REVIEW ARTICLE
SOUZA, Ana Carolina Oliveira de [1], CASTRO, Joely Zelinda Menezes [2], MEIRA, Gabriela de Figueiredo [3], REGO, Jessica Tuane Maia [4]
SOUZA, Ana Carolina Oliveira de. et al. Influence of hyperthyroidism and hypothyroidism on the oral cavity: literature review. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year 08, Ed. 06, Vol. 03, pp. 82-106. June 2023. ISSN: 2448-0959, Access link: https://www.nucleodoconhecimento.com.br/dentistry/oral-cavity, DOI: 10.32749/nucleodoconhecimento.com.br/dentistry/oral-cavity
ABSTRACT
Thyroid gland dysfunctions, particularly hyperthyroidism and hypothyroidism, can cause systemic alterations such as hypertension, anxiety, and bone changes, as well as oral manifestations including salivary alterations, increased periodontal disease, and dental caries. It is of utmost importance for the dentist to be vigilant about these changes, considering that a decompensated patient cannot be treated, and medications can also interfere with oral microbiota, respecting each patient’s limitations. Thus, the objective of this study is to investigate the influence of hyperthyroidism and hypothyroidism on the oral cavity through a literature review from 2018 to 2023. Articles, monographs, dissertations, books, and websites discussing the correlation between thyroid dysfunctions and dentistry were selected. The 30 references found were thoroughly read, but only 26 were directly related to the proposed theme. Conclusion: The dentist is one of the professionals capable of identifying the initial signs and symptoms of the disease, highlighting the importance of a thorough medical history. Further studies on this topic are necessary to consolidate the results found in the literature.
Keywords: Hyperthyroidism, Hypothyroidism, Dentistry.
INTRODUCTION
The thyroid gland is located in the neck, close to the larynx and trachea, and is represented by an isthmus that interconnects two lobes. To distinguish them, the right lobe appears larger than the left, and some patients may exhibit an upper segment of glandular tissue. Its tissue is found in areas belonging to the thyroglossal duct pathway (LITTLE, 2009; FERNANDES & FREITAS, 2018).
Microscopically, the follicles produce and store hormones: tetraiodothyronine or thyroxine (T4) and triiodothyronine (T3), responsible for regulating organic functions such as temperature adjustment, metabolism of vitamins and lipids, potentiation of other hormones, and bone metabolism (AL-HINDI et al., 2021; CHAVES et al., 2021; TORREJON-MOYA, 2022).
In addition to the aforementioned hormones, the thyroid gland is also responsible for producing calcitonin, which, along with Vitamin D and parathyroid hormone, regulates the metabolism of calcium and phosphorus ions in the blood and participates in bone remodeling (AL-HINDI et al., 2021; LITTLE, 2009, p.24; PEDROSO, 2020).
Although T3 and T4 production occurs in the thyroid gland, the synthesis and release of these hormones are overseen by the hypothalamus-pituitary system through the release of TSH (thyroid stimulating hormone), responsible for thyroid stimulation (AUON, 2021; KUBO, 2018; MESHAIKHY, 2020).
Little (2009, p.239) explains that goiter refers to the structural enlargement of the thyroid gland, which can be functional or non-functional, nodular, or diffuse. When analyzing the functional type, it is subdivided into primary goiter, which includes simple goiters, accounting for 75% of all thyroid enlargements.
Thyroid dysfunction is relatively common, being the second most common among endocrine disorders. It can occur at any age, but women between 30-40 years are the most affected. The most common dysfunctions are hyperthyroidism, characterized by excess hormones, and hypothyroidism, with insufficient hormone production (AL-HINDI et al., 2021; FREITAS, 2022; MESHAIKHY, 2020).
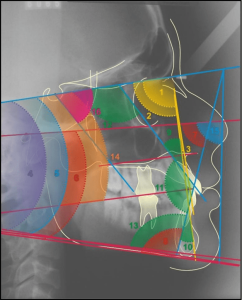
Diagnosis can be made through hormonal quantification or iodine in the blood, through laboratory tests, but clinical signs and symptoms can contribute to the diagnosis. Palpation becomes a great ally in cases of goiter or 1 or more nodules. Imaging tests such as ultrasound, computed tomography, and magnetic resonance imaging are great allies in detecting small lesions, capable of differentiating between liquid and solid ones and defining the gland’s size. Moreover, a detailed medical history with palpation in the neck area is essential, capable of detecting nodules and other relevant abnormalities (AOUN, 2021; LITTLE, 2009).
Thyroid dysfunctions lead to aggressive oral diseases, such as bone loss, root resorption, and exfoliation of teeth associated with periodontal disease, making these patients more vulnerable to developing other oral infections (KSHIRSAGAR et al., 2018).
This work aims to conduct a literature review on two thyroid gland alterations: hypothyroidism and hyperthyroidism and their effects on the oral cavity.
METHODOLOGY
This work consists of a literature review focusing on studies addressing the topics of hypothyroidism and hyperthyroidism, specifically the findings in the oral cavity of patients treated in dental clinics.
The literature search was conducted using databases such as PubMed, Google Scholar, and CAPES journals, utilizing keywords: “hyperthyroidism,” “hyperfunction,” “thyrotoxicosis,” “dentistry and hyperthyroidism,” “hyperthyroidism in dentistry,” “hypothyroidism in dentistry,” in addition to bibliographic searches and relevant websites.
The articles were selected based on inclusion criteria, which required that the articles:
1) Address oral findings in clinical evaluations of patients with hyperthyroidism and hypothyroidism;
2) Be published between the years 2018 to 2023;
3) Be written in Portuguese or English.
For exclusion criteria, articles unrelated to the proposed topic or not meeting the publication year criteria were removed. After applying these criteria, a total of 30 articles were selected for reading, and 25 were included in the final sample.
LITERATURE REVIEW
Naturally, TSH regulates the release of T3 and T4, and these hormones, through the hypothalamus-pituitary-thyroid axis, inhibit the production of more TSH by the body, thus interrupting the cycle of T3 and T4 release and leading to hormonal balance (AOUN 2021; FREITAS, 2022; MESHAIKHY, 2020).
According to Chaves et al. (2021), Fernandes and Freitas (2018), and Martinez (2019), iodine is an extremely important component in the synthesis of T3 and T4 and is primarily obtained from the diet, currently found in table salt, with its quantity varying depending on the locality.
Iodine deficiency is the most common cause of thyroid disorders and is related to thyrotoxicosis. In total, one-third of the world’s population suffers from iodine deficiency; on the other hand, high ingestion of this ion increases the prevalence of Graves’ disease (LITTLE, 2009, p.241; MESHAIKHY et al., 2020, TAYLOR et al., 2018).
Geduk (2021), in a case report, followed numerous patients to estimate this in a university near the Black Sea in Turkey. According to the author, there is a significant iodine deficiency in the population’s food, and many people have endocrine alterations due to this deficiency. Nevertheless, 90% of the respondents did not have dysfunctions, while 8.8% had hypothyroidism, 0.6% had hyperthyroidism, 0.1% had Hashimoto’s thyroiditis, and another 0.1% had a history of thyroid cancer.
HYPERTHYROIDISM
The thyroid gland’s function is to remove iodine ions from the diet and transform them into the hormones T3 and T4. Hyperthyroidism is a disorder of the thyroid gland, characterized by an excess production of hormones, tri-iodothyronine (T3) and thyroxine (T4), and a decrease in the stimulating hormone (TSH) (ARAÚJO, 2019; HUSSEIN et al., 2022; MESHAIKHY, 2020).
Both T3 and T4 are responsible for regulating the body’s metabolism, so when there is an overproduction of these hormones circulating in the bloodstream, a phenomenon known as thyrotoxicosis, there is an acceleration of metabolism, resulting in a range of signs and symptoms (FABRIS et al., 2021).
According to Geduk (2021), thyrotoxicosis is a severe emergency condition requiring immediate treatment. The author mentions that thyrotoxicosis symptoms occur between the sixth and eighth postoperative hour, and clinical signs include: fever above 38.5°C, tachycardia, central nervous system findings (anxiety, agitation, delirium, acute psychosis, and coma), and gastrointestinal manifestations (nausea, vomiting, abdominal pain, diarrhea, jaundice).
Graves’ Disease, an autoimmune disease, is the most commonly found form, characterized by the presence of a multilobular goiter. In this pathology, Kubo (2018) states that autoantibodies target the TSH thyroid receptors, inducing thyroid hormone production.
The hyperfunction of the thyroid gland is clinical evidence of hormone excess due to the presence of thyrotoxins. Its diagnosis is made through laboratory tests and specialist follow-ups, with the initial assessment performed by TSH level tests (UFRGS, 2021).
Patients may exhibit symptoms such as heat, hyperhidrosis, and erythema upon touch in the region. The skin appears warm and smooth. Patients may also experience tremors, anxiety, weight loss, early cardiac manifestations, weakness, palpitations, anxiety/irritability, insomnia, nervousness, menstrual cycle changes. Physical examinations may reveal elevated body temperature, warmer skin, diffuse goiter, thyroid nodules, thenar/hypothenar atrophies, tachycardia, palpitations, atrial fibrillation, tachypnea, tremors, alopecia, hyperhidrosis, and warm skin (LITTLE et al., 2009; UFRGS, 2021).
Thyroid hormones have effects on the myocardium, explaining why some hyperthyroid patients have hypertension, arrhythmias, or even heart failure (ARAÚJO, 2019).
According to Fabris et al. (2021), clinical findings in patients with exacerbated hyperthyroidism may be related to autoimmune pathologies, as it appears diffuse and enlarged, with ocular alterations leading to ocular muscle paralysis and exophthalmos.
Neville et al. (2016) emphasize that ocular involvement can occur in 20% to 40% of cases, and exophthalmos is characteristic of Graves’ Disease.
INFLUENCE OF HYPERTHYROIDISM ON THE ORAL CAVITY
Before starting dental treatment for patients with such disorders, a more detailed medical history and correct treatment planning are essential, confirming the type of thyroid dysfunction. (ARAÚJO, 2019; AOUN, 2021).
Cases of patients with systemic alterations in the daily practice of dentists are common. Therefore, the professional must be prepared to conduct the ideal clinical approach, avoiding dental complications. If necessary, treatment may be postponed due to the patient experiencing symptoms or being decompensated, such as abnormal blood pressure and heart rate (AOUN, 2021).
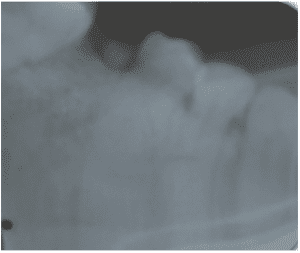
In addition to these symptoms, premature shedding of deciduous teeth and consequently early eruption in children can occur. In adults, the development of osteoporosis in the mandibular or maxillary region is observed (REGEZI, SCIUBBA, JORDAN 2012).
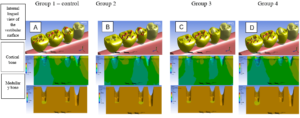
Meshaihky et al. (2020) emphasize in their review on salivary alterations found in patients with thyroid hyperfunction, among them an increased flow rate and its organic and inorganic components. Aoun (2021) analyzed salivary changes in patients with hyperthyroidism and mentioned some oral manifestations found in patients with this type of dysfunction: increased susceptibility to caries, periodontal disease, glandular tissue enlargement (especially in the posterolateral region of the tongue), among others.
Research using a randomized method in a sample of 90 women aged 25 to 45 years showed that patients with hyperthyroidism are at a higher risk of periodontal disease, as there is a change in interleukin-6, a major mediator of the inflammatory response. This alteration, combined with the local microbiota and the patient’s immune response, worsens the inflammatory condition, contributing to the progression of periodontal disease (PD) (KADHOM and RADHI, 2023).
Kshirsagar et al. (2018) conducted a study to verify the prevalence of caries and periodontal health status in different groups. This comparison was made between a study group (individuals with hyperthyroidism) and a control group (individuals not diagnosed with this alteration), resulting in a higher susceptibility to these diseases in the study group.
Al-Yasiry and Al-Jammali (2020) conducted a literature review and stated that patients diagnosed with hyperthyroidism have an increased risk of cavities, periodontal disease, and accelerated tooth eruption.
In the case of pregnant women, it is necessary to advise good prenatal care since a woman diagnosed with thyroid alterations can affect the early stages of fetal development, as the fetus receives thyroid hormones through the placenta (ABREU, 2022).
In the clinical context, it was observed that patients with thyroid dysfunctions can be treated normally, as long as they are controlled, as there are no contraindications in using vasoconstrictor-containing anesthetics. A suitable option is Articaine with 1:200,000 Epinephrine. However, in the case of uncontrolled hyperthyroidism, the patient should only be treated in emergency situations, avoiding certain anesthetic solutions, with Prilocaine 3% with Felypressin being the recommended option (POLESE, 2022).
HYPOTHYROIDISM
Hypothyroidism is characterized by a reduction in thyroid hormone levels, along with distinct clinical signs and symptoms, and is related to various factors, with the most significant being low iodine levels; other tissue and enzymatic dysfunctions also correlate, as well as the presence of autoimmune diseases, with Hashimoto’s Thyroiditis being the most well-known (AL-HINDI et al., 2021; CHAVES et al., 2021; FREITAS, 2022;).
Geduk (2021), Kubo (2018), Taylor et al. (2018) mention one of the classifications of hypothyroidism: based on the level of dysfunction, it can be primary or secondary. It is primary when there is failure of the thyroid gland; it is secondary when other diseases or conditions (such as surgeries) have led to a decrease in circulating hormones. Hypothyroidism can also be congenital due to thyroid malformation or hormonal biosynthesis alteration.
According to Chaves et al. (2021), the classification can vary between central – when there is a reduction in thyroid hormones and TSH, and peripheral – occurs when there is a failure in the mechanism of T3 and T4 hormone production, but in this case, TSH is increased.
According to Martinez (2019), acquired hypothyroidism can result from hormonal stimulation deficiency, severe iron deficiency, use of drugs – such as lithium, radioactive iodine, which destroys the follicles of the gland, iatrogeny – such as surgery, and even chronic thyroiditis, like Hashimoto’s Thyroiditis (TH).
Unlike hyperthyroidism, where there was an increase in metabolic level, hypothyroidism is characterized by weight gain with reduced metabolism. Other symptoms include hypotension, slow heart rate, susceptibility to cardiovascular diseases, lethargy, bradypnea, cold feet and hands, weakness, slow muscle reflex, swelling of the eyelid and face region, weak nails, hair loss, irregular menstrual cycle, voice change caused by gland enlargement, and difficulty swallowing, as well as psychical alterations like depression, anxiety, psychosis, and memory loss (AUON, 2021; FREITAS, 2022; KUBO, 2018).
Al-Hindi et al. (2021) also highlight that hypothyroidism can reduce the recruitment, maturation, and activity of bone cells, decreasing bone formation and resorption. Besides the disease itself, the medications used also influence bone metabolism.
INFLUENCE OF HYPOTHYROIDISM ON THE ORAL CAVITY
Before starting dental treatment, the dentist must have access to the medical conditions of these patients, with their cardiovascular history and lethargy being fundamental. However, a compensated patient will not necessarily require specific precautions (AOUN, 2021, FARIAS et al., 2019).
Achanta and Khasbage (2022) mention the most common oral alterations found in patients with hypothyroidism: macroglossia, dysgeusia, weakened periodontal health, delayed tooth eruption, burning mouth syndrome, and dry mouth.
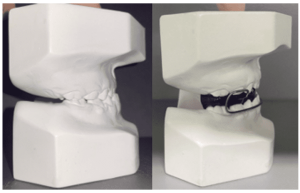
Martinez (2019) also found evidence of manifestations in the development of facial bones, as well as in tooth eruption, highlighting the impaction of second molars, both upper and lower. According to the author, the cause seems to be related to insufficient space due to a failure in normal bone resorption. Other long-term manifestations are highlighted, such as malocclusion and open bite, as condylar bone growth is incomplete in these patients, making them mouth breathers.
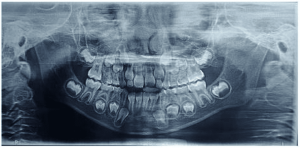
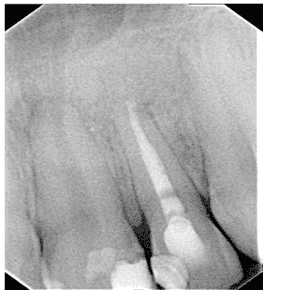
Freitas (2022) reported a clinical case of a child with hypothyroidism, where delayed tooth eruption occurred due to the retention of deciduous teeth in the mouth and the delayed root formation of permanent teeth. It was observed that despite the patient being 9 years old, his bone age corresponded to that of a 5-year-old child.
Regarding other alterations found in the oral cavity in patients with hypothyroidism, Kubo (2018) reports the phenomenon of hyposalivation, where saliva synthesis, composition, and secretion are altered. The author mentions that saliva plays an important role as an antimicrobial agent, stabilizing the pH of the oral cavity and preventing mineral loss from tooth enamel, as well as neutralizing acids and bases. It also serves as a natural lubricant, aiding in the clearance of unwanted substances and food digestion.
In relation to salivary flow, Meshaikhy et al. (2020) conducted an epidemiological survey in Baghdad, Iraq, relating to tooth decay and thyroid dysfunctions (i.e., both hyperthyroidism and hypothyroidism). They found a connection between antithyroid medication used by patients with hypothyroidism, reducing salivary flow, acidifying the oral environment, and altering the organic and inorganic constituents of salivary composition, concluding that this salivary alteration can interfere with the pathogenesis of tooth decay.
Martinez (2019) found evidence of reduced salivary flow in hypothyroidism and reported that it can influence prosthesis retentions, leading to injuries such as oral mucosa ulcers in patients.
In the case of implants, Al-Hindi et al. (2021) sought, through a literature review, to point out clinical cases related to osseointegration and hypothyroidism in association, concluding that this disease does not influence implant success.
Aldulaijan et al. (2019) and Shcherba et al. (2020) found evidence regarding the relationship between Periodontal Disease (PD) and hypothyroidism, the former through a literature review and the latter through experiments with rats.
It is reported by Albulaijan et al. (2019) that local inflammation mediators as a consequence of PD may represent a risk factor for other chronic diseases, thus affecting thyroid hormone production. Furthermore, evidence was found that there is a decrease in resorption during bone remodeling.
Similarly, Pedroso (2020) analyzed the influence of TH on PD. In his literature review, important findings were the loss of alveolar bone and low levels of vitamin D in patients with thyroid alterations; this vitamin actively participates in the immune response, aiding in the release of T and B cells and their cytokines, and with low vitamin D levels and TH, there is a high chance of DP development in these patients.
In the clinical scope, regarding anesthetic salts, Polese (2022) concluded in her article that in controlled hypothyroidism, there are no restrictions on dental care, opting for Articaine with 1:200,000 Epinephrine as the anesthetic choice.
However, uncontrolled patients present anesthetic risks, and elective treatments should be postponed. The dentist should be aware that this condition is primarily treated with levothyroxine monotherapy, and there can be increased responses to drugs affecting the central nervous system function (AOUN, 2021).
RESULTS
The method of presenting the choices of the articles selected for the review was organized in a demonstrative table, containing the following information: article title, author, year, objective, methodology, conclusion, as shown in Table 1.
Table 1: Research Results
| ARTICLE TITLE | AUTHOR(S) | YEAR | OBJECTIVE | METHODOLOGY | CONCLUSIONS |
| Thyroid Gland Dysfunction and Orthodontic Treatment: An Integrative Literature Review | Hatsuo Kubo et al.,
|
2018 | Research in the literature studies based on clinical and scientific evidence, focusing on the importance of identifying oral alterations caused by thyroid gland dysfunction in orthodontic treatment. | Integrative review in the search for scientific findings on thyroid gland alterations correlated to orthodontic treatment. | The variations in alterations are uncommon, ruling out profound scientific evidence.
|
| Dentist’s Knowledge of Local Anesthetic Use in Patients: Diabetics, Hypertensive Individuals, Cardiac Patients, Pregnant Women, and Those with Hyperthyroidism | Vinicius Fabris et al.,
|
2018 | Assessment of Professionals’ Understanding Levels in the Use of Anesthetics in Patients with Clinical Disorders | Cross-sectional Quantity Planning Work with Data Selection through Author-conducted Questionnaires using an Instrument | The professionals demonstrated a lack of understanding in clinical conduct when choosing the anesthetic |
| Hyperthyroidism | Ana Claudia M.M., Dimitris et al.,
|
2021 | To report clinical manifestations, diagnosis, signs and symptoms, treatment, and possible clinical approach | Bibliographic Study by the Federal University of Rio Grande do Sul – School of Medicine, carried out with the purpose of conducting a bibliographic study on hyperthyroidism | The authors emphasized the importance of initial and final clinical knowledge to guide the best treatment throughout all stages of hyperthyroidism |
| Influence of Hashimoto’s Thyroiditis on Periodontal Disease. | Inês Sofia Prata Pedroso
|
2020 | Understanding how this condition influences the development of periodontal disease | Literature review article covering Hashimoto’s thyroiditis and periodontal disease | The author concluded that there is a possibility of Hashimoto’s disease influencing periodontal disease, but there are few studies that confirm this |
|
Drug-drug interaction in dental clinic:risks in patients with hypothyroidism
|
Farias et al., | 2019 | A literature review addressing potential drug-drug interactions (DDIs) in patients with hypothyroidism and therapeutic approach during dental treatment | Research on pharmaceutical articles and bibliographies | The authors concluded that hypothyroidism affects key parts of the body’s homeostatic system. This underscores the importance for the professional to achieve a more accurate diagnosis, always mindful of potential drug-drug interactions (DDIs) |
| Thyroid Dysfunction: Risk and Management in Dentistry | Georges Aoun | 2021 | To emphasize to the professional the importance of understanding the signs and symptoms for the development of the dental treatment plan. | Research in journals, published articles, and literature focused on oral findings and the care of patients with thyroid dysfunction | The author concluded that professionals should be aware of oral manifestations to handle the patient in any complications regarding their level of control |
| Oral Manifestation for Patients with Thyroid Dysfunction and it’s Management in Dental Clinic -A Review
|
Anas Al-Yasiry M.Sc1 Zainab Mahmood Al-Jammali M.Sc2 et al., | 2020 | Reviewing the most suitable management for thyroid dysfunction, including clinical findings, prevalence, associated comorbidities, and drug interactions | Research on published works, with inclusion and exclusion criteria for in-depth reading | In conclusion, this study demonstrated that dentists need more knowledge about the subject, as well as a more specific study of associated diseases to guide the optimal management of patients for treatment |
| Estimation of Salivary IL-6 Level in relation of Periodontal Status in Patients with
Hyperthyroidism
|
Eman Habib kadhom,
Nada Jafer MH. Radhi
|
2022 | Investigate the association between periodontal health status and IL6 in patients with hyperthyroidism.
|
Simple randomization method | Individuals with hyperthyroidism are at risk for periodontal disease; these patients have high levels of periodontal disease and IL6, and there was a weak non-significant positive correlation between the two |
| Relation between Hypothyroidism and Cancer: Literature Review | Matheus Soares Chaves et al., | 2021 | Search for the Possible Relationship between Hypothyroidism and Cancer | Comprehensive Review Method of Articles and Bibliographies Addressing the Topic | The authors concluded that hypothyroidism may pose a risk for endometrial cancer and others. Further in-depth studies are needed |
| Use of vasoconstrictors in patients with hyperthyroidism | Araujo et al., | 2018 | Reviewing the correct approach regarding the use of vasoconstrictors in patients with hyperthyroidism | Research on databases and use of books | The authors concluded that the use of anesthetics with vasoconstrictors is contraindicated for patients with uncompensated hyperthyroidism |
| Prevalence of hypothyroidism in type 2 diabetes mellitus patients | Gabriel Queiroz Fernandes et al., | 2018 | Relationship between type 1 and type 2 diabetes mellitus and hypothyroidism | Research on patients treated between January and December who had type 1 and type 2 diabetes | The authors concluded the high prevalence of hypothyroidism in patients with type 2 diabetes, which calls for further in-depth study due to the scarcity of literature on the subject |
| Evaluation Thyroid disease stories of indiduals attended to the faculty of dentistry | Ogr Gor Gediz Geduk | 2021 | To study the medical and dental history of patients with systemic alterations and thyroid dysfunction | Clinical evaluation and anamnesis of patients treated at Zonguldak Bulent Ecevit Dental Faculty | The author concluded that conducting a detailed anamnesis is of utmost importance to guide the best treatment for the patient, |
| Patients with thyroid disorder, acontraindication for dental implants? A systematic review | Aina Torrejon-moya et al., | 2022 | Systematic literature review to provide evidence on the relationship between dental implants and the disorder | Research on the database with inclusion and exclusion criteria for full-text reading | The authors concluded that thyroid disorder does not interfere with dental implant treatment |
| Hypothyroidism: Oral manifestations and therapeutic approach in dentistry | Tereza Soriano Martinez | 2019 | Review on the topic aiming to describe the alterations found in the studies | Research of articles related to the discussed topic | In conclusion, the author emphasizes the importance of the professional having knowledge to better guide the patient’s treatment |
| Pediatric Hypothyroidism and Its Relationship with Delayed Tooth Eruption: A Case Report | Rheryda de Sousa Rocha Pereira Freitas | 2022 | Reporting a Clinical Case of a Child with Hypothyroidism and Delayed Dental Eruption Chronology | Clinical intra and extraoral assessment of the patient, as well as physical examination, radiography, and specific tests for treatment | After evaluating the exams, the professional may refer the patient for treatment in collaboration with an endocrinologist, resulting in a rebalancing of the dental eruption chronology |
| A comparative study of connective tissue metabolismo índice in experimental comobidity-free periodontitis and periodontitis combined with thyroid dysfunction | Vitaliy shcherba et al., | 2020 | Confirmatory study of metabolism indices in patients with thyroid disorder and periodontitis | Selection of patients presenting hyperthyroidism and hypothyroidism, clinical evaluation, and periodontal assessment | The authors concluded that periodontitis progresses more significantly when the patient is decompensated, both in hyperthyroidism and hypothyroidism |
| Dermination of the level of il-6 and vaspin in hyperthyroind patients treated with carbimazole | Hussein et al., | 2021 | To evaluate the levels of interleukin-6 and vaspin in patients with hyperthyroidism, | Evaluation of patients aged between 20 to 70 years with hyperthyroidism | Patients with hyperthyroidism have elevated levels of IL-6, but a decrease in vaspin in the same group |
| Global epidemiology of hyperthyroidism and hypothyroidism | Peter N. Taylor et al., | 2018 | Highlighting global differences and environmental factors leading to the occurrence of hypothyroidism and hyperthyroidism | Tabulating risk factors for development, incidence, prevalence in parents with or without iodine, and longitudinal supplementation studies | It was summarized that the current epidemiology of hypothyroidism and hyperthyroidism involves various factors but requires initiatives for further refined research |
| Effects of maternal hyperthyroidism on dental and periodontal histomorphometry of offspring in pre- and postnatal periods in a murine model | Douglas Marinho Abreu | 2022 | Effects of thyroid dysfunction on the periodontium in early stages of life | Study conducted on pregnant rats, with 5 of them induced into hyperthyroidism throughout gestation, and another 5 remaining in a euthyroid state | The author concluded that the morphology manifested only in the postnatal period, during weaning when there was a decrease in the thickness of the odontoblast layers and predentin, and an increase in periodontal ligament thickness |
| Assessment of Dental Caries Experience Among Patients with Thyroid Disorders AttendingDifferent Hospitals in Baghdad City/Iraq
|
Rawaa Basel AL Meshaikhy, Nadia Aftan Al Rawi
|
2020 | To investigate the occurrence of dental caries and assess the impact of the disease and treatment on the dental caries experience at different time intervals
|
Study conducted on 444 patients diagnosed with thyroid disorder, through oral examination, and data presentation was performed using the Statistical Package for Social Science
|
The author concluded that there is a higher dental caries experience in patients with thyroid disorder and that both the duration of the disease and medication can be a factor in exacerbating caries |
| Evaluation of the Thyroid Hormone Action on the Expression of Coding RNAs in Osteoblastic Cells Derived from Human Adipose Tissue
|
Bruna Moretto Rodrigues | 2018 | To study the action of thyroid hormones on RNAs in osteoblastic cells derived from adipose tissue
|
Study using CTM Culture, Osteogenic Induction, T3 Treatment, RNA Sequencing, and Bioinformatic Analysis | |
| Effect of hypothyrodism’s medication (T4) on implant
osstointegration: A case series and literature search
|
Mariam Al-Hindi a et al. | 2021 |
Investigate the effect of thyroxine medication T4 on the osseointegration of dental implants and report five clinical cases
|
“Literature review study using a database from the periods of 1999 to 2019. Also, a patient record review of individuals who received dental implants, were diagnosed with hypothyroidism, and underwent T4 replacement treatment
|
The author concluded that patients with hypothyroidism met the criteria for successful implants |
|
Assessment of Oral Health Status and Treatment Needs among Individuals with Thyroid Dysfunction in Nashik City (Maharashtra): A Cross-Sectional Study
|
Minal Madhukar
Kshirsagar et al. |
2018 |
To assess the prevalence of dental caries and periodontal health status among individuals with thyroid dysfunction in Nashik. Compare the prevalence of thyroid dysfunction between men and women
|
Cross-sectional study on 100 individuals with thyroid disorder at the Endocrinology Center in the city of Nashik | The author concluded that there is an impact of this alteration on oral health, necessitating early diagnosis of thyroid disorder before its progression. Additionally, an appropriate treatment plan is essential to prevent complications |
| Relationship between hypothyroidism and periodontitis: A scoping review
|
Hajer A. Aldulaijan et al. | 2019 |
Assessing existing literature to determine if there is a relationship between hypothyroidism and periodontitis
|
Systematic reviews and meta-analyses using a database |
The author concluded that there are few studies describing the relationship between hypothyroidism and periodontal disease, but based on their studies, it is possible to correlate these two factors |
| Oral Manifestations of Thyroid Disorders | Aparna Achanta, Suwarna Dangore Khasbage | 2022 |
Describe the clinical characteristics of thyroid disorders with detailed emphasis on oral manifestations and dental considerations |
Literature review describing oral findings of thyroid alterations |
The author concludes that any disease can be diagnosed through the oral cavity; if there is any systemic pathology, it is necessary for the treatment to be temporarily halted |
| The influence of thyroid disorders on dental anesthesia | Felipe Polese | 2022 | Evaluate the relationship of thyroid disorders with dental anesthesia | Literature review article focusing on the concept and dental management related to anesthetic choice | The author concluded that depending on whether the patient is treated, undergoing treatment, or untreated, the administration of the anesthetic will vary |
Source: Authors, 2023
DISCUSSION
The selected and reviewed articles presented significant issues that should be emphasized and implemented in the daily clinical practice of dentists. Hyperthyroidism and hypothyroidism are systemic alterations that should be thoroughly studied by professionals for better diagnostic direction and treatment.
Laboratory tests are of paramount importance to ensure the choice and appropriate quantity of anesthetic before procedures. It is the responsibility of the professional to identify and evaluate the tests accurately for this choice (KUBO et al., 2018).
A detailed anamnesis is vital, and establishing a treatment protocol before dental treatments is crucial, considering the prevalence of thyroid disorder in young adults, especially in women (GEDUK, 2021).
Freitas (2022), in a clinical case report of a patient born with hypothyroidism, observed significant delay in the eruption of permanent teeth, emphasizing the importance of referral to an endocrinologist for hormonal restoration for the patient’s oral health. Subsequently, the eruptive process continued.
Aoun (2021) concluded his study by emphasizing the importance of dentists being familiar with oral and general manifestations to recognize possible alterations or complications. Special emphasis was given regarding postponing potential dental treatments until a medical evaluation is conducted, as well as the preparedness of the dentist in cases of emergency measures.
In agreement, Kshirsagar et al. (2018) concluded in their study that concerning thyroid dysfunction, along with the severity of analyzed caries and periodontal destruction, more women were affected than men. They cited the importance of early detection to prevent disease progression and tailor the treatment plan for each condition.
Al-Jasiry and Al-Jammali (2020) concluded that the information gathered in the anamnesis is important and prevents complications arising from dental clinics. Many patients have cardiovascular problems, especially in cases of hyperthyroidism, and require antibiotic prophylaxis before treatment. In cases of hypothyroidism, patients may be sensitive to barbiturates and central nervous system depressants, necessitating a possible dosage reduction.
Regarding anesthetics, in cases of well-compensated hyperthyroidism patients, Araújo (2019) mentioned that they should be used wisely and rationally. The author noted that the chances of generating stress due to a lack of vasoconstrictor may lead to an increased release of catecholamines. The use of two cartridges is documented in the literature, and anesthetic with felypressin is a viable option, except for pregnant patients.
Contrarily, Geduk (2021) emphasized that the use of anesthetics without vasoconstrictors is better, as a crisis in hyperthyroidism cases can occur with the combination of stress and local anesthetic.
Another significant alteration found in the literature was the reduction of salivary flow. Martinez (2019) found evidence on this subject in hypothyroidism and reported that it can influence prosthesis retentions, leading to injuries such as oral mucosal ulcers in patients.
Meshaikhy et al. (2020) concluded in their study that there is a strong association between dental caries and thyroid dysfunctions, and the duration of thyroid disease, along with the choice of medication for treatment, can potentiate the prevalence of dental caries and periodontal disease.
Regarding implants, hypothyroidism does not seem to be related to the failure and/or survival of dental implants, but it appears to be related to tissue healing time and the level of bone regeneration and resorption (MARTINEZ, 2019).
In agreement, Al-Hindi et al. (2021) concluded that dental implants in patients with hypothyroidism meet the criteria for successful implantation. The author recommends additional good documentation to confirm possible clinical findings.
Torrejon-Moya (2022) also concluded that patients with thyroid disorders can be rehabilitated with dental implants, with implant survival similar to that of patients without thyroid dysfunctions, with a success rate above 93%, with no difference between hypothyroidism and hyperthyroidism.
However, Geduk (2021) makes a caveat: uncontrolled patients, both in hyperthyroidism and hypothyroidism, should not undergo invasive treatments or even anesthesia. To perform surgical procedures, disease control is necessary, as patients with hormonal peaks may also experience an adrenaline rush.
Regarding periodontal disease (PD), Aldulaijan et al. (2019) found a positive association between hypothyroidism and periodontitis, and it seems to be more evident in patients with severe periodontitis. However, it was suggested that further clinical studies are needed to confirm this association and to investigate the severity one disease can cause in the other.
Pedroso (2020) concluded with the influence of the consequences of hypothyroidism – in Hashimoto’s thyroiditis – on the periodontium and bone tissues, which stimulates the development of PD, with reduced vitamin D being a negative factor for PD.
Kadhom and Rahdi (2023), in their study on periodontal health and the relationship of interleukin-6 in hyperthyroidism, found a significant difference in this inflammatory mediator in patients with dysfunction. Thus, these patients are at higher risk for PD.
The discussed topic is important because the new generation must be aware that every pathology has its uniqueness. In graduation, the management of patients with special needs is limited to only the most common diseases such as diabetes, hypertension, etc. In the face of this, there is a need for greater interest from both students and professionals to expand their knowledge in caring for individuals with special needs.
Thus, caring for patients with systemic dysfunctions is not only about anesthetic choice but being aware that they also have their physical limitations. Conditioning goes beyond the dental chair, always aiming for comfort and avoiding causing stress, which can be very dangerous, especially in cases of hormonal imbalance.
CONCLUSION
The importance of knowledge about these conditions for the dentist is crucial, as the professional can identify the early signs and symptoms, as well as the need to change the way patients are managed, starting from a detailed anamnesis to the correct choice of anesthetic, as well as the alterations found in the mouth (such as periodontal disease, dental caries, bone alterations, and salivary changes).
REFERENCES
ABREU, Douglas Marinho. Efeitos do Hipertireoidismo Materno na Histomorfometria Dentária e Periodontal da Prole no Período Pré e Pós Natal em Modelo Murino.2022. Dissertação (Mestrado em Ciência Animal) – Universidade Federal de Minas Gerais, Minas Gerais, 2022. Disponível em http://hdl.handle.net/1843/48567. Acesso em 22 mai.2023
ACHANTA, Aparna; KHASHBAGE, Suwarna Dangore. Oral Manifestations of Thyroid Disorders. Journal of Research in Medical Dental Science, v.10, p.012-016, set-2022.
ALDULAIJAN, Hajer A; Cohen, Robert E; Stellrecht, Elizabeth M; Levine, Michael J ; Yerke, Lisa M. Relationship between hypothyroidism and periodontitis: A scoping review. Clinical and Experimental Dental Research, v.6, n.1, p.147-157, 2019.
AL-HINDI, Mariam; AL-FOTAWI, Randa; AL-TAMIMI, Abdulaziz; KHALIL, Osama; AL-OSAIMI, Naif; AL-GHAMDI, Khalid; HEJI, Khloud . Effect of hypothyrodism’s medication (T4) on implant osstointegration: A case series and literature search. International Journal of Surgery Case Reports, v.79, p.255-262, 2021.
AL-YASIRY, Anas M.SC1; AL-JAMMALI, Zainab B Mahmood M.Sc2. Oral Manifestation for Patients with Thyroid Dysfunction and it’s Management in Dental Clinic -A Review. International Journal of Drug Research and Dental Science, v.2, n.1, p.23-26, 2020.
AOUN, Georges. Thyroid Disfunction: Risk and Management in Dentistry. Current Research in Dentistry, v.12, n.1, p.1-6, 2021.
ARAUJO, Emanuele Castro; SILVA, Thaís Evellyn da; ROCHA, Marcela Paschoal; OLIVEIRA, Leandro Moraes Coelho de. Uso de vasoconstritores em pacientes portadores de Hipertireoidismo. Revista Pró-UniverSUS, Vassouras-RJ, v.10, n.1, 2019.
CHAVES, Mateus Soares; MARQUES, Gabriel Henrique Nogueira ; THIAGO, João Victor Marques; TELES, Lucca Cordeiro; SAFATLE, Giselle Cunha Barbosa; ROCHA, Karine Siqueira Cabral; ORSOLIN, Priscila Capelari; AMANCIO, Natália de Fátima Gonçalves. Relação entre hipotireoidismo e câncer: revisão de literatura. Brazilian Journal of Health Review, Curitiba, v.4, n.1, p. 156-168, 2021.
FABRIS, Vinicius; SCORTEGAGNA, Ariane Ruaro; OLIVEIRA, Gabriel Rodrigues; SCORTEGAGNA, Gabriela Trentin; MALMANN, Fernando. Conhecimento dos cirurgiões dentistas sobre o uso de anestésicos locais em pacientes: diabéticos, hipertensos, cardiopatas, gestantes e com hipertireoidismo. Journal of Oral Investigations, Passo Fundo, v.7, n.1, p. 33-51, 2018.
FARIAS, Karolina Ferreira; LEAL, Luiza Rabello; RIBEIRO, Raíssa Barbosa; VILLELA, Christina Gaspar. Drug-drug interaction in dental clinic: risks in patients with hypotireoidism. Revista Brasileira de Odontologia, Supl.1, 2019.
FERNANDES, Gabriel Queiros; FREITAS, Giordanne Guimaraes. Prevalência de hipotireoidismo em pacientes com diabetes mellitus tipo 2. Revista de Medicina, São Paulo, v.97, n.3, 2018.
FREITAS, Rheryda de Sousa Rocha Pereira. HIPOTIREOIDISMO INFANTIL E SUA RELAÇÃO COM O ATRASO DA ERUPÇÃO DENTÁRIA: RELATO DE CASO.2022. Trabalho de conclusão de curso (Graduação em odontologia) – Centro Universitário Christus, Fortaleza, 2022.
GEDUK Gediz; HAYLAZ, Emre. Evaluation of thyroid disease stories of individuals attended to the faculty of dentistry.Current Research in Dental Sciences, v.31, n.2, p.147-153,2021.
HUSSEIN, Dina Khudhair; AL-JOWARI, Suha Abdul-Khaliq; RAHMAH, Abbas Mahdi. Determination of the Levelof IL-6 and Vaspin in Hyperthyroid patients treated wth carbimazole. Iraqi Journal of Science, v. 63, N. 5, p. 1909-1917, 2022.
KADHOM, Eman Habib; RADHI, Nada Jafer MH. Estimation of Salivary IL-6 Level in relation of Periodontal Status in Patients with Hyperthyroidism. Al-Kindy College Medical Journal, v.19, n.1, p.115-120, 2023.
KSHIRSAGAR Madhukar Minal; DODAMANI, Arun Suresh; KARIBASAPPA, Gundbakhta Nagappa; VISHWAKARMA, Prashanth Yachrappa; VATHAR, Jagdishchandra Bheemasain; SONAWANE, Kapil Ramesh. Assessment of oral health status and treatment needs among individuals with thyroid dysfunction in Nashik city (Maharashtra): A cross-sectional study. Contemporary Clinical Dentistry, v.9, n.4, p.619-624, 2018.
KUBO, Hatsuo; LEAL, Taís Pereira; BRUDER, Carolina; BERTOLO,Carlos Antonio; ORTOLANI, Cristina Lúcia Feijó; TAKEI,Vera Lúcia Fukuda. Disfunção da glândula tireoide o tratamento ortodôntico: Revisão integrativa da literatura. Revista Uningá, v. 55, n. 3, p. 100-110, 2018.
LITTLE, James W; FALACE, Donald A; MILLER, Craig S; RHODUS, Nelson L. Manejo odontológico do paciente clinicamente comprometido. 7ª ed. Rio de Janeiro: Elsevier, 2009, p.231
MARTINEZ, Teresa Soriano. Hipotirodismo: Manifestações orais e abordagem terapêutica em medicina dentária. 2019. Dissertação (Mestrado Integrado em Medicina Dentária) – Instituto Universitário Egas Moniz, 2019.
MESHAIKHY, Rawaa Basel AL; RAWI, Nadia Aftan AL. Assessment of Dental Caries Experience Among Patients with Thyroid Disorders Attending Different Hospitals in Baghdad City/Iraq. Journal of Research in Medical and Dental Science, v.8, n.5, p.37-43, 2020.
NEVILLE, Brad W; DAMM, Douglas D; ALLEN, Carl M; CHI, Angela C. Patologia oral e maxilofacial.4ª Edição.Rio de Janeiro: Elsevier, 2016, p.1587.
PEDROSO, Inês Sofia Prata. Influência da tiroidite de Hashimoto na doença periodontal. 2020. Dissertação (Mestrado Integrativo em Medicina Dentária) – Instituto Universitário Egas Moniz, 2020.
POLESE, Filipe. Influência dos distúrbios da tireoide na anestesia odontológica. DFL ACADEMY. Disponível em: https://www.anestesie.com.br/wp-content/uploads/2022/11/artigo_anestesie_dr-filipe_tireoide-1.pdf . Acesso em 24 mai.2022
REGEZI, Joseph A; SCIUBBA, James J; JORDAN, Richard C.K. Patologia oral: correlações clinicopatológicas.6ª ed. Rio de Janeiro: Elsevier,2012, p.351
RODRIGUES, Bruna Moretto. Avaliação da ação do hormônio tireoidiano na expressão dos RNAs codificantes em células osteoblásticas derivadas de tecido adiposo humano.2018. Dissertação (Mestrado em fisiopatologia em Clínica Médica) Faculdade de Medicina – Universidade Estadual Paulista Júlio de Mesquita Filho, Botucatu, 2018.
SHCHERBA, Vitaly; KYRYLIV, Mariia; BEKUS, Iryna; KRYNYTSKA, Inna; MARUSHCHAK, Mariya; KORDA, Mykhaylo. A Comparative Study of Connective Tissue Metabolism Indices in Experimental Comorbidity-Free Periodontitis and Periodontitis Combined with Thyroid Dysfunction. Journal of medicine and life, v.13, n.2, p.219-224, 2020.
TAYLOR, Peter N; ALBRECHT, Diana; SCHOLZ, Anna; GUTIERREZ-BUEY, Gala; LAZARUS, John H; DAYAN, Colin M; OKOSIEME, Onyebuchi E. Global Epidemiology of hyperthyroidism and hypothyroidism. Nature Reviews Endocrinology, v.14, n.5, p.301-316, 2018
TORREJON-MOYA, Aina; IZQUIERDO-GOMEZ, Keila; PEREZ-SAYANS, Mario; JANA-SALAS, Enric; ROIG, Antonio Marí; LOPEZ-LOPEZ, José. Patients with Thyroid Disorder, a Contraindication for Dental Implants? A Systematic Review. Journal of Clinical Medicine, v.11, n.9, 2022.
UNIVERSIDADE FEDERAL DO RIO GRANDE DO SUL (UFRGS). Telecondutas: Hipertireoidismo.Versão digital 2021. Disponível em: https://www.ufrgs.br/telessauders/documentos/telecondutas/tc_hipertireoidismo.pdf. Acesso em: 16 maio.2023
[1] Dentistry Undergraduate. ORCID: 0009-0002-1436-0851. Currículo Lattes: 3503259999421188.
[2] Dentistry Undergraduate. ORCID: 0009-0004-7824-8337.
[3] Ph.D., Master’s, Postgraduate, and Dentistry Undergraduate. ORCID: 0000-0002-8285-8769. Currículo Lattes: 3710771916871688.
[4] Postgraduate and Dentistry Undergraduate. Supervisor. ORCID: 0000-0001-9396-4201. Currículo Lattes: 9442936841513278.
Submitted: June 2, 2023.
Approved: June 9, 2023.