ORIGINAL ARTICLE
SILVA, Agnaldo Plácido da [1], PLÁCIDO, Eloá Jessica Mendes dos Santos [2], SILVA, Gustavo Henrique Ramos da [3]
SILVA, Agnaldo Plácido da. PLÁCIDO, Eloá Jessica Mendes dos Santos. SILVA, Gustavo Henrique Ramos da. Bilateral comminuted mandible fracture by firearm: A clinical case report. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year 05, Ed. 11, Vol. 17, pp. 05-13. November 2020. ISSN: 2448-0959, Access Link: https://www.nucleodoconhecimento.com.br/dentistry/firearm, DOI: 10.32749/nucleodoconhecimento.com.br/dentistry/firearm
SUMMARY
The mandibular fracture has as its most common causes car accidents, physical aggressions, falls and accidents in the removal of teeth, among others. However, facial injuries caused by firearms are still a cause of great health concern, which can cause great aesthetic and functional damage to the patient, in addition to the loss of quality of life. The therapeutic choice for treatment will depend on the severity of the case and mastery of the technique chosen by the professional. The aim of this article is to report the treatment of a patient with bilateral fracture of the body and mandible branch, resulting from aggression by firearm projectile. Having as treatment established the extraoral access with installation of plates and screws 2.0 mm on the right and left side, because it is a good treatment option for comminuted fractures caused by firearm projectile, returning to the patient aesthetic, functional and psychological aspect.
Keywords: Fracture fixation, gunshot wounds, mandibular fractures, oral surgery.
INTRODUCTION
“The mandible presents itself as the only mobile bone of the facial skeleton, being articulated with the head through two joints; it has horseshoe shape, in which there is a resistant central area, being weaker at its ends” (SIQUEIRA; CARVALHO et al., 2012). The mandible presents itself as one of the most commonly fractured bones due to its prominence (BAIRRAL; DUARTE et al., 2011), occupying the second place among all facial skeleton fractures (SAKR; FARAG and ZEITOUN, 2006).
The etiological agents of mandibular fractures may vary according to the region studied; the most common causes are: automobile accidents, physical aggression, sports accidents, firearms and pathological fractures (SCARIOT; OLIVEIRA et al., 2009).
According to Côrtes (2010) mandible fractures are among the most frequent lesions found in trauma treatment centers. In recent times, one of the main causes of mandible fracture has been physical aggression by firearm (CÔRTES; MARQUES and GUEDES, 2010), these lesions have been presenting as an important public health problem due to their morbidity and mortality rate (BERMEJO; COLÉTE et al., 2016).
Gunshot wounds to the face can result in devastating consequences for patients, depending on the caliber of the weapon used and the distance the patient is from the scene of the shooting can result in devastating aesthetic and functional consequences (HOLLIER; GRANTCHAROVA and KATTASH, 2001).
The management of patients with gunshot wounds to the face remains quite controversial in relation to treatment (CLARK; BIRELY et al., 1996); the literature on the therapy for gunshot wounds to the face is scarce (MCLEAN; MOORE and YELLIN, 2005), some professionals advise performing surgical intervention in the initial stage (CLARK; BIRELY et al., 1996), however, some studies report a more conservative approach, without performing surgical procedures in the first moments (WEIDER; HUGHES et al., 1999).
Some important innovations have enabled a better treatment of mandibular fractures, such as the use of locking system plates, which can facilitate the management of fractures, whether simple or complicated, however, this does not totally eliminate complications (MORAIS; CARVALHO et al., 2010).
CLINICAL CASE
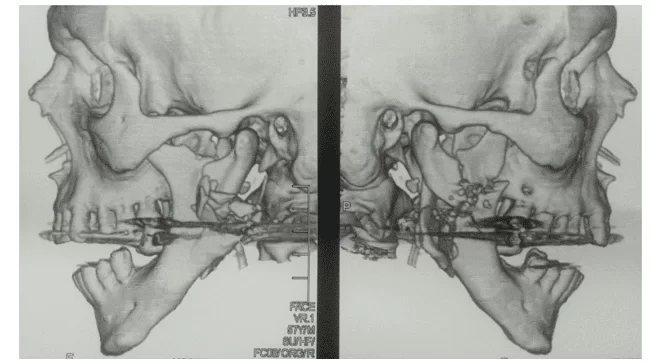
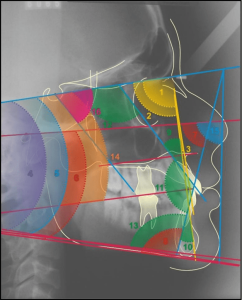
A 67-year-old male leucoderma patient was admitted to the Regional Hospital of Agreste, located in the city of Caruaru, victim of PAF-Familial Amyloidotic Polyneuropathy on the face, in which he was evaluated by the general surgery that opted, as initial conduct, the patient was tracheostomized in order to maintain a pervious airway. The next day, the patient was transferred to the Bucomaxillofacial Traumatology service of the Santa Ephigenia Hospital, in the same city. During the anamnesis, an extra oral orifice of the projectile was incoming in the right region of the face at the level of mandibular angle and exit hole at the level of extraoral left mandibular angle; the patient presented ecchymosis in the jugal region and continuity solution in the angle region and right and left body of the mandible. Imaging was performed (Computed Tomography), confirming the clinical findings of bilateral mandible fracture, with extensive comminution of bodies and mandibular angles, bilaterally caused a displacement between the fragments and with loss of basilar leveling, thus generating a defect in the continuity of the mandible. (Figure 1).
Figure 1 – Computed tomography denoting the extensive comminution of bodies and mandibular angles.
The patient remained hospitalized, using antibiotic medications, steroid al-inflammatory, analgesic and non-steroidal anti-inflammatory drugs parenteral (intravenous), in addition to liquid diet and maintenance of tracheostomy.
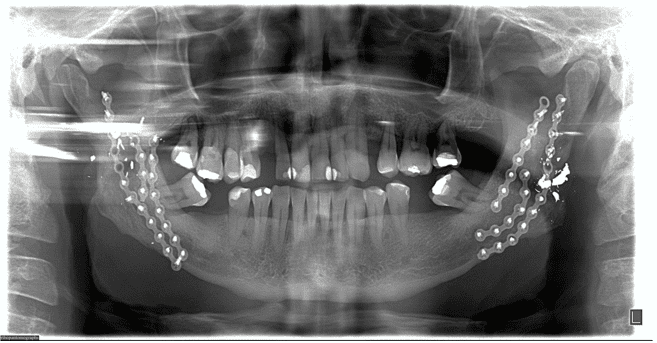
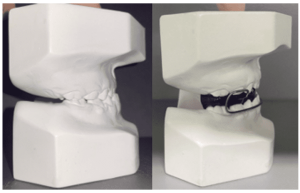
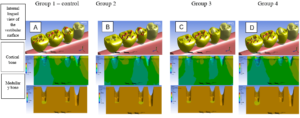
The surgery was performed after 14 days with nasal intubation and mandibular maxillary block, we opted for extraoral access, covering the submandibular region bilaterally with dilution of the planes, exposure of the areas of the fractured mandible; the reduction and surgical fixation of the mandible and fragments were performed with 2.0 mm straight titanium miniplates, the plates were modeled to fix the comminuted bone fragments, providing stability of the mandible and rescuing the mandibular framework. (Figure 2 and 3)
Figure 2 – Right angle submandibular access and 2.0 mm plate fixation
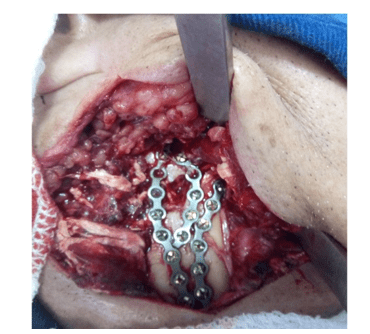 Figure 3 – Left angle submandibular access and 2.0 mm plate fixation
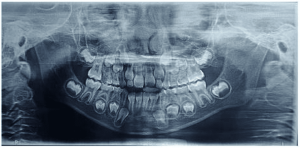
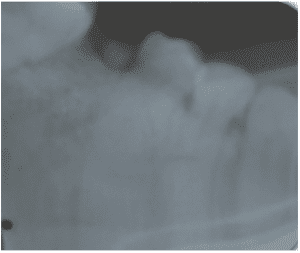
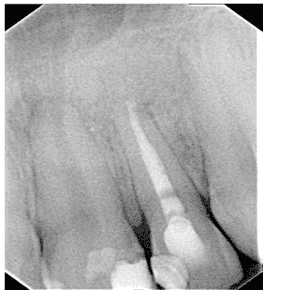
Figure 3 – Left angle submandibular access and 2.0 mm plate fixation After the fourth postoperative day and hospitalization, the patient was discharged from the hospital because he was in a general, asymptomatic condition; there was no deficit of nerve structures, presenting preserved mandibular movements, only manifested a small difficulty to open the mouth, indicating a satisfactory occlusion. When performing the postoperative radiographic examination, the continuity of the bone segments was observed, without other alterations (Figure 3). Physiotherapy was requested to recover, as soon as possible, the range of motion, stimulating and contributing to the return of the affected sensitivity during surgery.
After the fourth postoperative day and hospitalization, the patient was discharged from the hospital because he was in a general, asymptomatic condition; there was no deficit of nerve structures, presenting preserved mandibular movements, only manifested a small difficulty to open the mouth, indicating a satisfactory occlusion. When performing the postoperative radiographic examination, the continuity of the bone segments was observed, without other alterations (Figure 3). Physiotherapy was requested to recover, as soon as possible, the range of motion, stimulating and contributing to the return of the affected sensitivity during surgery.
Figure 3 – Radiographic examinations (panoramic) denoting the reconstruction of the mandible with the internal fixation system.
DISCUSSION
It is of great importance that professionals working in the care of PAF victims take into account the ATLS protocol. Often, apparently innocuous lesions can present unpleasant surprises for the professional, it is the responsibility of the surgeon to know that the presence of a skilled and well-trained team, may indicate or contraindicate definitive surgery at the first moment (RODRIGUES; ALMEIDA et al., 2020) (MORAIS; CARVALHO et al., 2010) (DANTAS; SILVA et al., 2018).
Most of the times the injuries caused by PAF are due to criminal activities (MORAIS; CARVALHO et al., 2010) (RODRIGUES; ALMEIDA et al., 2020), such extensive injuries may include bruising, profuse haemorrhage, contamination and increased intracranial pressure (GIESE; KOOPS et al., 2002) . When these projections reach the bones of the face, fractures of cominuído pattern in the mandible and transfixing wound in the maxilla predominate (MORAIS; CARVALHO et al., 2010).
The late or immediate approach to fractures presents many controversies in the literature, but it is up to the Bucomaxillofacial surgeon, together with an assistant team, to consider the potential of infection that such lesions are associated with, regarding the decision to maintain the projectile, it should be taken into account its location in the affected anatomical spaces (RODRIGUES; ALMEIDA et al., 2020). Each situation should be carefully evaluated and the decision of the ideal time for treatment should be chosen according to each situation, aiming at the complete restoration of the patient’s functions as soon as possible (KROON; VAN BEEK and VAN DAMME, 2007).
Another perspective related to the cases of gunshot wounds in the face, in most situations, is the maintenance or not of the projectile (RODRIGUES; ALMEIDA et al., 2020). It is essential that decision-making, by surgical or conservative approach, in relation to the objects housed can take into account clinical, surgical and anatomical criteria, in order to bring better quality of life and lower morbidity to the patient (SUASSUNA; SILVA JÚNIOR et al., 2017). These criteria should be considered with significant parsimony, because the location of the projectile is close to noble structures, such as veins, arteries and nerves, besides that the location to which the projectile is located can hinder or hinder its removal (RODRIGUES; ALMEIDA et al., 2020).
The surgeon needs to understand that not all gunshot wounds require surgical treatment. Injuries in which the projectile transfixed the structures without causing fracture or vascular injury do not require a surgical intervention, the protocol is cleaning the edges of the wound (DEMETRIADES; CHAHWAN et al., 1998). However, in PAF injuries with fractures in the mandible, the use of reconstruction plates predominates as treatment because it has advantages over other stabilization systems (ROCTON; CHAINE et al., 2007). The use of internal fixation systems eliminates or reduces the need for intermaxillary block, this fixation system presents as advantages the possibility of the patient talking, chewing, improving nutritional status. However, the lack of professional skill in the technique is a frequent event in the application of internal devices for fixation of mandibular comtinutive fractures, this lack of ability cause can cause damage to the roots of the teeth, fracture of the screw during insertion, absence of stable bone structures for fixation of osteosynthesis material and bone sequestration at the perforation site (RODRIGUES; ALMEIDA et al., 2020) (IMAZAWA; KOMURO et al., 2006).
Considering all the factors mentioned, the case described was conducted in the best possible way. The 2.0 mm plate system was used to reduce and adequately fix the multiple bone fragments, allowing the masticatory load to be supported, showing that the conduction of the case presented satisfactory results, reestablishing function and aesthetic contour, with minimal exposure of complications to the patient.
CONCLUSION
Face trauma involving firearms presents a challenge for the Bucomaxillofacial Surgeon, since the destructive level caused by such trauma is significant, always leading to questions regarding the best methodology for treatment, because it involves anatomical structures of great importance. The case mentioned showed that the use of rigid internal fixation through open reduction improved the patient’s well-being in the postoperative period, considering that this surgical technique allows a rapid return to normal physiological function, because it is more predictable optimizes the treatment result and reduces complications, allowing the reintegration of the patient to society in a short period of time , reducing the socioeconomic impact.
BIBLIOGRAPHY
BAIRRAL, J. V. et al. Otite Média e Anquilose na Região Temporomandibular Causada por Fratura de Arma de Fogo. Relato de Caso. Rev. Cir. Traumatol. Buco-Maxilo-Fac., Camaragibe, v. 11, n. 2, p. 27-32, abr./jun. 2011.
BERMEJO, P. R. et al. Tratamento cirúrgico de fratura mandibular decorrente de projétil de arma de fogo: relato de caso. Arch Health Invest, v. 5, n. 6, p. 330-335, 2016.
CLARK, N. et al. High-energy Ballistic and Avulsive Facial Injuries: Classification, Patterns, and an Algorithm for Primary Reconstruction. Plast Reconstr Surg, v. 98, n. 4, p. 583-601, Sep. 1996.
CÔRTES, M. G. W.; MARQUES, A. C.; GUEDES, L. J. Fratura cominutiva grave de mandíbula por arma de fogo: relato de caso. Rev Méd Minas Gerais, v. 20, p. 415-418, 2010.
DANTAS, A. C. G. C. et al. Fratura cominutiva de mandíbula por fogos de artifício. Relato de caso. Rev. Cir. Traumatol. Buco-Maxilo-Fac., Camaragibe, v. 18, n. 3, p. 17-21, jul./set. 2018.
DEMETRIADES, D. et al. Initial Evaluation and Management of Gunshot Wounds to the Face. J Trauma, v. 45, n. 1, p. 38-41, Jul. 1998.
GIESE, A. et al. Head Injury by Gunshots From Blank Cartridges. Surg Neurol, v. 67, n. 4, p. 268-277, Apr. 2002.
HOLLIER, L.; GRANTCHAROVA, E. P.; KATTASH, M. Facial Gunshot Wounds: A 4-year Experience. J Oral Maxillofac Surg, v. 59, n. 3, p. 277-82, Mar. 2001.
IMAZAWA, T. et al. Mandibular Fractures Treated With Maxillomandibular Fixation Screws (MMFS Method). J Craniofac Surg, v. 17, n. 3, p. 544-549, May. 2006.
KROON, F. H. M.; VAN BEEK, G. J.; VAN DAMME, P. A. Cranio-maxillofacial Traumatology. Ned Tijdschr Tandheelkd, v. 114, n. 1, p. 23-33., jan. 2007.
MCLEAN , J. N.; MOORE, C. E.; YELLIN, S. A. Gunshot Wounds to the Face-Acute Management. Facial Plast Surg, v. 21, n. 3, p. 191-198, Aug. 2005.
MORAIS, H. H. A. D. et al. Tratamento imediato de fratura de mandíbula por projétil de arma de fogo. RGO – Rev Gaúcha Odontol., Porto Alegre, v. 58, n. 3, p. 399-403, jul./set. 2010.
ROCTON, S. et al. Mandibular Fractures: Epidemiology, Therapeutic Management, and Complications in a Series of 563 Cases. Rev Stomatol Chir Maxillofac, v. 108, n. 1, p. 3-10, Feb. 2007.
RODRIGUES, C. M. D. C. et al. Tratamento conservador de ferimento por arma de fogo em face, associado remoção cirúrgica tardia de projetil sob anestesia local – relato de caso. Brazilian Journal of health Review, Curitiba, v. 3, n. 2, p. 3044-3053, mar./apr 2020.
SAKR, ; FARAG, I. A.; ZEITOUN, I. M. Review of 509 Mandibular Fractures Treated at the University Hospital, Alexandria, Egypt. Br J Oral Maxillofac Surg, v. 44, n. 2, p. 107-111, Apr. 2006.
SCARIOT, R. et al. Maxillofacial Injuries in a Group of Brazilian Subjects Under 18 Years of Age. J Appl Oral Sci., v. 17, n. 3, p. 195-195, 2009.
SIQUEIRA, P. et al. Fratura mandibular após injúria por projétil de arma de fogo: relato de caso clínico. Revista de Odontologia da UNESP, v. 41, n. 2, p. 133-138, Mar-Apr. 2012.
SUASSUNA, T. M. et al. Retenção de Projéteis de arma de fogo na face – relato de casos. Rev. Cir. Traumatol. Buco-Maxilo-Fac., Camaragibe , v. 17, n. 1, p. 46-50, jan./mar. 2017.
WEIDER, L. et al. Early Versus Delayed Repair of Facial Fractures in the Multiply Injured Patient. Am Surg, v. 65, n. 8, p. 790-793, Aug. 1999.
[1] PhD student in Biomedical Sciences at IUNIR – Italian University Institute of Rosario. Specialist in Bucomaxillofacial Surgery and Traumatology by Ciodonto – Integrated Dentistry Clinic. Graduated in Dentistry from ASCES – Caruaruense Association of Higher Education. Graduated in Biologist from UPE – University of Pernambuco.
[2] Graduated from the Physiotherapy Course of UNISSAU College.
[3] Graduated in Dentistry from Asces Unita. Attending Specialization in Orthodontics – Cruzeiro do Sul College.
Sent: July, 2020.
Approved: November, 2020.