ARTIGO DE REVISÃO
ANNUNCIAÇÃO, Andressa Vitória Tavares Pereira da [1]
ANNUNCIAÇÃO, Andressa Vitória Tavares Pereira da. Keratistic Odontogenic Tumor: From diagnosis to treatment. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year 05, Ed. 09, Vol. 02, pp. 85-90. September 2020. ISSN: 2448-0959, Access Link: https://www.nucleodoconhecimento.com.br/dentistry/tumor-odontogenic, DOI: 10.32749/nucleodoconhecimento.com.br/dentistry/tumor-odontogenic
SUMMARY
Odontogenic tumors are neoplasms that develop in the region of the gnathic bones, originating from odontogenic tissues by proliferation of epithelial tissue, mesenchymal or both. Among them, we can mention the odontogenic keratocyst that has its own characteristics and totally differentiated from any other oral pathology presenting a challenge for diagnosis to the professional. The objective of this work is to conduct a literature review on dental keratocyst and address clinical and radiographic characteristics associated with this pathology, as well as its therapeutic approach.
Keywords: tumor, odontogenic, pathology, neoplasms.
1. INTRODUCTION
The first clinical cases presented in the patients were described as cholesteatoma (presentation of progressive growth of the keratinized squamous epithelium). In 1992 it was called a primordial cyst or odontogenic keratocyst. The latest classification of the World Health Organization (WHO) of odontogenic tumors, called odontogenic keratocyst as keratocystic odontogenic tumor, with criteria in the presence of genetic, molecular alterations, which would also be present in some neoplasms.
Even though it still has an unknown etiology, there is a general agreement that odontogenic keratocyst arises from the cellular remains of the dental lamina, in the period of development of odontogenesis, discarding the hypothesis that its formation is through the oral epithelium. This pathology presents a mechanism of growth and biological behavior different from pathologies that are more common to be found in the daily clinical routine due to its aggressive behavior and the high rate of recurrent cases. It is important to mention that there is a high chance of causing morbidity when not diagnosed early. It has a benign nature of slow evolution and aggressive and asymptomatic clinical behavior with predilection for the posterior region and ascending branch of the mandible, being in most cases associated with an included tooth. There are reports of cases that the lesion was presented in the maxilla, but it is not something common. Radiographic signs are only characteristic of the lesion, but histopathological examination should be done to conclude the diagnosis to rule out any possibility of differential diagnosis with other pathologies.
2. LITERATURE REVIEW
CO is a distinct form of developmental odontogenic pathology that requires special considerations because of its clinical behavior, specific histopathological aspects and its high recurrence rate. It is presented in patients of wide age range and has a predilection for males as well as the region of the lower molars (especially in regions of third molars) and in the mandible branch.
2.1 SIGNS AND SYMPTOMS
Signs and symptoms are usually absent, and their discovery is only performed through routine radiographic examinations. In cases of more extensive lesions, tumephation, drainage or associated and local pain, increased volume of soft tissues and bone tissue, parasthesia and mobility of teeth involved by the lesion are identified, characterizing the lesion with slow growth and displacement of dental structures by increasing the loss of bone support.
Amorim et al. (2003) presented an epidemiological evaluation of 26 cases of cysts diagnosed as odontogenic keratocyst and identified mostly the presence of lesions in male patients, with variant ages from forty years and white, located mainly in the posterior region of the mandible. Starting from the time of the evolution of the lesions, it was possible to observe a slow development, with no specific radiographic pattern predominance. In the diagnoses analyzed, it was not identified in most cases something consistent with the histopathological diagnosis, but rather ameloblastoma, being the main lesion cited in the diagnostic hypotheses. (VAROLI et al., 2010)
It is extremely important that the professional evaluates the patient regarding the possibility of Gorlin-Goltz Syndrome, since it is associated with the appearance of multiple keratocysts, plantar and palm alterations and basal cell nevoid carcinomas.
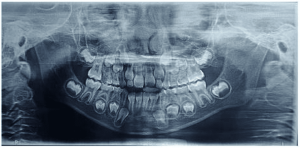
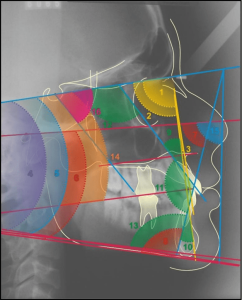
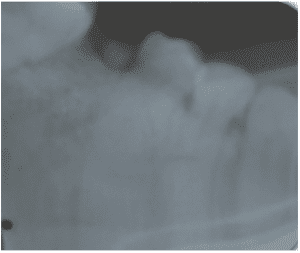
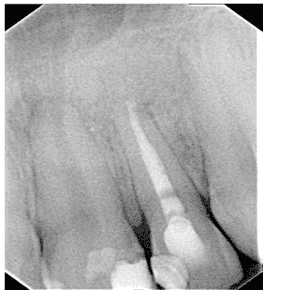
Radiographically, such pathology is seen as a circular or ovoid lesion of radiolucent form – unilocular or multilocular – and regular radiopaque margins, with precise limits (well defined and corticalized). There is rarely the occurrence of root resorption and is associated with an included tooth in 25 to 40% of the cases presented.
2.2 TREATMENT
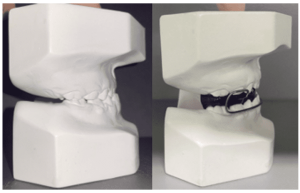
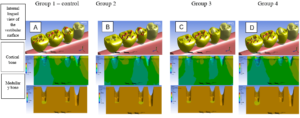
The treatment of CO is of immense challenge for surgeons, considering the high degree of recurrence rate. The patient’s age and the size of the lesion are taken into account for the best selection of the choice of treatment in order to enable the health of the lesion patient. Marsupialization can be used as a form of first-instance treatment, aiming to protect important and noble structures. In a second view, the entire lesion should be removed. The injection of Carnoy solution into the lumen region of the cyst has also been used to detach the cyst from the bone wall, facilitating lesion removal and with lower recurrence rates. It is also done together with enucleation and curettage (GUERRA et al., 2013). Some factors that may be associated with this recurrence are: the presence of satellite cysts that are lost during surgical removal and/or thin and friable capsule, hindering enucleation without fragmentation of the lesion. The CO has a poor prognosis, regardless of which treatment method will be used in its removal, because of its high recurrence rate.
3. Discussion
In order to confirm the diagnosis of CO, it is necessary to perform the histopathological examination (thus, the biopsy examination is performed), because it can be confused with other pathologies such as: ameloblastoma, adenomatoid odontogenic tumor, dentitocyst, calcifying odontogenic cyst and ameloblastic fibroma. Its histopathology presents a well-defined and empalised and hyperchromatic basal cell layer, thin and friable capsule, corrugated parakeratoin, thin fibrous wall and no inflammatory infiltrate as well as absence of interpapillary crests. Stratified squamous epithelium layer is unification with five to seven layers of cells and, in recurrence of the lesion, satellites can be seen in the fibrous capsule.
Chi et al. (2005) reported two cases that presented the occurrence of soft tissue lesions of the intraosseous keratocyst, identified as peripheral odontogenic keratocyst. However, there is a differentiation in the part of the diagnoses regarding the classification of this occurrence in the gingival mucosa, in which some consider it as a histological variant of the gingival cyst, while others believe it to be the peripheral form of the odontogenic keratocyst. (VAROL et al., 2010)
Forssell et al. (1988) analyzed the postoperative period of 75 patients with CO for five years, totaling 43% of cases with poor prognoses because they were relapsed. Recurrences found in patients with Gorlin Syndrome, which is now required for as long as possible follow-up.
Through his study on the genetics of keratocystic odontogenic tumor, Heikinheimo et al. 20 (2007) found that the excessive presence of genes can contribute to the continuous of the keratocystic odontogenic tumor. (VAROLI et al., 2010)
Cases with secondary infection, cortical perforation, and multilocular aspect showed a higher chance of recurrence.
4. CONCLUSION
Currently, due to its aggressiveness, growth potential, neoplastic nature and high recurrence rate, keratocyst or odontogenic keratocyst is termed as an odontogenic tumor. (VAROLI et al., 2010)
In view of all the above mentioned contents, it is of paramount importance to know oral pathologies associated with dental origins by the dentist with the objective of developing a correct and early diagnosis for the best choice of treatment, aiming at the patient’s well-being and promoting health for the patient. Odontogenic keratitis requires appropriate therapeutic procedures for successful treatment. It is indispensable to refer the patient to the histopathological examination, because it is necessary to exclude hypotheses of differential diagnoses associated with other diseases and even the possibility of association with Gorlin-Goltz Syndrome.
5. REFERENCES
AMORIM, RFB, et. al. Ceratocisto odontogênico: estudo epidemiológico de 26 casos. Rev Odontol Ciênc. 2003;18(39): 23-30;
CHI, AC, OWINGS, JR, MULLER, S. Peripheral odontogenic keratocyst: report of two cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99(1):71-8;
FORSSEL, K., et. al. Recurance of keratocysts. A long-term follow-up study. Int J Oral Maxillofac Surg, v.17, n.1, p.25-28, 1988;
FORSSEL, K. The primordial cyst. A clinical radiografic study. Proc Finn Dent Soc, v.76, n.3, p.129-174, 1980;
GUERRA, L., et al. Tratamento conservador de múltiplos tumores odontogênicos ceratocísticos em paciente não sindrômico. Rev. cir. traumatol. buco-maxilo-fac. [online]. 2013, vol.13, n.2, pp. 43-50. ISSN 1808-5210.
GREGORY, C. Cirurgia buco-dento-alveolar. São Paulo: Sarvier, 1996;
MARCUCCI M. Tratamento cirúrgico e terapêutico complementar dos queratocistos odontogênicos: revisão de literatura [Dissertação de Mestrado]. São Paulo: Faculdade de Odontologia USP; 2002;
NEVILLE BW, et. al. Patologia oral maxilofacial. Rio de Janeiro: Ed. Guanabara Koogan; 2004. p. 570-573;
PEIXOTO, R. F. et al. Tumor odontogênico ceratocístico: revisão dos achados atuais. Rev. cir. traumatol. buco-maxilo-fac.,Recife, v.9,n.3,p.21-28 jul.-Set 09;
SHEAR M. Cistos da região bucomaxilofacial – diagnóstico e tratamento. 3. ed. São Paulo: Ed. Santos; 1999;
VAROLI F.P. et al. Tumor odontogênico queratocístico: características intrínsecas e elucidação da nova nomenclatura do queratocisto odontogênico. J Health Sci Inst. 2010;28(1):80-3.
[1] Graduated in Dentistry from Iguaçu University – Campus Nova Iguaçu – RJ. Post graduated from unibf college in temporomandibular dysfunction and orofacial pains and Dental Radiology and Imaging.
Submitted: August, 2020.
Approved: September, 2020.