REVIEW ARTICLE
GOMES, Mariana Amélia Sena [1], SILVA, Kedson de Sousa [2], MEIRA, Gabriela de Figueiredo [3], OLIVEIRA, Nayhane Cristine da Silva de [4]
GOMES, Mariana Amélia Sena. et al. Dental trauma in childhood: integrative review. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year: 08, Issue: 06, Vol. 02, Pages: 179-190. June 2023. ISSN: 2448-0959, Access link: https://www.nucleodoconhecimento.com.br/dentistry/dental-trauma, DOI: 10.32749/nucleodoconhecimento.com.br/dentistry/dental-trauma
ABSTRACT
The aim of this work is to conduct a literature review on aspects of dental trauma in deciduous dentition, based on data found in the PUBMED, LILACS, BBO, and SCIELO databases regarding the proposed topic. Trauma to deciduous teeth occurs in preschool children and is often associated with behavioral traits such as curiosity and restlessness, leading children to explore environments that result in falls, leading to an increased incidence of injuries. The success of post-traumatic care is related to the emergency care provided at the time of the event, as delayed treatment can result in a series of problems according to the trauma suffered. To avoid problems resulting from trauma and delayed treatment, there are protocols and guidelines that can be used in the treatment of dental trauma, with each treatment corresponding to a type of trauma.
Keywords: Dental trauma, Pediatric dentistry, Accident prevention, Health education.
INTRODUCTION
Dental trauma is common in early childhood and is classified by the World Health Organization (WHO) as a public health problem, ranging from small enamel cracks to permanent tooth loss. Traumatized teeth can cause not only aesthetic but also physical and functional damage, with numerous consequences for the health of pediatric patients (MACHADO, 2019).
The damages induced by trauma are varied and can even lead to early loss of teeth, as well as greater occlusal problems if not managed properly. Among the places most likely to experience dental trauma, the school environment was the most prominent, with deciduous teeth and soft tissues adjacent to dental elements being the most affected. The best way to prevent dental trauma is to provide information to parents and teachers about the best course of action for different types of dental trauma (COSTA, 2014).
Emergency care in cases of acute dental trauma can ensure a better prognosis, prevent pulp necrosis, or premature tooth loss. Therefore, the patient should be immediately referred to a dentist so that necessary action can be taken promptly (SANABE, 2019).
Thus, the objective of this work is to conduct a literature review on aspects of dental trauma in deciduous dentition.
METHODOLOGY
This study is an integrative literature review, using various articles from the following databases: Scientific Electronic Library Online (SCIELO), Latin American and Caribbean Literature in Health Sciences (LILACS), Bibliografia Brasileira de Odontologia (BBO), Scholar Google, and National Library of Medicine (PUBMED/Medline). Using the descriptors dental trauma, pediatric dentistry, dentistry, dental trauma, including articles in English and Portuguese. Articles published in the last 5 years were included, such as observational studies, case reports, and literature reviews.
According to the selected descriptors, the initial search resulted in 40 articles (phase 1); thereafter, the following procedures were performed: exclusion of duplicates in the databases (phase 2); titles were read and excluded according to the objectives of this study (phase 3); abstracts were read and exclusions were made according to established criteria (phase 4); the articles used for analysis in this review were read in their entirety (phase 5). At the end of the five phases, a total of 16 studies were obtained to compose the review.
LITERATURE REVIEW
FACTORS ASSOCIATED WITH DENTAL TRAUMA
Cetinbas et al. (2018) state that at different age groups, Dental Trauma (DT) affects both dentitions and is common in early childhood when children learn to crawl, walk, and run, even without motor coordination, and later in childhood, falls, collisions with objects such as furniture, and falling from high places are also common and can lead to DT.
During adolescence, when children engage in sports and recreational activities, there are always exposures that put their physical integrity at risk, with potential for falls or electrical shocks and bicycle accidents (JORGE et al., 2019; ANDERSSON, 2019).
There are other factors that can lead to DT, such as harmful oral habits, oral perforation, iatrogenic injury (medical examination, such as laryngoscopy or during intubation), drugs, and alcohol (GOMES, COSTA, and BONOW, 2019).
CLASSIFICATION OF DENTAL TRAUMA
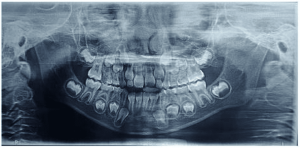
The classification of dental injuries is very important and can be used as a guide to aid in the diagnosis of deciduous and permanent dentitions, providing not only treatment guidance but also possible prognosis. We can classify DTs according to the current Andreasen classification accepted by the WHO (FLORES, 2018; AMORIM et al., 2021).
INJURIES TO SOFT AND HARD TISSUES
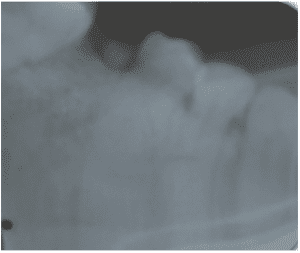
Among the injuries to the hard tissues of the tooth, we can find all injuries that result from enamel cracks, dentin (with or without pulp exposure), and even involving the root. They can be divided into complete and incomplete enamel fractures. Uncomplicated coronal fractures can be divided into: fractures of enamel and dentin without pulp involvement, fractures of enamel with dentin involvement; complex coronal fractures include: coronal fractures without pulp exposure, and crown-root fractures with exposed pulp and root fractures (ANDREASEN and AHRENSBURG, 2019; DIANGELIS et al., 2019; FLORES, 2018).
INJURIES WITH PULP INVOLVEMENT
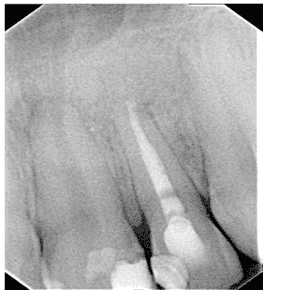
Flores (2018) addresses that fractures involving exposed enamel, dentin, and pulp are uncommon in deciduous teeth. Therefore, a radiographic diagnosis should be performed to assess the extent of the fracture and the stage of root development, as Marinho (2019) states. In very young children with hypoplastic roots, it is important to preserve pulp vitality by performing a partial pulpotomy or overpass pulpal procedure. Pulpotomy treatment involves the complete removal of the coronal pulp and, in this way, preserves the root pulp according to Nino and Del (2018), and the same treatment applies in cases of fully formed roots. Thus, clinical control can be performed in week 1, and clinical and radiographic control can be performed in weeks 6-8 and year 1 (MALMGREN, 2021).
ENAMEL AND DENTIN INJURIES
The most commonly found injuries involve fractures of enamel and dentin with loss of dental structure but without pulp involvement, mainly on the mesial aspect of the upper incisors and may be accompanied by lesions in the supporting tissues. Teeth affected in this way exhibit normal mobility and are not sensitive to percussion. On radiographs, the loss of dentin and enamel can be seen, and the distance between the fracture and the pulp chamber should be evaluated. Therefore, the most suitable treatment for coronal fractures is to completely seal the affected dentin with glass ionomer to prevent microleakage (WANDERLEY and OLIVEIRA, 2019).
POST-TRAUMA RECOMMENDATIONS
Cortes et al. (2018) proposed a more appropriate approach following a traumatic injury. These recommendations include: a soft diet for 10 to 14 days; good oral hygiene, including dental brushing after each meal, using a soft brush. Apply 0.12% chlorhexidine externally, twice a day, for a week. This measure is important to prevent plaque accumulation. Limiting pacifier use is advisable as it can influence tissue healing after trauma and the pulp prognosis of traumatized teeth due to suction forces. Parents should be informed about possible complications such as inflammation, discoloration of the crown, increased mobility, or fistula, and should be vigilant for signs of gum inflammation as well as the possibility of complications in the development of permanent successor teeth, especially in cases of intrusion and avulsion in children under 3 years old (COSTA et al., 2021).
TREATMENT OPTION
Replantation of permanent teeth is a conservative approach that aims to reposition the avulsed tooth in its own alveolar bone and should be considered the treatment of choice. The time the tooth remains out of the socket should be as short as possible to achieve the best treatment effect within the first 30 minutes and provide a better prognosis. However, the study authors propose various time intervals for teeth outside the socket. According to this research, the trauma-to-treatment interval is at least 15 minutes, which is considered non-critical (BLAKYTNY et al., 2021).
RESULTS AND DISCUSSION
Without proper treatment, children with dental trauma can experience a negative impact on their quality of life, suffering from low self-esteem and problems in personal and social relationships (BLAKYTNY et al., 2021).
Thus, the most affected age range in childhood is 1 to 3 years, which is related to factors like motor coordination, spongy and plastic bones. According to Souza et al. (2018) and Menegotto et al. (2017), the highest prevalence among children was in the age range of 7 to 12 years.
Contrary to this, focusing on a treatment approach, for permanent tooth trauma, Rebouças, Neto, and Sousa (2018) stated that the ideal time for dental replantation should be at least 15 to 30 minutes to ensure patient safety.
Continuing this line of thought, Guedes-Pinto et al. (2018) and Melo (2017) observed that damage to the periodontal ligament cells is a consequence of the extra-alveolar phase, meaning the time between avulsion and dental replantation, and environmental factors are involved. The teeth should be preserved because periodontal ligament cells are unable to multiply and differentiate into fibroblasts, especially if stored in a dry environment for more than 15 minutes. A deciduous tooth that has been avulsed should not be repositioned in the socket, as permanent damage can lead to complications such as bacterial infection, abscess formation, mobility, ankylosis, prolonged retention, and inflammatory resorption, contraindicating dental replantation (GUEDES-PINTO et al., 2018; MACHADO, 2019).
On the other hand, in cases of dental trauma, parents and/or caregivers are often laypersons and may make decisions that compromise the treatment and prognosis of traumatized teeth. Therefore, means of dental storage, extra-alveolar time, trauma, time to dentist consultation, accurate diagnosis, intraoral and extraoral exams are factors directly related to trauma treatment. In this situation, dentists must effectively communicate knowledge about dental trauma and the appropriate actions to take in each case to those who interact with children on a daily basis or are involved in accidents (BRANDÉO, 2020; SOUSA, 2018).
Silva et al. (2017) reported that after trauma involving avulsion, the remaining periodontal ligament cells on the root surface are deprived of blood supply and lose stored cellular metabolites. To maintain physiological cellular metabolism, these nutrients must be supplemented as quickly as possible. An ideal storage medium should maintain physiological pH, metabolism, and osmolarity to preserve the vigor and vitality of periodontal fibers while the tooth is transported to the dental office. Regarding extra-alveolar time, in this scientific study, parents and/or caregivers (68.7%) reported taking up to 30 minutes to seek treatment for their traumatized child. One of the most intriguing current challenges in dental traumatology is finding the best transport medium for cellular viability, both periodontal and endodontic, presenting antioxidant properties that neutralize biotic contamination, with pH and osmolarity values similar to those of the tooth, and being cost-effective and accessible (SANABE, 2019).
Thus, it is understood that the success of dental trauma treatment begins minutes after the accident and depends on the proper execution of emergency care provided on-site until the correct diagnosis is made by the dentist using accurate records and intraoral and extraoral exams, thereby promoting the correct case management behavior. Therefore, the success of post-traumatic care is related to the emergency care provided at the time of the event (ALBUQUERQUE et al., 2018).
Therefore, currently, there seems to be no consensus in the literature on the ideal pattern of tooth movement. In cases where the tooth is not attended to by a dentist in a short period, the tooth may suffer alterations in supporting structures, discoloration, and even the vitality of the element, depending on the trauma. Thus, some consequences of dental trauma are frequently recognized as dental problems (FLORES, 2021; TRAEBERT and CLAUDINO, 2018).
There are protocols that can be used to guide dental trauma treatment. For example, in cases of enamel fracture or enamel and dentin fracture, the fragment should be stored in physiological saline for later bonding. When this technique is not possible, restoration with composite resin is indicated. In cases of coronal fractures with pulp involvement, for a good prognosis, treatment should occur within three hours of the trauma, and any fragments should be bonded after initial emergency treatment, whenever possible. In cases of coronoradicular fractures involving enamel, dentin, cementum, and pulp, horizontally, the tooth can be preserved by repositioning it correctly and following with endodontic treatment to prevent pulp necrosis. But if the fracture is vertical, extraction is the only option (SILVA et al., 2020).
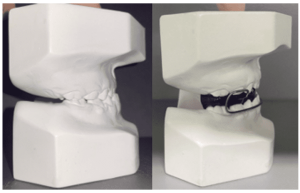
Silva et al. (2020) also affirm that in cases of root fractures involving dentin, cementum, and pulp, tooth mobility can occur, and repositioning of the
tooth should be done, followed by stabilization, and endodontic treatment might be necessary. In cases of fractures of the alveolar wall and process involving the bone, the fragment should be repositioned, and rigid or semi-rigid stabilization should be applied for four weeks.
Pulp capping or partial pulpotomy is recommended when pulp involvement occurs in trauma. For complete root formation, pulpectomy is recommended. There are also guidelines for the treatment of luxation injuries, such as: concussion, only monitoring pulp vitality for about 1 year; subluxations, stabilizing the tooth with a flexible splint for two weeks; complete root formation, endodontic treatment is indicated; lateral luxation, manually or with forceps, the tooth should be repositioned, with four weeks of stabilization, and pulp vitality monitored; intrusion, eruption should be allowed to happen without intervention, but if the tooth has intruded more than 7 mm, repositioning with orthodontic or surgical treatment is recommended (FONSECA et al., 2021).
CONCLUSION
The results of this study present the main treatments for dental trauma, with children being the most affected group, and dental replantation being one of the options. However, the lack of knowledge among parents/guardians can compromise the quality and effectiveness of treatment. Therefore, dental professionals should guide parents and teach them the best course of action in the event of accidents leading to dental trauma.
The success of post-traumatic care is related to the emergency care provided at the time of the event. In case of delayed treatment, teeth can suffer various issues depending on the trauma suffered. To avoid problems arising from trauma and treatment delays, there are protocols and guidelines that can be followed for dental trauma treatment, with each action corresponding to a specific type of trauma.
Further research is needed in this area to distribute more information about childhood dental trauma, and corrective and educational public policies should be developed to reduce accidents that can cause trauma and ensure correct post-trauma actions.
REFERENCES
ALBUQUERQUE, Camila Moraes et al. Principais técnicas de controle de comportamento em Odontopediatria. Arquivos em odontologia, v. 46, ed. 2, p. 110-115, 2018.
AMORIM, Lilian de Fátima Guedes et al. Estudo retrospectivo de lesões dentárias traumáticas em dentes decíduos em clínica pediátrica brasileira especializada. Traumatologia Dentária, v. 27, ed. 5, pág. 368-373, 2021.
ANDERSSON, Lars. Guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dental Traumatology, v. 28, ed. 2, p. 88–96, 2019.
ANDREASEN, Jens Ove; AHRENSBURG, Soren Steno. História do guia de trauma dental. Traumatologia Dentária, v. 28, ed. 5, pág. 336-344, 2019.
BLAKYTNY, Thomas et al. Avulsed permanent incisors: knowledge and attitudes of primary school teachers with regard to emergency management. International journal of paediatric dentistry, v. 11, ed. 5, p. 327-332, 2021.
CETINBAŞ, Tugba et al. The relationship between sports activities and permanent incisor crown fractures in a group of school children aged 7-9 and 11-13 in Ankara, Turkey. Dental Traumatology, v. 24, ed. 5, p. 532-536, 2018.
CORTES, Maria Ilma de Souza et al. Impact of traumatic injuries to the permanent teeth on the oral health-related quality of life in 12-14-year-old children. Community Dentistry and Oral Epidemiology, 30, ed. 3, p. 193–8, 2018.
COSTA, Luciana Ellen Dantas. Trauma dentário na infância: avaliação da conduta dos educadores de creches públicas de Patos-PB, Rev odontol unesp., v. 43, ed. 6, p. 402-08, 2014.
COSTA, Luciane Ribeiro de Rezende Sucasas da et al. Traumatismo na Dentição Decídua. Odontopediatria na Primeira Infância, ed. 3, p. 689-714, 2021.
DIANGELIS, Anthony et al. Guidelines for the Management of Traumatic Dental Injuries: 1. Fractures and Luxations of Permanent Teeth. Pediatr Dent, v. 38, ed. 6, p. 358-368, 2019.
FLORES, Marie Therese et al. Guidelines for the management of traumatic dental injuries. III. Primary teeth. Dental Traumatology, v. 23, ed. 4, p. 196-202, 2021.
FLORES, Marie Therese et al. Guidelines for the management of traumatic dental injuries. I. Fractures and luxations of permanent teeth. Endodontic Topics, v. 14, ed. 1, p. 102-110, 2018.
FONSECA, Carlissya Alves et al. Tratamento das lesões dentárias traumáticas: perspectivas atuais. Brazilian Journal of Development, v. 7, ed. 4, p. 38121-38126, 2021.
GOMES, Genara Brum; COSTA, Catiara Terra; BONOW, Maria Laura Menezes. Traumatic intrusion of permanent teeth: 10 years follow‐up of 2 cases. Dental traumatology, v. 29, ed. 2, p. 165-169, 2019.
GUEDES-PINTO, Antônio Carlos et al. Manual de odontopediatria. Manual de Odontopediatria, São Paulo: Santos. 2018.
JORGE, Kelly Oliva et al. Prevalence and factors associated to dental trauma in infants 1–3 years of age. Dental traumatology, v. 25, ed. 2, p. 185-189, 2019.
MACHADO, João Victor Melo et al. Prevalência de lesões traumáticas em crianças assistidas no programa bebê clínica: universidade vale do rio doce no período de 2010 a 2015. Revista Científica FACS, v. 19, ed. 23, p. 104-113, 2019.
MALMGREN, Barbro et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 3. Injuries in the primary dentition. Dental Traumatology, v. 28, ed. 3, p. 174-182, 2021.
MARINHO, Clarisse da Silva et al. Impacto do traumatismo dentário na qualidade de vida de crianças, adolescentes e suas famílias: revisão crítica da literatura. Arquivos em Odontologia, v. 55, 2019.
MENEGOTTO, Alessandra et al. Avaliação do conhecimento dos professores de escolas públicas quanto ao manejo da avulsão dentária em crianças. Revista perspectiva: ciência e saúde, v. 2, ed. 1, p. 83-84, 2017.
NIÑO, Vaquero; POZO, Paloma Planells Del. Evolución de los protocolos de la International Association of Dental Traumatology (IADT) para la evolución y manejo de los traumatismos dentales. Odontol Pediátr (Madrid), v. 20, ed. 2, p. 134-145, 2018.
REBOUÇAS, Pedro Diniz; NETO, José Jeová Siebra Moreira; SOUSA, Denise Lins. Fatores que influenciam no sucesso do reimplante dental. Publicatio UEPG: Ciências Biológicas e da Saúde, v. 19, ed. 1, p. 31-37, 2018.
SANABE, Mariane Emi et al. Urgências em traumatismos dentários: classificação, características e procedimentos. Revista Paulista de Pediatria, v. 27, p. 447-451, 2019.
SILVA, Maurício Bacarin et al. Avaliação do conhecimento da abordagem de trauma dental pelos profissionais de creches. ConScientiae Saúde, v. 8, ed. 1, p. 65-73, 2017.
SILVA, Yuri Cássio de Lima et al. Epidemiologia e tratamento do traumatismo dentoalveolar em crianças e adolescentes: uma revisão da literatura. Brazilian Journal of Development, v. 6, ed. 7, p. 43814-43822, 2020.
SOUSA, Denise Lins et al. Prevalência de trauma dental em crianças atendidas na Universidade Federal do Ceará. Revista Odonto ciência, v. 23, ed. 4, 2018.
SOUZA, Juliana Garcia Mugnai Vieira et al. Conhecimento dos responsáveis das crianças atendidas na clínica odontológica da unipar campus cascavel-pr sobre traumatismo alvéolo dentário. Odontologia Clínico-Científica, v. 17, ed. 1, p. 39 – 44, 2018.
TRAEBERT, Jefferson; CLAUDINO, Dikson. Epidemiologia do traumatismo dentário em crianças: a produção científica brasileira. Pesquisa brasileira em odontopediatria e clínica integrada, v. 12, ed. 2, p. 263-272, 2018.
WANDERLEY, Márcia Turolla; OLIVEIRA, Luciana Butini. Lesões Traumáticas na Dentição Decídua. Odontopediatria-Fundamentos em Odontologia, ed. 1, p. 301-28, 2018.
[1] Bachelor’s degree in Dentistry from Fametro University Center. ORCID: 0009-0008-2036-7455. Lattes Curriculum: http://lattes.cnpq.br/7064391656930511.
[2] Bachelor’s degree in Dentistry from Fametro University Center. ORCID: 0009-0008-8376-7923.
[3] Ph.D. in Pediatric Dentistry from Federal University of Santa Maria (2020); Master’s degree in Dental Sciences from Federal University of Amazonas (2016); Specialist in Orthodontics from Ceproeducar (2020); Specialist in Public Health from Unyleya College (2018); Bachelor’s degree in Dentistry from Federal University of Amazonas (2013). ORCID: 0000-0002-8285-8769. Lattes Curriculum: http://lattes.cnpq.br/3710771916871688.
[4] Advisor. Specialization in Pediatric Dentistry from Blauro Cardoso de Mattos Institute of Higher Education (2020), Bachelor’s degree in Dentistry from Federal University of Amazonas (2018). ORCID: 0000-0003-2056-5853. Lattes Curriculum: http://lattes.cnpq.br/2255456614872519.
Submitted: May 23, 2023.
Approved: June 6, 2023.