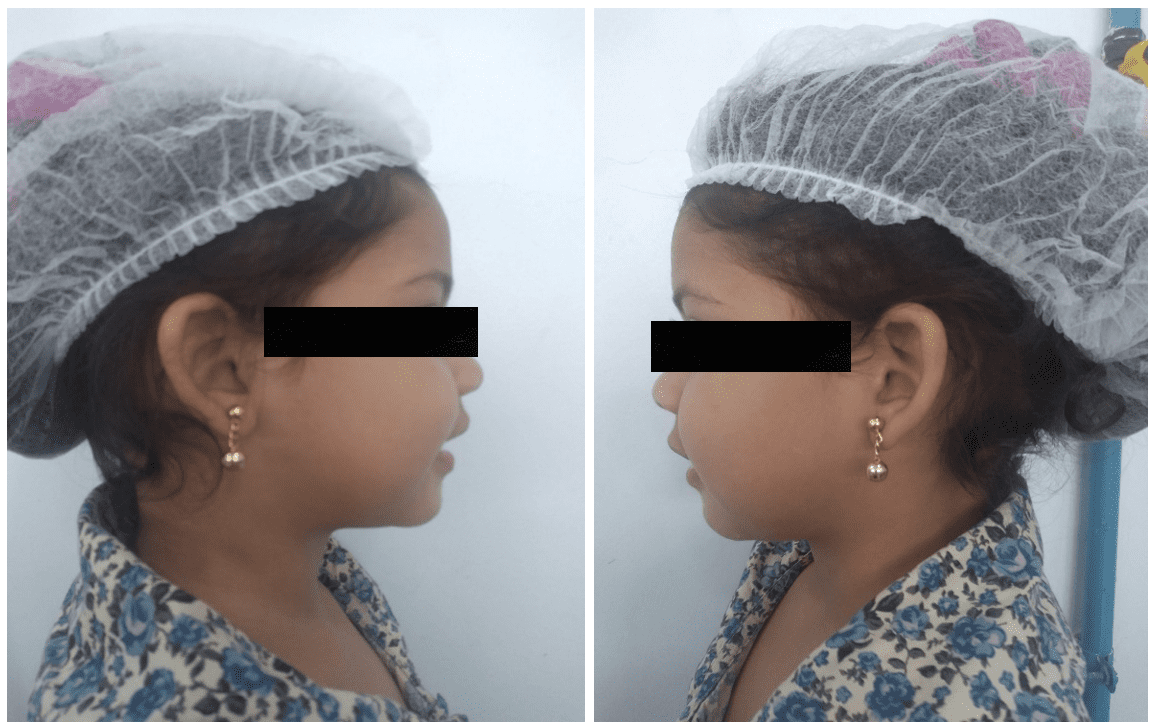
During the consultation, it was also noted the loss of part of the restoration of tooth 55 due to occlusal contact with the acrylic of the appliance, necessitating the repair of the restoration, leaving it in infraocclusion, and the acrylic was trimmed with tungsten maxicut (American Burrs®, Cidade Universitária Pedra Branca, Palhoça, SC, Brazil) and straight handpiece, respecting the occlusal plane, ending with the new facial registration of the patient, totaling 7 weeks of use (Figure 13).
Figure 13: Maintenance of the convex facial profile – Right and left lateral view
Eleven weeks later, she returned for the 3rd activation of the appliance on November 25, 2022, where a significant progression in closing the anterior open bite and improvement in incisor giroversion, correct canine key was observed.
There was also an advancement in the eruption of tooth 12, in addition to maintaining the adequate occlusion of the posterior teeth and the absence of tooth 62 (Figures 14).
Figure 14: Significant progression in closing the anterior open bite and advancement in the eruption of tooth 12 – Frontal intraoral view

Due to the university’s vacation period, patients seen during the course of this time are rescheduled for the beginning of a new cycle of clinical appointments, considering that the university caters to a large local demand; therefore, rescheduling or rebooking old patients often proves to be quite challenging, unfortunately, this was the case with the mentioned patient. Additionally to internal obstacles at the clinic, there were also family problems on the patient’s side, causing the timing of activations to not adhere to the established 3-week intervals.
It’s important to emphasize that a treatment plan is outlined by the responsible professional; however, it’s the full responsibility of the legal guardian to adopt and comply with the established and pre-determined appointment days. Nonetheless, reality differs significantly from what we envision, unexpected events and setbacks arise from parents and from our workplace, often delaying and altering the routine appliance check-ups, consequently postponing the results.
On March 1, 2023, the patient returned to the university, now totaling 29 weeks since the appliance installation, where she was assisted to complete the remaining activations.
During the appointment, it was possible to observe consistent usage within the period that she was under supervision. This underscores the need and the difference that commitment to treatment makes by the legal guardians of the patient.
A significant closure of the anterior open bite was observed, with a strong approximation of adjacent incisal edges, eruption of teeth 12 and 22, achieving adequate space in the arch during eruption. When viewing both arches laterally, we saw a satisfactory occlusion of posterior teeth, appropriate canine key, and the initiation of a reduction in incisor vestibularization. However, it is necessary to emphasize that the latter mentioned characteristic will only succeed with the implementation of other future therapeutic methods (Figures 15 and 16).
Figure 15: Closure of the anterior open bite, eruption of teeth 12 and 22 – Frontal intraoral view
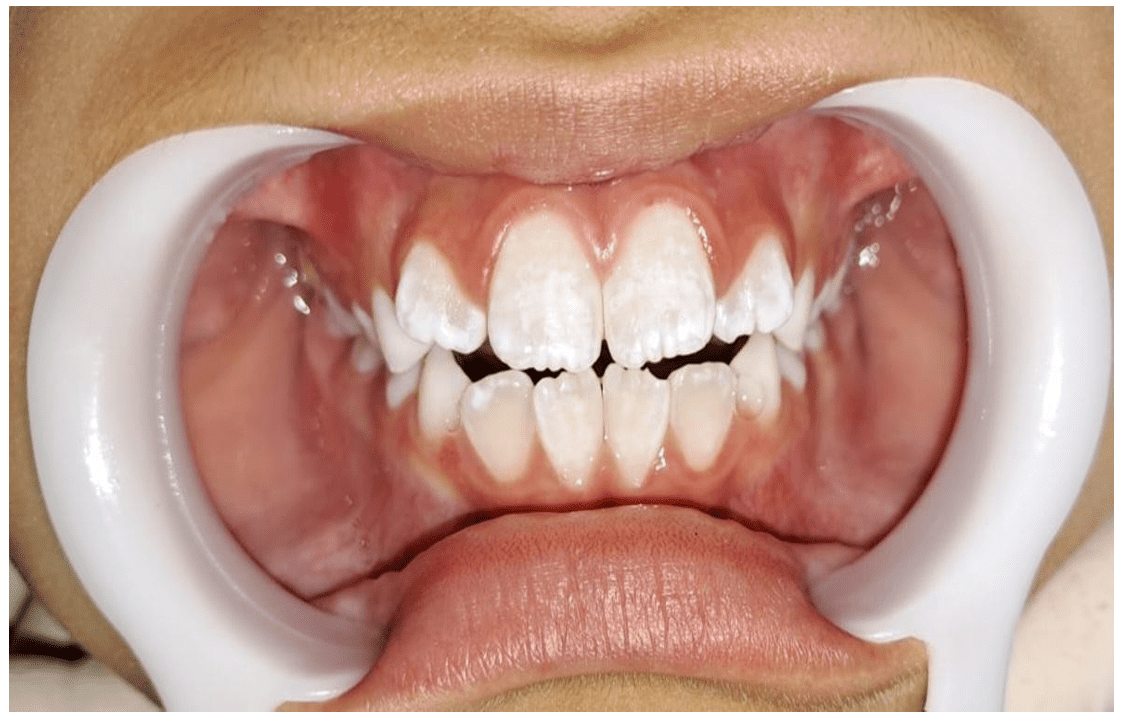
Figure 16: Satisfactory molar relationship, appropriate canine key, beginning of the reduction of incisor vestibularization – Intraoral Right and Left Lateral View
The patient complained of a small ulcerated erythematous area near the sulcus base, although it did not bother her during the fitting of the appliance. Upon evaluation, it was concluded to be a recurrent aphthous stomatitis, which regressed without the need for any therapeutic intervention.
During this same appointment, a new facial radiographic image was taken, now showing easily evident results, such as the nasolabial angle now less pronounced within normal standards, in harmony with the other facial structures, both in a position of passive lip seal and during minimal or evident contractions (Figure 17).
Figure 17: Passive lip seal, without contraction of the lip musculature – Right and Left Lateral View
After the consultation and necessary records, a new impression was taken to make a new Class II Balters Orthopedic Bionator appliance, considering the patient’s facial growth and the bone and dental displacement caused by the previous appliance. The procedure for the new appliance was identical to the first, using the same materials and following the handling methods described at the beginning of this report.
At the end of the last mentioned appointment, a lateral cephalometric radiograph was requested to monitor the case.
One week later, on March 8, 2023, totaling 30 weeks since the installation of the first fabricated appliance, the patient returned for the installation of the new Class II Balters Orthopedic Bionator appliance, now adjusted to the dento-skeletal changes that occurred during the treatment with the initial Bionator. (Figure 18)
Figure 18: Second fabrication of the Class II Balters Orthopedic Bionator appliance
With the appliance in hand and adjusted in the patient’s oral cavity, it was observed that the buccal loop was in infraocclusion, a common error during the making of this type of appliance, which can be easily adjusted using orthodontic pliers n°139 (Angle Bending Golgran®, São Caetano do Sul, SP, Brazil), pulling the buccinator loop and raising the buccal loop to the mid-third of the anterior elements of the upper arch from canine to canine (Figures 19 and 20).
Figure 19: Frontal intraoral view of the new functional orthopedic appliance Bionator by Balters in the mid-third region of the upper elements, from canine to canine after adjustment
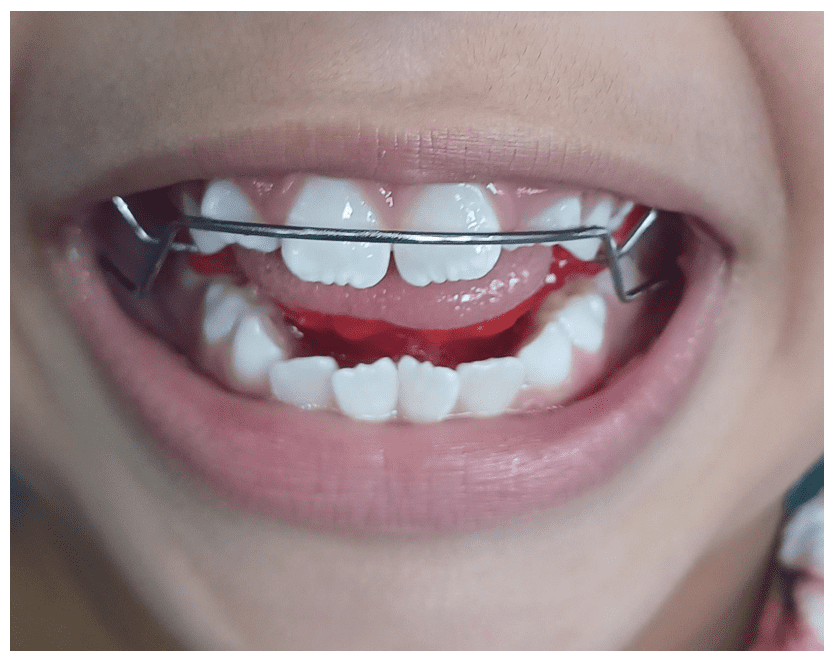
Figure 20: Frontal view of the patient wearing the appliance after fabrication, installation, activation, and adjustment

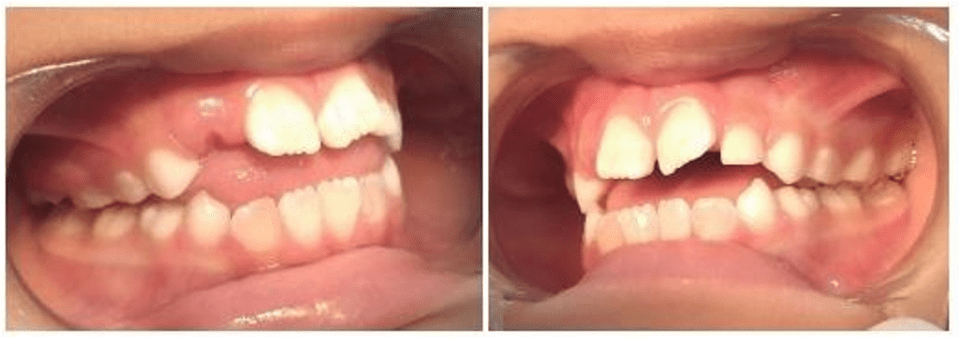
On May 5, 2023, the patient attended for the last time for the purpose of documenting this case report, along with final radiographs, totaling 44 weeks of monitoring and tracking dentoskeletal changes. Clinically, changes were observed in the canine fit, bite closure, and improvement in maxillary protrusion, in addition to the mother’s report that the habit of digital suction was no longer present (Figures 21 and 22).
Figure 21: Initial and final photographs of functional orthopedic treatment with the Bionator appliance by Balters, demonstrating bite closure, improved maxillary protrusion with absence of digital suction, decreased tongue projection, and reduced incisal crowding compared to the initial state

The patient’s facial profile showed significant improvement in the symmetry of the structures, especially in the nasolabial angle, achieving a well-advanced and harmonious range within normal standards (Figure 23).
Figure 22: Convex profile with symmetrical facial structures, nasolabial angle within normal standards – Right and Left Lateral View

Figure 23: Final Lateral Cephalometric Radiograph
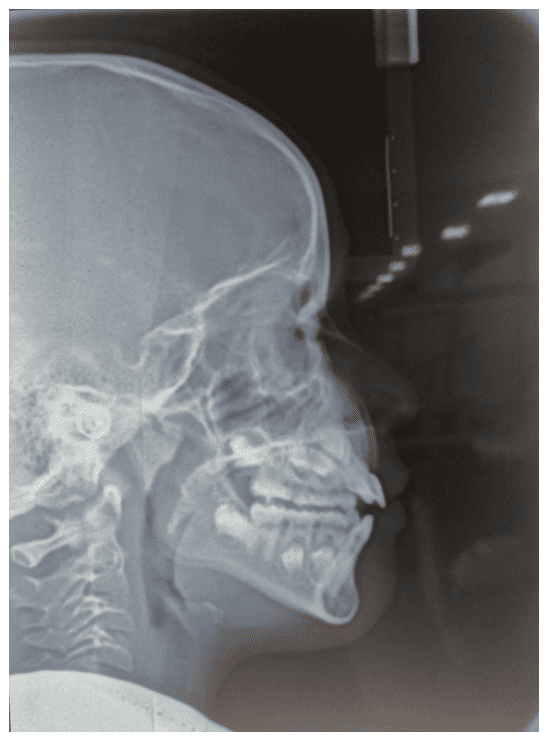
Figure 24: Final Cephalometric Analysis
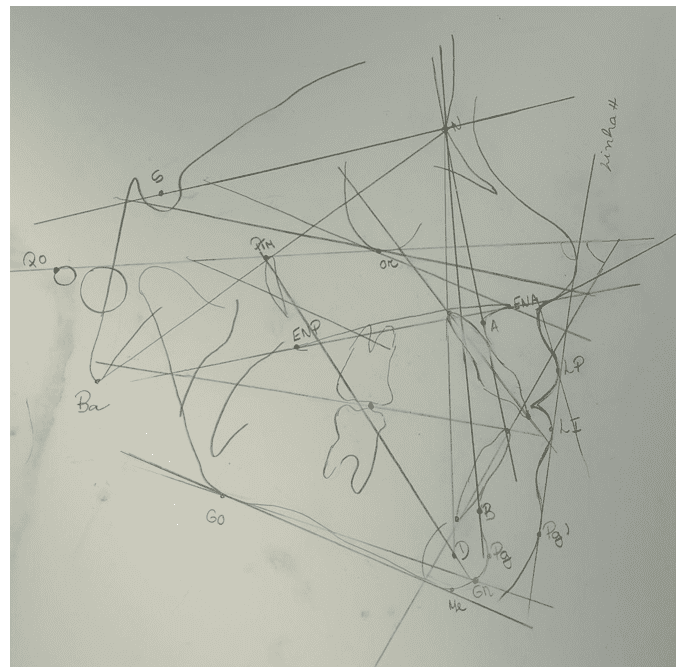
Table 2: Comparison Table of Cephalometric Analysis – Cranial Skeleton Standard
| Cranial Skeleton Standard | |||
| Measurement | Initial | Average | Final |
| SN.GoMe | 35° | 32° | 37° |
| FMA | 30° | 25° | 29° |
| NS.PLO | 22° | 14° | 25° |
| Facial Axis | 90° | 90° | 88° |
| Relation of Apical Bases | |||
| Measurement | Initial | Average | Final |
| SNA | 90° | 82° | 90° |
| SNB | 82° | 80° | 83° |
| ANB | 8° | 2° | 7° |
| FMIA | 55° | 68° | 59° |
| Dental Arches vs. Apical Bases | |||
| Measurement | Initial | Average | Final |
Source: Author, 2023.
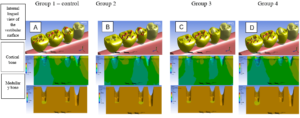
We compared the cephalometric measurements obtained using the Balters Class II Bionator appliance from its installation and activation during the course of treatment. We compared the initial and final cephalometric data through point, line, and plane records with their angulations in the orthodontics laboratory at the Federal University of Amazonas – UFAM, using a light box (Essence Dental®, Slim Led, Araraquara, SP, Brazil) and Ultrafun cephalometry paper (American Orthodontics®, Ultrafun, Sheboygan, WI, USA), providing visualization of the smallest details to be studied. This was followed by cephalometric measurements evaluating maxillo-mandibular relationships, vertical analysis, dental pattern analysis, profile analysis, cephalometric discrepancy, and airways, guided by current anatomical structures and based on facial analyses (Figures 6, 7, 24, and 25).
The angle formed by the lines SN and NA (SNA) indicates the anteroposterior position of the maxilla relative to the cranial base: the treated patient had a value of 90° in both analyses, with an average value of 82°, showing an 8° deviation, diagnosed as maxillary protrusion. In the analysis of the angles formed by the lines SN and NB (SNB), the anteroposterior position was shown, with initial values of 82°, demonstrating a standard deviation, and a final value of 83°, compared to the reference value of 80°, showing an initial mandibular protrusion due to bone movement with a positive effect towards its correction, which is one of the main functions of the Bionator.
Through the angle formed by the intersection of lines NA and NB (ANB), we represent the maxillomandibular relationship anteroposteriorly; in this case, the NB line was found behind the NA line, based on an average of 2°, with an initial positive value of 8° and a final value of 7°, demonstrating a minimal reduction, but already present after orthopedic treatment in the patient’s Class II skeletal case.
The angle (SN.GoMe) represents the inclination of the mandibular plane relative to the anterior base of the skull and shows the tendency for vertical growth of the patient. Initially, it was 35°, based on its average of 32°, ending with 37°. Based on these data, it was evaluated that after the treatment, there was an increase in the tendency for vertical growth of the patient.
During the results collection, attention was given to the angle formed by the intersection of the BaN line with PtGn (Facial Axis), which showed a decrease at the end, with 88°, considering an average of 90° when compared to the initial 90°, resulting in an analysis indicating a tendency for vertical growth, classifying it as a Type 3 profile – Dolichofacial, with a short midface aspect with predominance of vertical distance, still showing facial patterns corresponding to malocclusion.
The analysis of the angle formed by the long axis of the upper incisor with the NA line (1.NA) indicates the axial inclination of the patient’s teeth in relation to the skull base. In the collected results, an initial and final balance of 30° was found, referenced by the established value of 22°, showing that the upper incisors are still vestibularized, which is very common in cases with Class II skeletal malocclusion, first division, observed in the patient in question, i.e., her incisors remain vestibularized. Referring to the upper incisors, data on the linear measurement from the most vestibular point of the crown to the NA line (1-NA) were collected, with initial values within the normal range proposed by the USP standard of 4mm, and a final value of 5mm, deviating from the average and demonstrating protrusion of the upper incisors in relation to the skull base after treatment.
When analyzing the angle formed by the intersection of the long axis of the lower incisor with the NB line (1.NB), a measurement of 35° was initially observed, which persisted until the end, showing the continued vestibularization of the lower incisors post-treatment, considering its average value of 25°. In the case of the distance from the most vestibular portion of the crown of the lower incisor to the NB line (1-NB), we assessed if there was protrusion of the lower incisors through the average value of 4mm; in the report of the patient in question, the corresponding values persisted at 6 mm both initially and finally, maintaining the protrusion of the lower incisors in relation to the skull base.
Through the angle formed by the intersection of the long axis of the lower incisor with the GoMe mandibular plane (IMPA), it is possible to indicate the axial inclination of the lower incisors in relation to the patient’s mandible, which remained at 86° until the end of the intervention, considering the reference parameter of 87° and indicating vestibularization of the same. These measurements will serve as a parameter in her future treatment plan for the attempt to accommodate the crowded teeth, promoting correct implantation in their bone bases.
When we turn to the analysis of the patient’s nasolabial angle, we must first understand the angle and its formation by the LsSn lines with SnCm, allowing the indication of the degree of protrusion of the patient’s upper lip, with reference values of 95° to 110°, compared to the initial value of 116° and final value of 113°, leading to an improvement in the balance of the upper lip in relation to the patient’s profile in a more harmonious profile.
Analyzing the angle formed by the profile line with the Frankfurt horizontal plane (Z angle), the improvement in the patient’s profile is confirmed. It is important to understand that this line is defined by the most anterior portion of the soft tissue of the chin (Pg) with the most anterior portion of the most protruding lip. Its average value is 80°, with initial records at 73° and final records at 79°, with a difference of 6°. Considering its deviation from the standard, with a larger discrepancy of 5°, a convex profile is evident, when compared to the end of the treatment, already showing significant change and leaning almost entirely towards the standards of a straighter profile.
Regarding the FMIA angle, we understand that its formation occurs through the Frankfurt plane and the long axis of the lower incisor. Initial data of 55°, compared to final data of 59°, within an average of 68°, resulted in a decrease in the vestibularization of the incisors.
It is important to highlight the increase in airspace in the oropharyngeal region due to lingual rest acquired during the primary removal of tongue projection, observed in lateral cephalometry when compared (Figures 6 and 24).
Based on the final findings, the patient was referred to the next phase of her treatment, in conjunction with a speech therapist, and the performance of new complementary exams, in order to outline her needs and guide us regarding the new appliance to be installed in the future. The pediatric patient will continue to receive dental care at FAO-UFAM.
3. RESULTS AND DISCUSSION
Malocclusion is a public health issue; hence, the need for more studies to emphasize the importance of early treatment and the removal of oral habits (ARAÚJO et al., 2023).
The case report described in this study involves functional orthopedic treatment with the Balters Class II Bionator appliance, in a Class I molar key patient according to Angle’s classification and Class II skeletal, with the relevant data evidenced through lateral cephalometry, by measuring the ANB angle. There are various appliances available in the market for the treatment of malocclusions, and their indications are what specifically guide the choice for a particular case. In the case presented, the diagnosis of anterior skeletal disharmony and digital sucking habit, with consequent mouth breathing, highlighted the need for the orthopedic appliance (ARAÚJO et al., 2023).
Different case reports on the therapeutic approach used in this study strongly reinforce the need for study over the years, considering dental characteristics, timing, and treatment methods (PAKSHIR et al., 2017). Despite the satisfactory number of studies in the scientific field on malocclusions and their causes, especially concerning case reports, a greater number of publications are still needed regarding the use of Balters Bionator and its results, in the short and long term, as authors still significantly diverge on the number of hours the Balters functional orthopedic appliances should be used and their results, having only one parameter that can vary between 12-22 hours, according to the practicing professional, with removal only during hygiene.
Children between 6 and 7 years old, like the patient in the study, with an established malocclusion, should always be evaluated for the need for orthodontic treatment with removable or fixed functional orthopedic appliances, allowing an improvement in occlusal disharmony (JUNGBAUER, 2023).
The use of the Bionator appliance, when compared to others, such as the lingual bar, has been shown to be more effective in closing open bites (MOUSA et al., 2021).
When compared to the use of Herbst, aiming for dentoskeletal correction, in aspects such as a significant decrease in the width of the lower arch, width of the upper and lower arch, as well as sagittal molar relationship, they are equivalent (BOCK et al., 2023).
Palatal cribs, which are also a way of containing lingual projection, would not be highly indicated in this case, precisely due to the significant number of dental and skeletal anomalies that require correction, as mentioned earlier. This necessitates a more careful and comprehensive intervention, aiming to rehabilitate not only one of the factors that led to this condition but the entire context that requires rehabilitation, where the palatal crib is not one of the most indicated appliances due to its rigidity, differing from the Bionator, which is movable and allows a broader change in the entire dento-muco-skeletal structure (ARAÚJO et al., 2023).
According to Ahmadian-Babaki et al. (2017), another option for treating malocclusions can be through the use of Twin Block appliances. However, when used, they have less effect on the angle of the upper incisor to the palatal plane, which is a strong effective indicator of dentoalveolar changes, making the Bionator again the better option, generating greater action on the incisors in this investigation. Another appliance frequently used and compared to the one used in the case at hand is the Farmand Appliance, similar to the one applied to the patient in this report but with some different specificities, consisting of a labial arch in each dental arch, two supports or stops on the first permanent molars, a lingual arch, and an acrylic plate. Both the Farmand and the Bionator improve the intermaxillary discrepancy in patients with malocclusion; however, the latter has greater specificities regarding repositioning the mandible more anteriorly, restoring overjet and overbite, controlling tooth eruption, and improving facial structures (PAKSHIR et al., 2017).
Given the techniques used in the treatment, it was possible to confirm that anterior open bite is one of the biggest challenges for orthodontists; this malocclusion is still widely discussed due to its multifactorial origin and its significant importance to patients from an aesthetic standpoint (ANTOUN et al., 2008). In the present case, the anterior open bite was strongly established due to the presence of deleterious oral habits and consequent lingual projection, occurring over a long period, with an absence of adequate vertical overlap between the upper and lower incisors. Its correction is indeed challenging, for various reasons: one of the main reasons is the need for responsible adoption of the appliance’s use, considering that the user is a minor, often lacking the understanding of their needs, necessitating a third party, usually their guardian, to supervise the treatment protocol (ARAÚJO et al., 2023).
We observed that the open bite is mainly caused by deleterious oral habits (ARAÚJO et al., 2023), along with the epigenetic tendencies of the patient in vertical growth, i.e., with the presence of digital suction, this reaction was aggravated, observed initially and confirmed through the initial and final cephalometric analyses. In a scenario where the patient did not have vertical tendencies, it would not be possible to evidence such growth in the final analysis; however, the suction habits would significantly hinder the patient’s normal vertical growth tendencies. Even after removing the habit, it would still be possible to observe this vertical growth, as it occurs due to normal growth tendencies. However, by persisting with the habit, these tendencies are projected and emphasized further. We also observed through cephalometric analysis that there was an increase in the oropharynx, with a consequent decrease in mouth breathing by the child, in agreement with Araújo’s studies (2023).
Regarding the treatment and prognosis of the malocclusion in this study, a series of factors and approaches must be considered, including precise and individualized diagnosis, appliance selection, and prescription, i.e., how many hours the appliance was used per day, as well as the skill in managing these types of cases in the clinical setting (ARREGHINI et al., 2017). The treatment results were satisfactory and led to improved posterior intercuspation, reduced overjet and overbite, and anterior functional guidance free of interferences, similar to other described case reports (RÉDUA, 2020). In the present study, due to habit removal and appliance use, the vertical and horizontal overlaps of the patient improved, resulting in bite closure. However, it is still progressing due to the eruption of permanent teeth with evident replacement of the elements, requiring follow-up and replanning of future treatment.
The overlap of the initial and final cephalometric tracings revealed good mandibular growth in a favorable direction. One of the findings in this case, involving facial parameters, was that functional appliance therapy increased the dimensions of the pharyngeal airways in a growing patient, and this finding was maintained until growth completion, according to the evidence (HAN et al., 2014, RÉDUA, 2020).
This study contradicts other reports that indicated no significant change in the maxillary component with the use of Balters’ Bionator and confirmed a significant increase in maxillary length, with the upper incisors showing stable vestibular inclination and the lower incisors with a slight labial inclination and stable protrusion (FRANCISCONI et al., 2013). One of the points strongly discussed by Santos-Pinto et al. (2013) is the significant skeletal growth in relation to all analyzed points, demonstrating dentoalveolar modifications.
By observing 120 lateral cephalometric radiographs, a tangent line was established to the soft mentum and the more protruded lip, whether upper or lower, until it reached the horizontal plane of Frankfurt, forming angle Z. An average value of 80° was obtained for adults and 78° for individuals between 11 and 15 years old, indicating individuals with a harmonious profile. In this clinical case, we observed an improvement in the patient’s profile, evaluating both the nasolabial angle and angle Z. The patient’s nasolabial angle increased, demonstrating a decrease in the protrusion of the upper lip, and the Z angle increased, indicating that the patient’s convex profile observed at the beginning of the treatment changed to a more straight and harmonious profile.
4. CONCLUSION
Based on the above, it can be concluded that:
Dental malocclusion is a public health issue, requiring early attention in the clinical setting; thus, a correct diagnosis and individualized treatment plan are essential to prevent more severe future occlusal disharmony and the implementation of more invasive therapeutic procedures in the future;
The use of Balters’ Bionator Class II Appliance proved to be effective during the mixed dentition phase, leading to occlusal harmony and the removal of deleterious habits, such as digital sucking; however, commitment from the caregivers is necessary to achieve adequate patient adherence throughout the treatment.
Cephalometric tracings allow and facilitate proper case monitoring, generating an excellent understanding of future treatment needs and the current state of the dentoskeletal relationship.
REFERENCES
AHMADIAN-BABAKI F. et al. A Cephalometric Comparison of Twi d Bionator Appliances in Treatment of Class II Malocclusion. J Clin Exp Dent, v.9, n.1, p.107-111, 2017.
AKSU M. et al. Assessment of upper airway size after orthopedic treatment for maxillary protrusion or mandibular retrusion. Am J Orthod Dentofacial Orthop, v.152, n.3, p.364-370, 2017.
ANTOUN T. R. A., et al. Mordida aberta anterior na dentição permanente – relato de caso. Rev. Odontol. Univ. Cid. São Paulo, v.30, n.2, p.190-199, 2008.
ANTUNES C.F. et al. Morphometric analysis of treatment effects of the Balters bionator in growing Class II patients. Angle Orthod, v. 83 n.3, 2013.
ARAUJO P. P. B. N., ARANHA R. P. Avaliação de medidas cefalométricas angulares para análise da tendência de crescimento vertical e ângulo Z em uma amostra de pacientes com oclusão normal. Revista Científica Multidisciplinar Núcleo do Conhecimento, v.01, n.06, pp. 44-53, 2023.
ARREGHINI, A. et al. Objective assessment of compliance with intra- and extraoral removable appliances. Angle Orthod, v.87, n.1, p.88-95, 2017.
BATISTA K.B. et al. Orthodontic treatment for prominent upper front teeth (Class II malocclusion) in children and adolescents. Cochrane Database Syst Rev, v.133, n.3, 2018.
BIGLIAZZI R. et al. Morphometric analysis of long-term dentoskeletal effects induced by treatment with Balters bionator. Angle Orthod, v.85, n.5, p.790-8, 2015.
BOCK N.C. et al. Long-term (≥ 15 years) outcome quality after Class II:1 bionator or Herbst multibracket appliance treatment: A comparison. J Orofac Orthop, v.24, 2023.
FRANCISCONI M. F. et al. Stability of Class II treatment with the Bionator followed by fixed appliances. Journal of Applied Oral Science, v.21, n.6, p.547–553, 2013.
HAN S. et al. Long-term pharyngeal airway changes after bionator treatment in adolescents with skeletal Class II malocclusions. Korean J Orthod. v.44, n.1, p.13-9, 2014.
JUNGBAUER R. et al. Twenty-year follow-up of functional treatment with a bionator appliance (part 2): a retrospective cephalometric analysis of skeletal and dentoskeletal changes. Angle Orthod. v.93, n.3, p.269–74, 2023.
LANDÁZURI D. R. G. et al. Changes on facial profile in the mixed dentition, from natural growth and induced by Balters’ bionator appliance. Dental Press Journal of Orthodontics, v.18, n. 2, 2013.
MENDES S.L. et al. Risk factors for anterior open bite: A case-control study. Dent Res J (Isfahan), v.17, n.5, 2020.
MOUSA M. R. et al. Avaliação da mordida aberta Bionator versus o plano de mordida posterior removível com berço lingual no tratamento precoce da mordida aberta anterior esquelética: um estudo controlado randomizado. Jornal da Federação Mundial de Ortodontistas, V.10, n.4, p.163 – 171, 2021.
PAKSHIR H. et al. Effect of Bionator and Farmand Appliance on the Treatment of Mandibular Deficiency in Prepubertal Stage. Turk J Orthod, v.30, n.1, p.15-20, 2017.
RÉDUA R. B. Different approaches to the treatment of skeletal Class II malocclusion during growth: Bionator versus extraoral appliance. Dental Press Journal of Orthodontics, v.25, n.2, p.69–85, 2020.
[1] Dental undergraduate student. ORCID: 0009-0003-0477-2614. Currículo Lattes: http://lattes.cnpq.br/1977203311524825.
[2] Dental undergraduate student. ORCID: 0009-0001-8398-2390. Currículo Lattes: http://lattes.cnpq.br/7301946389987967.
[3] Dental undergraduate student. ORCID: 0009-0003-8461-6338. Currículo Lattes: http://lattes.cnpq.br/1832010931426679.
[4] Dental undergraduate student. ORCID: 0009-0001-1734-8455. Currículo Lattes: http://lattes.cnpq.br/8709140095376311.
[5] Advisor. Updates in Pediatric Dentistry, Laser Therapy qualification, Advanced training in Orthodontics and Functional Jaw Orthopedics, Specialization in Public Health and Orthodontics, Master’s in Orthodontics, PhD in Orthodontics. ORCID: 0000-0002-5514-0911. Currículo Lattes: http://lattes.cnpq.br/1678395879499706.
[6] Co-advisor. Ph.D. ORCID: https://orcid.org/0000-0002-3415-8557. Currículo Lattes: http://lattes.cnpq.br/9360379216723532.
Submitted: July 28, 2023.
Approved: August 10, 2023.