CASE REPORT
PESSOA, Juliana Victória de Sousa [1], ARAÚJO, Marhia Eduarda Vilela de [2], CAMPOS, Gabrielly Caldeira [3], COSTA, Maria Beatriz Tavares da [4], ARAUJO, Priscila Pinto Brandão de [5], ALVES FILHO, Ary de Oliveira [6]
PESSOA, Juliana Victória de Sousa. et al. Use of Balters’ Bionator in the treatment of anterior crossbite in deciduous dentition: a case report. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year. 08, Ed. 08, Vol. 02, pp. 05-35. August 2023. ISSN: 2448-0959, Access link: https://www.nucleodoconhecimento.com.br/dentistry/use-of-balters-bionator, DOI: 10.32749/nucleodoconhecimento.com.br/dentistry/use-of-balters-bionator
ABSTRACT
Malocclusion is the third most important oral health issue, affecting children, adolescents, and adults. It has a multifactorial etiology, compromising aesthetics, function, and quality of life. Anterior crossbite occurs when the lower teeth occlude in front of the upper teeth. Early treatment, when correctly diagnosed, is always recommended. The purpose of this work was to describe a clinical case of facial orthopedic treatment in a five-year-old female patient, presenting a complete set of deciduous dentition along with anterior crossbite and deep bite. The treatment was carried out using a modified Bionator de Balters appliance for Class III treatment, with a duration of six months. The use of this appliance aimed at maxillary expansion, vestibularization of upper incisors, and control of mandibular growth. This approach achieved favorable results in the treatment of the condition. However, there is still a recommendation for the continuous use of the appliance due to the patient’s growth period and transition between dentitions. The appliance is cost-effective, causes minimal discomfort, and is easy to use. This study demonstrated the importance of early diagnosis, prevention, and treatment of anterior crossbite, with a successful clinical outcome in interceptive and orthopedic treatment, preventing complications, future treatments, and difficulties in subsequent interventions.
Keywords: Anterior crossbite, Bionator de Balters, Deciduous dentition, Facial orthopedics.
1. INTRODUCTION
The World Health Organization (WHO) considers malocclusion one of the most significant oral health problems, after cavities and periodontal disease (SANTOS et al., 2012). Moreira (2016) states that malocclusion occurs due to a disharmony in the development of the craniofacial complex affecting the jaws, tongue, and facial muscles. It has a multifactorial etiology and can cause aesthetic and functional alterations that lead to psychosocial consequences.
Results from the SB Brasil 2010 epidemiological survey (Brasil, 2011) demonstrated that malocclusion is a relevant public health problem in Brazil, with anterior crossbite present in about 3% of the population. The distribution of malocclusions may vary according to factors such as geographical region, age, and socioeconomic conditions.
Thomas and Valença (2005) found a prevalence of 71.4% of malocclusion in the deciduous dentition of preschoolers in São Luís, Maranhão, where only 28.6% of the 1,056 volunteers had a normal occlusion. According to Spilla et al. (2007), the prevalence of anterior crossbite in deciduous dentition ranged from 0.3% to 16%, being more frequent in melanoderm individuals when compared to leucoderm individuals. In Araujo et al.’s study (2018), anterior crossbite was present in 6.2% of the preschoolers analyzed in Belém, Pará.
Anterior crossbite is a malocclusion resulting from the lingual positioning of the upper anterior teeth in relation to the lower anterior teeth and can occur in the deciduous, mixed, or permanent dentition (ARAUJO et al., 2012).
According to Almeida et al. (2011), it can be classified as dental, due to the incorrect inclination of the upper and lower incisors; functional, when there is an occlusal interference that deviates the mandible anteriorly; and skeletal when associated with a discrepancy between the maxilla and mandible.
Santos et al. (2012) stated that those classified as dental or functional could be treated early with interceptive orthodontic appliances.
The early orthodontic approach to pediatric patients points to the responsibility of the dentist in clarifying to parents the long-term consequences of this condition. Aesthetic interest combined with good adherence from both parents and the patient leads to an early search for treatment and assists in the success of the treatment. The rebalancing of bone bases aimed at by the treatment favors the correct development of craniofacial structures and occlusion, as well as aesthetic and functional improvement, as in the case described by Ramadan and Santamaria Júnior (2018).
According to Santos et al. (2012) and Tashima et al. (2003), various devices are used to correct the anterior crossbite condition, such as removable devices with springs, fixed correctors, individual inclined planes, and even the use of a wooden spatula. Each treatment has its advantages and disadvantages, and the prognosis depends on the patient’s age, degree of cooperation, and etiological factor involved. The presented treatments are effective in their respective indications, and the success of the therapy is linked to the professional competence of the specialist in determining the most appropriate one.
The appliance proposed by Wilhelm Balters as a modification of Andresen’s activator comes in various variations, promoting maxillary expansion, vestibularization of upper incisors, mandibular growth containment, and release of the buccal mucosa. The clinical indications for this device align with the presented characteristics, that is, patients in the growth and craniofacial development phase.
The objective of this study is to describe a clinical case of a pediatric patient with deciduous dentition and anterior crossbite, performing the initial treatment of this malocclusion with Balters Class III orthopedic appliance.
2. CASE REPORT
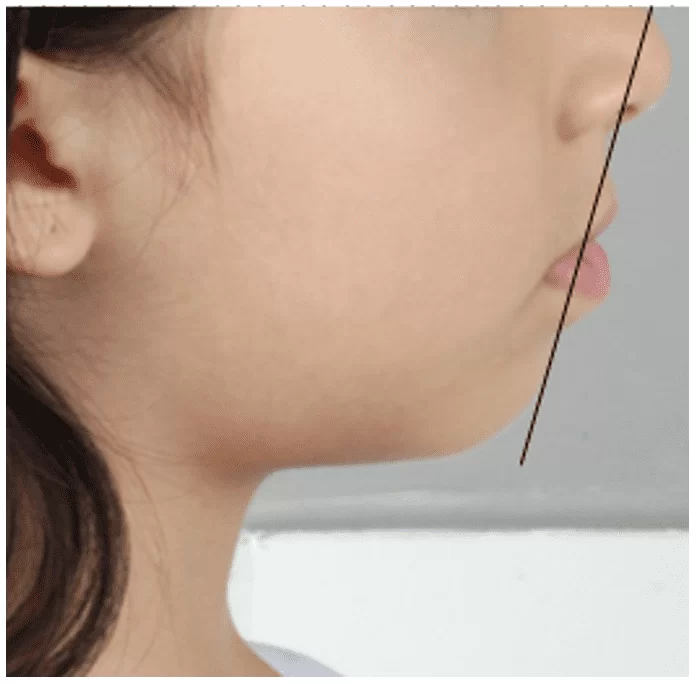
A 5-year-old female patient, of leucodermic ethnicity, Brazilian, originally from Amazonas, attended the Pediatric Dentistry Clinic of the Faculty of Dentistry at the Federal University of Amazonas (FAO-UFAM), accompanied by her guardian, due to a previous diagnosis made in the private healthcare network. During the anamnesis, the patient’s guardian reported that she had been followed in the private healthcare network where she was diagnosed with Class III malocclusion. In the initial frontal facial analysis, a symmetrical face was observed, with a mesofacial morphological type (Figure 7), and a slightly convex profile was noted, as evidenced by soft tissue analysis.
Regarding the lips (Figure 8), the upper lip was +3 mm (standard mean – 0 mm) ahead of the line from the soft pogonion to the middle of the nose (Line S), while the lower lip was +4 mm (standard mean – 0 mm) ahead.
Following the protocol of the mentioned Clinic, the patient’s anamnesis was collected, including a description of the chief complaint, current medical history, personal history, family history, investigation of dietary habits, and oral hygiene habits (GUEDES-PINTO, 2016). The guardian signed the IC (informed consent) of the university, granting permission for data disclosure for academic purposes.
Figure 7 – Patient’s initial condition in frontal and lateral views

Due to being a minor patient, the anamnesis was conducted in a way that the collected information was provided by the legal guardian, her mother.
Regarding the patient’s overall health condition, the legal guardian denied any illnesses during early childhood such as chickenpox, rubella, measles, etc. She also denied any surgical procedures, episodes of trauma, medication allergies, and/or food allergies.
Figure 8 – Initial lip analysis
The mother reported pneumonia at 5 months of age, requiring hospitalization, and in the past dental history, she informed about professional prophylaxis, restorations, and pulpotomy on tooth 84. Regarding the patient’s family history, she denied any diseases, signing the Informed Consent Form.
After the anamnesis, the patient was examined through extraoral physical examination, including TMJ inspection, palpation of cervical-facial lymph nodes, and sinuses, without any abnormalities.
Next, she was examined through intraoral physical examination, inspecting and palpating the soft tissues of the oral cavity, and direct examination of the dental units, previously cleaned through professional prophylaxis and dried, under good lighting.
At this stage, soft tissue alterations and the recording of present cavitated or non-cavitated, active or inactive caries lesions were noted on an appropriate clinical chart.
During the intraoral clinical examination, in Figure 8, the presence of all deciduous teeth in the oral cavity was observed (Figure 9).
The patient had a canine key (55 and 65) in Class I (when the cusp of the upper canine occludes in the embrasure between the lower deciduous canine and the lower deciduous first molar), passive lip seal, and nasal breathing.
She also had a mesial step left terminal plane (Figure 10) and a straight right terminal plane (Figure 11), causing a slight deviation of the jaw to the left.
In addition to the clinical condition of anterior crossbite affecting teeth 73,72,71,81, and 82.
Figure 9 – Initial occlusal clinical condition of the upper and lower arches

Figure 10 – Mesial step terminal plane on the left side

Figure 11 – Straight terminal plane on the right side

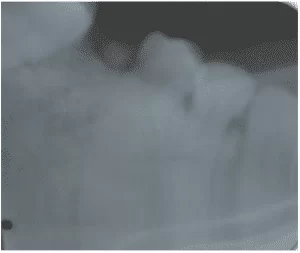
In the panoramic radiograph (Figure 12), absence of dental germs for elements 18, 28, 38, and 48 was observed; presence of forming dental germs for elements 17, 16, 15, 14, 13, 12, 11, 21, 22, 23, 24, 25, 26, 27, 37, 36, 35, 34, 33, 32, 31, 41, 42, 43, 44, 45, 46, and 47; normal bone level of the dental elements; radiolucent image suggestive of dental caries/infiltration in element 84, which was subjected to a pulpotomy procedure; contours of the right and left orbits’ floors without significant alterations; well-developed and normoarated maxillary sinuses, with alveolar extension on the right and left sides; nasal conchae with normal contours and size; intact septal nasal without significant deviation; bony elements with normal radiopacity and contours; absence of bone fractures; intact condyles, coronoid processes, tubercles, and articular eminences with normal radiopacity, in addition to other anatomical structures within radiographic patterns of normality.
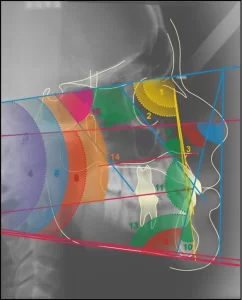
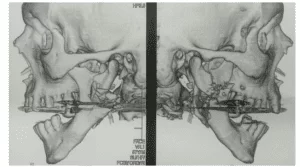
As a complementary and crucial examination to confirm the occlusal and skeletal condition of the patient, an initial teleradiography was performed (Figure 13) along with an initial cephalometric analysis (Figure 14).
Figure 12 – Initial Panoramic Radiograph
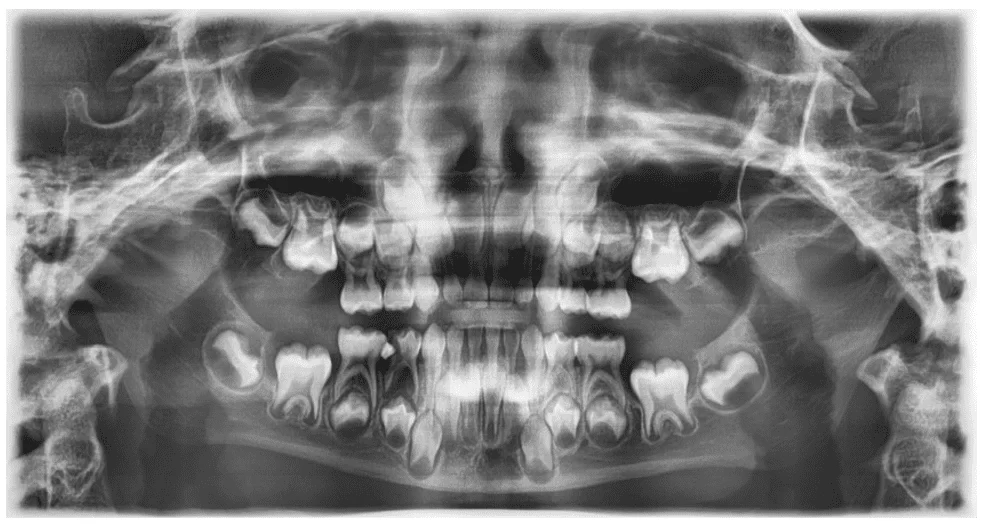
Figure 13 – Initial Lateral Cephalometric Radiograph
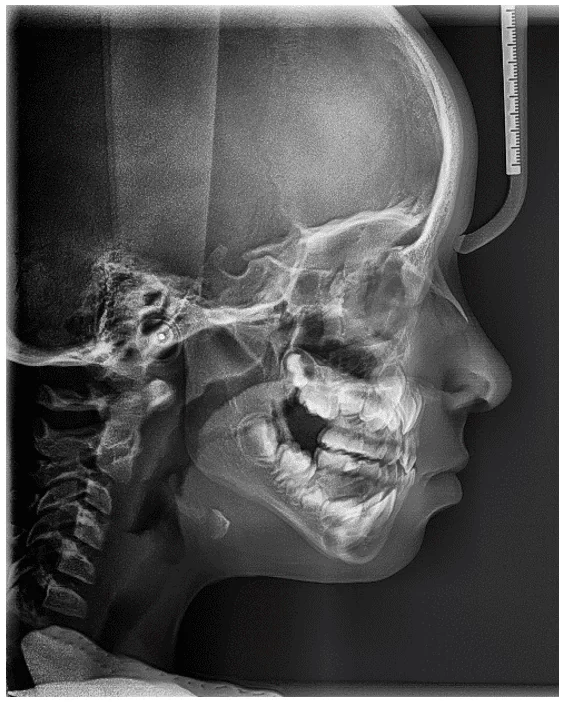
Figure 14 – Cephalometric Tracing Initial Aspect
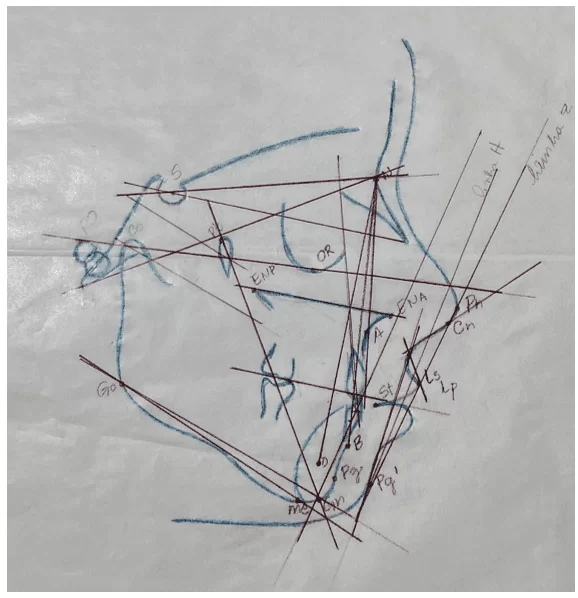
The values obtained in the cephalometric analysis were organized according to the following table:
Table 1 – Initial Cephalometric Analysis – University of São Paulo (USP) Standard
| DESCRIPTION | PARAMETER | STANDARD | INITIAL | RESULTS |
| Skeletal Cephalic Standard | S-N.Gn | 67°± 3° | 69° | Retruded mandible |
| S-N.Go-Me | 32°± 4° | 36° | Tendency for significantly vertical growth | |
| S-N.Plo | 14° | 17° | Tendency for vertical growth | |
| FMA | 25°± 5° | 24° | Tendency for balanced growth | |
| N.Ba-Pt.Gn | 90°± 3° | 90° | Mesofacial morphological type | |
| Relation of apical bases | SNA | 82°± 2° | 82° | Well-positioned maxilla |
| SNB | 80°± 2° | 79° | Well-positioned mandible | |
| ANB | 2°± 2° | 3° | Class I skeletal | |
| SND | 76° | 73° | Retruded mandible | |
| Dentes
x Apical bases |
1.NA | 22° | 11° | Sup. lingualized incisors |
| 1.NB | 25° | 20° | Inf. lingualized incisors | |
| 1-NA | 4mm | 1mm | Retracted upper incisors | |
| 1-NB | 4mm | 3mm | Slightly retruded lower incisors | |
| Interincisal angle | 131° | 150° | Biprotrusion of teeth | |
| Skeletal profile
x Soft tissue profile |
Z-angle | 80° | 68° | Retruded mandible and convex profile |
| Nasolabial | 95°-110° | 100° | Harmonic profile | |
| S line |
0/0 mm
|
3 mm
4mm |
Protruded upper lip
Protruded lower lip |
Source: Own (2023).
Adding the legend with the meaning of the abbreviations – these are specific characteristics of the cephalometric tracing, language used by orthodontists… I don’t find it necessary. It would be a very extensive legend.
2.1 THERAPEUTIC PROCEDURE CARRIED OUT
After conducting the facial and cephalometric analyses, the case was planned for a single-phase treatment. This phase consisted of using the modified Balters Bionator appliance for Class III treatment.
For this purpose, impressions of the upper and lower arches were taken, and a bite registration was made using wax 7, which was sent to the laboratory. Digital springs were included in the instructions to facilitate the vestibular movement of the incisors and expedite the correction of this malocclusion.
The patient and the guardian received instructions regarding appliance hygiene procedures, and they were advised to wear it continuously for at least 15 hours a day, as recommended by Giancotti et al. (2003). The appliance was not to be worn during school activities or while sleeping to avoid the risk of loss or breakage.
The appliance was installed in December 2022 (Figures 15 and 16), and the patient wore it until June 2023. However, due to the breakage of the digital springs, the need for a new appliance that could accompany the patient for a longer period was assessed.
The treatment lasted for six months, and during the monthly check-ups, adaptation and maxillary expansion were assessed through Coffin spring activation.
An activation protocol of 0.5 mm was followed at each maintenance appointment, with activation at the helix.
Figure 15 – Side view photographs highlighting the maxillary lift achieved by the appliance installation
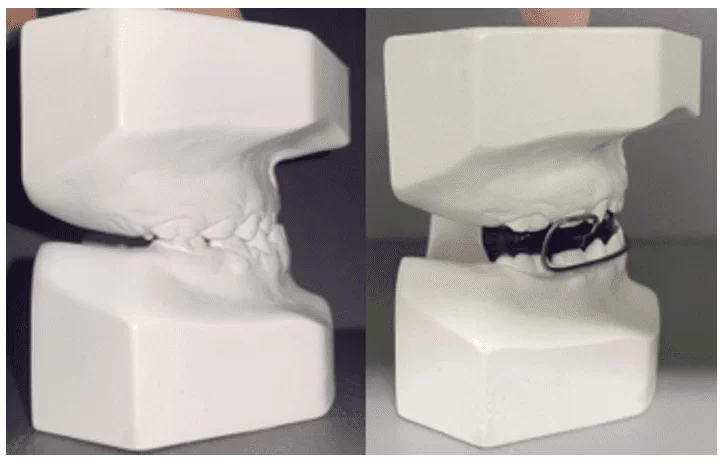
Figure 16 – Appliance installation and activation in December 2022

After three months of treatment, it was possible to observe the repositioning of the incisors in an edge-to-edge relationship (Figure 17).
Figure 17 – Follow-up photograph after three months of treatment

2.2 RESULTS OBTAINED
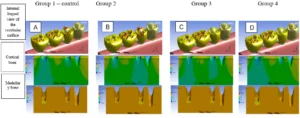
After six months of treatment, we summarize the follow-up photographs of the case, illustrated in Figures 18, 20, 21, and 22. We emphasize the lateral cephalometric radiograph shown in Figure 23 and the final cephalometric analysis presented in Figure 24, the results of which are displayed in Table 2.
The final lip analysis in Figure 19 indicated a protrusion of 2 mm of the upper lip and a protrusion of 3 mm of the lower lip in relation to Line S.
Figure 18 – Final condition of the patient in frontal and lateral view

Figure 19 – Final lip analysis

Figure 20 – Final occlusal condition

Figure 21 – Final right terminal plane

Figure 22 – Left terminal plane, final aspect

Figure 23 – Final lateral cephalometric radiograph

Figure 24 – Final cephalometric tracing
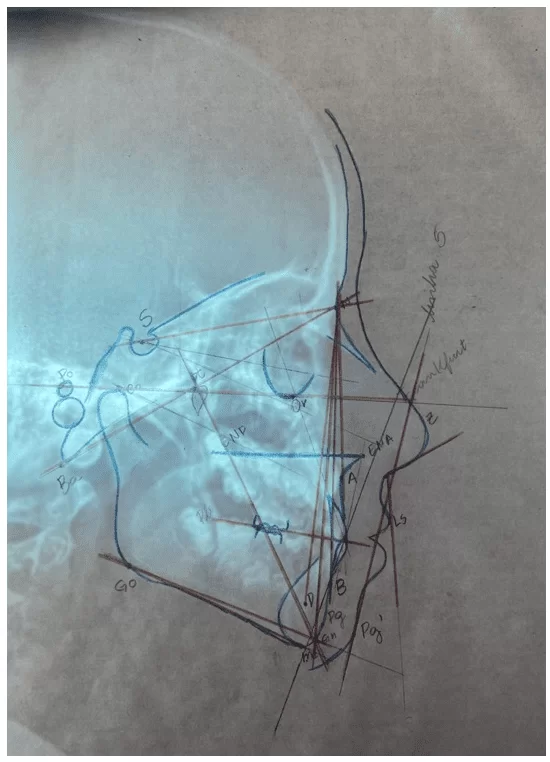
Table 2 – Comparison between initial and final cephalometric analysis – USP standard
| DESCRIPTION | MEASURE | PATTERN | INITIAL | POST-BIONATOR | VARIATION |
| Skeletal Cephalic Pattern | S-N.Gn | 67°± 3 | 69° | 70° | +1° |
| S-N.Go-Me | 32° ± 4 | 36° | 34° | -2° | |
| S-N.Plo | 14° | 17° | 21° | +4° | |
| FMA | 25°± 5° | 24° | 28° | +4° | |
| N.Ba-Pt.Gn | 90° ± 3 | 90° | 85° | -5° | |
| Relation of Apical Bases | SNA | 82°± 2° | 82° | 82° | Ø |
| SNB | 80°± 2° | 79° | 83° | +4° | |
| ANB | 2°± 2° | 3° | 3° | Ø | |
| SND | 76° | 73° | 74° | +1° | |
| Dentition
x Apical bases |
1.NA | 22° | 11° | 17° | +6° |
| 1.NB | 25° | 20° | 18° | -2° | |
| 1-NA | 4 mm | 1 mm | 1 mm | Ø | |
| 1-NB | 4 mm | 3 mm | 4 mm | +1 mm | |
| Interincisal Angle | 131° | 150° | 140° | -10° | |
| Skeletal Profile
x Soft Tissue Profile |
Z Angle | 80° | 68° | 78° | +10° |
| Nasolabial | 95°-110° | 100° | 116° | +16° | |
| S Line |
0/0 mm
|
3 mm
4 mm |
2 mm
3 mm |
-1mm
-1mm |
Source: Own (2023).
For didactic purposes, in order to better express the variation in measurements after appliance use, the variation before intervention was calculated, consisting of the subtraction between the final value after treatment and the initial value. Since the goal of the study was to assess the patient’s progress from a clinical perspective, data presentation is numerical but should be analyzed qualitatively. Thus, observing positive variations in the S-N.Go-Me, N.Ba-Pt.Gn, 1.NB, and Interincisal angles, and negative variations in the S-N.Gn, S-N.Plo, FMA, SNB, SND, 1.NA, Z angle, and nasolabial angle.
The post-Bionator cephalometric analysis revealed an increase in the S-N.Gn angles, formed by the intersection of the cranial base line with the most anterior point of the mandible, SN.Plo, formed by the intersection of the cranial base line with the occlusal plane, and FMA, formed by the intersection between the Frankfurt plane and the mandibular plane, indicating an increase in the tendency for vertical growth, which can be justified by the bite rise, which loses depth until almost reaching a near edge-to-edge relationship.
The decrease in the N.Ba-Pt.Gn angle, which determines the facial axis by 5°, corroborates the increase in the above-mentioned tendency for vertical growth, showing a clockwise rotation of the mandible.
The maintenance of the well-positioned maxilla in relation to the cranial base evidenced by the SNA angle, followed by the increase in the SNB angle, demonstrates slight mandibular protrusion, with growth restraint provided by the buccal loop of the appliance.
Regarding the dental elements and their bony bases, the labial movement of the upper incisors described by the increase in the 1.NA angle and the lingualization of the lower incisors described by the reduction in the 1.NB angle combine to transition from a previously crossbite and deep bite to an edge-to-edge bite. The 10° reduction in the Interincisal angle supports the earlier information about moving the elements to a more favorable and less verticalized position.
The soft tissue analysis shows an improved profile, expressed by a 10° increase in the Z angle, formed by the profile line and the Frankfurt horizontal plane. The increase in the Nasolabial angle shows a straighter and more balanced profile, and the 1mm reduction in the upper and lower lips with respect to the S line, which passes through the soft pogonion, the most anterior part of the lips and the midpoint of the nose, indicates a reduction in lip protrusion.
Treatment with the modified Balters Bionator appliance for Class III correction showed significant results in correcting the anterior crossbite condition in the deciduous dentition, even in a short period. Considering the patient’s young age, the incomplete resolution of the condition, the onset of permanent first molar eruption, and the unfavorable lingual inclination of the permanent incisors observed in the final lateral cephalogram, we chose to continue treatment with the patient under the care of this educational institution.
Treatment will continue with monthly activations, with the expectation of using the appliance for at least 15 hours a day. It is hoped that during the transitional period between the deciduous and mixed dentition, the appliance will provide a more favorable environment for treating the condition, as well as vestibular impulsion of the permanent upper incisors through the digital springs, uncrossing the involved elements.
3. DISCUSSION
Araújo et al. (2023) stated that the treatment of malocclusions should be addressed as a public health intervention, aiming to correct this condition as soon as possible to benefit oral and overall health. Occlusal pathologies not only compromise mastication, speech, temporomandibular joint function, and cause headaches but also hinder proper hygiene and increase susceptibility to carious lesions and periodontal diseases. On the other hand, early treatment can reduce costs and long-term invasive approaches, prevent future complications, and improve quality of life in terms of the aesthetic and psychological aspects of the condition.
According to Zegan et al. (2015), anterior crossbite is a condition that requires early treatment as it does not self-correct. Wiedel and Bondemark (2015) and Fernandes et al. (2019) argue that non-treatment can lead to the development of a true Class III or persistence of the condition. Staderini et al. (2020) suggest its approach only in cases where occlusal interference may evolve into a Class III growth pattern.
The literature advocates for the approach to anterior crossbite through removable or fixed appliances, ranging from isolated orthodontic treatment, orthopedic treatment, or a combination of both. According to Azamian and Shirban (2016), various types of devices can be used during the growth phase to correct Class III malocclusion, such as the approach with elastics and skeletal anchorage, Bionator III and Frankel III appliances, reverse Twin Block, Eschler, Facemask, flat tracks, and others.
Khalaf and Mando (2020) claimed that there is weak scientific evidence that fixed appliances were more cost-effective than removable ones in the treatment of anterior crossbite, and there was no significant change in treatment stability in the long term. An advantage presented by Wiedel and Bondemark (2015), Fernandes et al. (2019), and Staderini et al. (2020) was the relatively shorter usage time demanded by fixed appliances.
In the study by Wiedel and Bondemark (2015), comparing fixed and removable approaches in the treatment of anterior crossbite, the authors found success in both techniques. They stated that most relapses occurred within the first two years after intervention. Evaluating this condition in the aforementioned period and comparing the two groups, the authors concluded that there were small reductions in arch sizes, but without any clinical implication.
Consolidated research such as Tashima et al. (2003) and more recent ones like Fernandes et al. (2019) have also presented the use of an upper removable appliance with digital springs as an early treatment option for anterior crossbite. This approach can be used to move one or more teeth and typically consists of a vestibular or labial arch and digital springs positioned behind the crossed teeth. Originally, removable appliances with digital springs are designed for the upper arch, and it is estimated that the involved teeth will uncross within a period of 6 to 9 months of continuous use.
According to Faltin Jr et al. (2003), cephalometric studies have shown that the therapeutic effectiveness of functional appliances is greater when they are used during the upward portion of the individual pubertal growth spurt. Usually, the effects produced during the peak period demonstrate significant skeletal efficacy, while those used during the pre-peak period show significant effectiveness at the dentoalveolar level.
According to Borges and Almeida (2012), evaluating the pubertal growth spurt can reveal the most favorable phase to start orthopedic/orthodontic treatment, often planned based on the expectation of growth. Typically, the first growth spurt occurs in early childhood, usually at 3 years of age for both sexes. The second occurs in late childhood at around 6 to 7 years for females and 7 to 9 years for males. Finally, the third coincides with puberty, observed from 11 to 12 years in females and 14 to 15 years in males.
Tuma et al. (2011), in assessing the pubertal growth period of 132 schoolchildren aged between 9 and 12 years from the city of Manaus-AM, using hand and wrist radiograph analysis, concluded that female students started the pubertal growth spurt at 10.1 years, with a peak at 11.1 years, while in males, the onset of the spurt occurred at 11.4 years, peaking at 12.3 years.
The timeliness of treatment is important because in the pre-pubertal period, the maxillomandibular growth imbalance is masked by dental compensation, whereas in puberty, there is a sense of worsening due to the exhaustion of its capacity (FREIRE; NASCIMENTO; LIMA, 2011).
According to Giancotti et al. (2003), the Reverse Bionator appliance or Bionator III proved to be a functional alternative for interceptive treatment with clinical effectiveness in correcting Pseudoclass III. Several authors propose different timing approaches for using these appliances, ranging from 15 hours daily, as stated by Giancotti et al. (2003), to 16 hours daily for Silva (2017), 16 to 18 hours daily for Manchini (2020), 20 hours daily for Faltin and Faltin Junior (1998), and a minimum of 22 hours daily for Azamian, A; Shirban (2016) and Wiedel; Bondemark (2015).
An alternative for monitoring the daily appliance usage time is coupling the TheraMon® device, as described by Silva (2017) and Manchini (2020). This is a promising electronic microsensor that encourages the patient to use the appliance.
In the case series reported by Giancotti et al. (2003), the Balters III appliance used on three female patients in mixed dentition demonstrated the following results in cephalometric analysis. Cases one and two showed a maxillomandibular relationship, as indicated by the ANB angle, compatible with a Class I skeletal relationship. On the other hand, the third case had a negative ANB, indicating a possible Class III skeletal relationship. Cases one and three initially presented a tendency for vertical growth, reduced by the decrease in the SNGoGn angle, possibly due to mandibular restraint by the appliance, while the second case showed a balance between vertical and horizontal growth. In all three cases, the lower incisors assumed a more lingually inclined position, allowing correction of the anterior crossbite condition and demonstrating the effectiveness of treatment with the Balters appliance.
Furthermore, according to Giancotti et al. (2003), the vestibularization of the upper incisors and/or lingualization of the lower incisors contributed to the correction of anterior crossbite and elimination of mandibular displacement. The extended use of the appliance aimed to maximize the chances of treatment stability.
The influence of factors such as the patient’s bone maturation, daily usage time, as well as age compatible with the peak of pubertal growth in using the Bionator for correcting anterior crossbite can be explored as a perspective for future research to determine which characteristic is more influential during the treatment period.
4. FINAL CONSIDERATIONS
The modified Balters Bionator appliance for Class III treatment acts to promote correction of dental and skeletal positions, benefiting occlusion and facial aesthetics. It is an approach that can be used in patients of different ages, within growth curves, with good aesthetic alternatives, as it is an intraoral appliance with low potential for causing patient discomfort. The success of the treatment depends on its correct indication and planning, as well as the patient’s adherence to following the recommendations for appliance use and maintenance.
REFERENCES
ALMEIDA, Renato Rodrigues et al. Abordagem terapêutica da mordida cruzada anterior: aparelhos removíveis. Revista Clínica de Ortodontia Dental Press, v. 10, n. 6, pp.48-58, 2011.
ARAUJO, Cristiano Miranda et al. A interceptação da mordida cruzada anterior dentária em forma de tesoura. Da dentição mista até a dentição permanente. Orthodontic Science and Practice. v. 5, n.20, pp. 555-562, 2012.
ARAÚJO, Priscila Pinto Brandão et al. Maloclusão uma questão de saúde pública. IN: DENDASCK, Carla Viana et al. (Orgs). Ciência da Saúde: Atualização de área – janeiro e fevereiro de 2023. 2023. p 53 -63. Disponível em:<https://www.nucleodoconhecimento.com.br/livros/cienciasdasaude/maloclusao#_ftn1>. Acesso em: 6 jun. 2023.
ARAÚJO, Priscila Pinto Brandão et al. Oclusão normal e maloclusão na dentição decídua: um estudo epidemiológico em pré-escolares do município de Belém-PA. In: DUARTE, Vildiane Catique. Prevalência da má oclusão em crianças da educação infantil no município de Belém, Pará. 2018. 28 f. Trabalho de Conclusão de Curso (Graduação) – Faculdade de Odontologia, Instituto de Ciências da Saúde, Universidade Federal do Pará, Belém, 2018. Disponível em: <http://bdm.ufpa.br/jspui/handle/prefix/970>. Acesso em: 10 de junho de 2023.
AZAMIAN, Z.; SHIRBAN, F. Treatment Options for Class III Malocclusion in Growing Patients with Emphasis on Maxillary Protraction. Scientifica, 2016. Disponível em: <https://www.hindawi.com/journals/scientifica/2016/8105163/>. Acesso em: 6 jun. 2023.
BORGES, Rangel Lima; ALMEIDA, Luciano Pacheco de. Estudo comparativo entre dois métodos simplificados de avaliação dos estágios do surto de crescimento da puberdade. Orthodontic Science and Practice, v. 5, n. 20, pp. 505-511, 2012.
BRASIL. Ministério da Saúde. Projeto SB Brasil: pesquisa nacional de saúde bucal. Brasília, DF, 2011.
FALTIN JR, Kurt et al. Long-term effectiveness and treatment timing for Bionator therapy. The Angle Orthodontist, v. 73, n. 3, pp. 221-230, 2003.
FALTIN, Cristina Ortolani; FALTIN JUNIOR, Kurt. Bionator de Balters. Rev. dent. press ortodon. ortop. maxilar, v.3, n.6, pp. 70-95, 1998.
FERNANDES, Natália Lima Freze et al. Mordida cruzada anterior: possibilidades de tratamento na dentição decídua e mista. Revista Naval de Odontologia, v. 46, n. 1, pp. 59-68, 2019.
FREIRE, Marcelo Moraes; NASCIMENTO, Ana Érica Garcia Vale; LIMA, Betânia Pessoa. Padrão Facial III: diagnóstico, tratamento e proservação. Orthodontic Science and Practice, v. 4, n. 16, pp. 849-858, 2011.
GIANCOTTI, Aldo et al. Pseudo-class III malocclusion treatment with Balters’ Bionator. Journal of Orthodontics, v. 30. n. 3, pp. 203-2015, 2003.
GUEDES-PINTO AC. Odontopediatria. 9. ed. São Paulo: Santos, 2016.
KHALAF, Khaled; MANDO, Mahmoud. Removable appliances to correct anterior crossbites in the mixed dentition: a systematic review. Acta Odontologica Scandinavica, v. 78, n. 2, pp. 118-125, 2020.
MANCHINI, Guilherme Biazoto Avaliação do monitoramento do tempo de uso do aparelho ortodôntico removível na clínica de graduação: relato de caso clínico. Universidade Estadual Paulista (Unesp), 2020. 28 f. Trabalho de conclusão de curso (bacharelado – Odontologia) – Universidade Estadual Paulista Júlio Mesquita Filho, Faculdade de Odontologia de Araçatuba, 2020. Disponível em:< https://repositorio.unesp.br/handle/11449/213750>. Acesso em: 11 de junho de 2023.
MOREIRA, Andressa Ferreira et al. Impacto da maloclusão na dentição decídua e permanente na qualidade de vida de crianças e adolescentes: revisão de literatura. Revista Brasileira de Odontologia, v. 72, n. 1/2, pp. 70-75, 2016.
RAMADAN, Letícia Plícila Barbosa Magalhães; JÚNIOR, Milton Santamaria. Tratamento precoce da maloclusão de classe III–revisão de literatura. Journal of Dentistry e Public Health (inactive/archive only), v. 9, n. 3, pp. 220-226, 2018.
SANTOS, Pedro César Fernandes dos et al. Tratamento ortodôntico interceptivo da mordida cruzada anterior: relato de caso clínico. Revista Clínica de Ortodontia Dental Press, v. 11, n. 1, pp. 56-68, 2012.
SILVA, Thiago Amorim. Avaliação Clínica do Monitoramento Digital de Paciente Submetido ao Tratamento Ortopédico Funcional da mandíbula: efeito do tempo de uso: relato de caso clínico. 2017. 29 f. Trabalho de conclusão de curso (bacharelado – Odontologia) – Universidade Estadual Paulista Julio de Mesquita Filho, Faculdade de Odontologia de Araçatuba, 2017. Disponível em:<https://repositorio.unesp.br/handle/11449/156611?locale-attribute=es>. Acesso em: 11 de junho de 2023.
SPILLA, Heloisa Gandolfi et al. 89-Mordida cruzada anterior na dentição decídua. Revista de Odontologia da UNESP, v. 36, n. Especial, 2007.
STADERINI, Edoardo et al. Indicação de alinhadores transparentes no tratamento precoce da mordida cruzada anterior: série de casos. Dental Press Journal of Orthodontics, v. 25, n.4, pp. 33-43, 2020.
TASHIMA, Adriana Yuri et al. Tratamento ortodôntico precoce da mordida cruzada anterior e posterior: relato de caso clínico. J Bras Odontopediatr Odontol Bebê, v. 6, n. 29, pp. 24-31, 2003.
TUMA, Carlos Eduardo da Silva Nossa et al. Avaliação da idade óssea em crianças de 9 a 12 anos de idade na cidade de Manaus-AM. Dental Press Journal of Orthodontics, v. 16, pp. 63-69, 2011.
WIEDEL, Anna-Paulina; BONDEMARK, Lars. Stability of anterior crossbite correction: a randomized controlled trial with a 2-year follow-up. The Angle Orthodontist, v. 85, n. 2, pp. 189-195, 2015.
ZEGAN, Georgeta et al. Risk factors and predictors of crossbite at children. The Medical-Surgical Journal, v. 119, n. 2, pp. 564-571, 2015.
[1] Dental student. ORCID: 0009-0003-8461-6338. Currículo Lattes: http://lattes.cnpq.br/1832010931426679.
[2] Dental student. ORCID: 0009-0001-1734-8455. Currículo Lattes: http://lattes.cnpq.br/8709140095376311.
[3] Dental student. ORCID: 0009-0001-8398-2390. Currículo Lattes: http://lattes.cnpq.br/7301946389987967.
[4] Dental student. ORCID: 0009-0003-0477-2614. Currículo Lattes: http://lattes.cnpq.br/1977203311524825.
[5] Advisor. Updates in Pediatric Dentistry, Training in Laser Therapy, Improvement in Orthodontics and Functional Orthopedics of the Jaws, Specialization in Public Health and Orthodontics, Master’s in Orthodontics, PhD in Orthodontics. ORCID: 0000-0002-5514-0911. Currículo Lattes: http://lattes.cnpq.br/1678395879499706.
[6] Co-advisor. PhD. ORCID: https://orcid.org/0000-0003-4143-289X. Currículo Lattes: http://lattes.cnpq.br/4377698156424992.
Submitted: July 28, 2023.
Approved: August 10, 2023.