CASE REPORT
ALVES, Larissa de Jesus [1], WILLIAMS, Heloise Adele Costa [2], CORDEIRO, Naildo Aguiar [3], PEREIRA, Everaldo de Aquino [4]
ALVES, Larissa de Jesus. Et al. Parendodontic Surgery with Biomaterial Graft and use of platelet-rich fibrin system (PRF): Case report. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year 05, Ed. 04, Vol. 06, pp. 41-60. April 2020. ISSN: 2448-0959, Access link: https://www.nucleodoconhecimento.com.br/dentistry/surgery-parendodontica
SUMMARY
When a patient undergoes dental treatments that do not result in positive effects and as a consequence of these facts starts to run the risk of losing teeth in addition to being affected by other disorders, this patient may be presented with the possibility of undergoing the parendodontic surgery procedure. Endodontics aims to avoid damage to the health of patients who are victims of dental procedures, often caused by the professional’s disability, use of instruments that are inadequate to the procedure, among others. This procedure increases contact with the internal anatomy of the canal, therefore, a procedure widely used when the professional is faced with more conventional treatments that have failed as a result. The objective of this article was to present a clinical case report of parendodontic surgery using biomaterial graft and PRF system, describing the entire procedure used from the consultation to the recovery of the postoperative period of the patient in question, thus seeking to prove the efficacy of this procedure. This is a 20-year-old female patient, presenting an extensive periapical lesion, and a fractured instrument inside the canal, observed and verified by radiographic examination. In this case, the procedure was performed under local infiltrative anesthesia without subjecting the patient to any painful situation. After the entire procedure, the study was concluded and the efficacy of the parendodontic surgical technique associated with the use of a plasma membrane rich in fibrin and bone graft of Bio-Oss material was verified®, evidencing the success of the treatment, preventing the early or dispensable loss of the dental element.
Keywords: Procedures, dentistry, surgery, endodontics.
1. INTRODUCTION
The choice of the theme Paredodontic Surgery with Biomaterial Graft and use of the Platelet-Rich Fibrin System (PRF), is due to the fact that endodontics is an area that studies the dental pulp, root canal system and peripal tissues and also that conventional endodontic treatment has been a pertinent and effective option to prevent early or prescindible loss of the dental element , being indicated in case of irreversible pulpitis, in which the pulp may be in a state that indicates the performance of Biopulpectomy or Necropulpectomy (when there is infection).
You can also make the option for endodontic surgery, according to the need, in cases of: surgical drainage, endodontic treatment, filling without chances of recovery of the canal and its root, material with intraradicular pillar, calcified metamorphosis of the pulp space, iatrogenic errors such as separation of instruments, non-negotiable edge, root perforation, symptomatic overflow, as well as in surgical correction as root resorption defects , root caries, resection, hemisection, bicuspidization, biopsy and exploratory surgery.
The report addressed in this study refers to both a given case of failure, as well as primary treatment and retreatment, which may be a consequence of the patient’s poor health, iatrogenic or complexity of the dental element in question, where endodontic surgery was chosen as a therapeutic alternative for a satisfactory prognosis, considering that this way also ensures the cleaning and complete filling of the canal , adequately removing pathological tissue, contributing to the success of this technique and preventing recurrence of periapic lesions.
This therapeutic choice includes techniques such as perirradicular curettage, apicectomy and retro obturation, although all have a single design, to keep the tooth in the mouth and in function, free of any type of inflammation and infection. However, despite the great validity of conventional endodontics, there is great difficulty in ensuring that all branches of the canal pass through chemical-mechanical preparation and are in direct contact with the obturator material, and with adequate foraminal sealing, preventing the permanence and reproduction of microorganisms. It is from there that parendodontic surgery becomes extremely important, as it can be applied in several cases, being enough to remove foreign body in the root area, inflammations and continuous periapical lesion, loss of obturator material and impossibility of coronary canal treatment.
Parendodontic surgery has been used in order to solve problems in which endodontic treatment is not effective. This technique has achieved success and a greater application by having a knowledge of all anatomical structures involved, resulting in an excellent evolution.
Based on these statements, the main objective of this article is to present a clinical case report of parendodontic surgery that proves the efficacy of the use of biomaterial graft and PRF system.
2. CLINICAL CASE REPORT
2.1 DIAGNOSIS
A 20-year-old female patient attended the Dental Clinic of Nilton Lins University (Manaus–AM) complaining of pain and sensitivity in the region of the upper incisors during food chewing, reporting a history of endodontic and restorative treatment in the region.
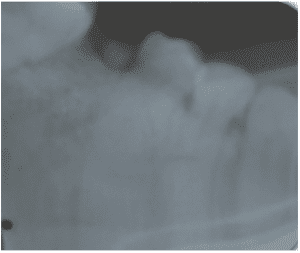
After clinical examination, it was found that the algogen tooth was element 22, where there was an unsatisfactory restoration (Figure 1).
Figure 1 – Initial Clinical Examination

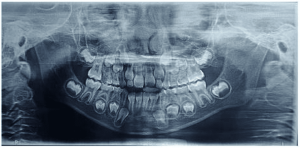
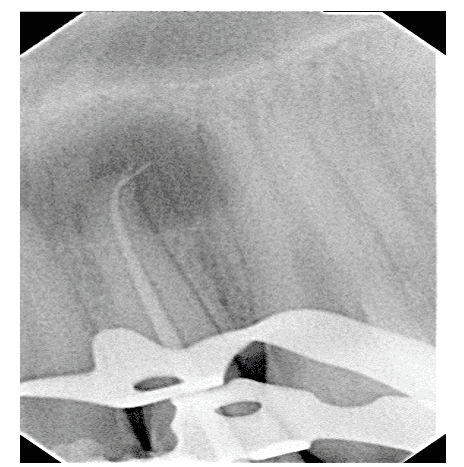
Radiographic examination showed that the tooth did not present endodontic treatment, but rather an extensive apical lesion and fractured instrument at the apex (Figure 2).
Figure 2 – Initial Periapical Radiography

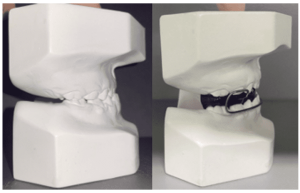
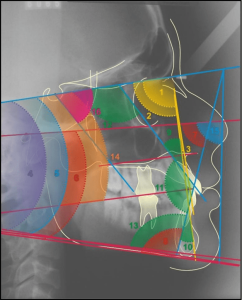
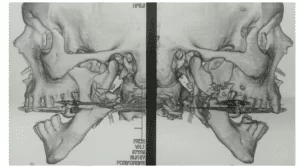
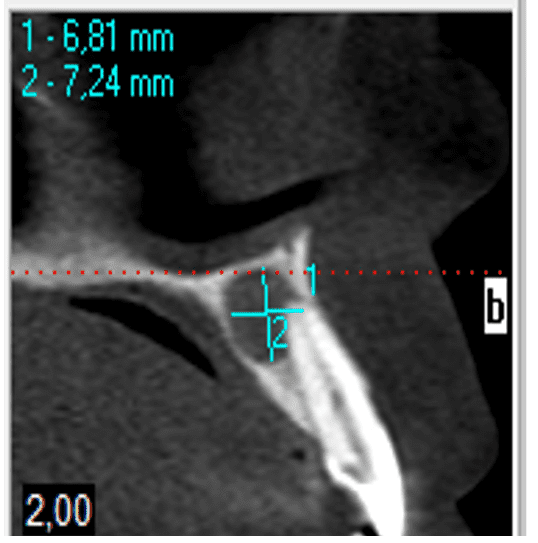
To confirm the diagnosis, a Computed Tomography was requested in order to verify the extent and location of the lesion and closure of the diagnosis (Figure 3 and Figure 4).
Figure 3 – Ct Scan 1
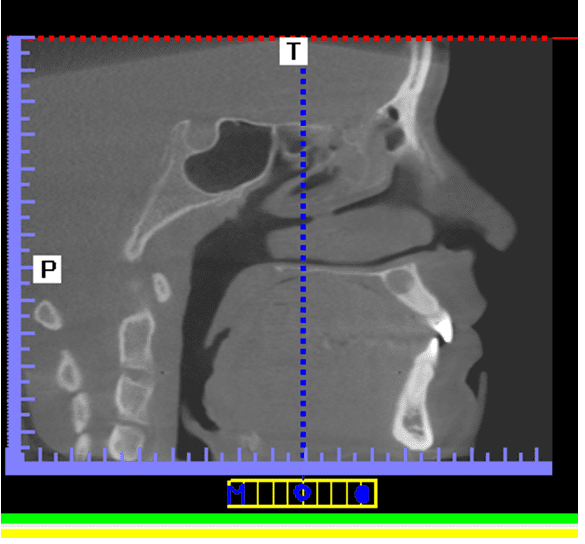
Figure 4 – Computed Tomography 2
2.2 TREATMENT PLAN
For the treatment, we planned to perform endodontic treatment, combined with parendodontic surgery, under the technique associated with fibrin-rich plasma membrane and bone graft with Bio–Oss®.
After discussion and approval of the patient of his treatment plan, the procedures were started.
After prophylaxis, analgesia of the element was performed through anterior upper alveolar nerve block, and field block by the palatine. Absolute tooth isolation 22 was performed conventionally, followed by Access Surgery.
The Reciprocating System (Reciproc, VDW, Germany) with Lima R25 was used as instrumentation. 08, enabling the modeling of root canals with only one instrument.
The actual working length was obtained through the apical locator (Root Zx II, Morita, Japan).
The patient’s odontometry was confirmed in 19 mm. The tooth was instrumented with 5.5% hypochlorite irrigation.
Cone test and radiography were performed for confirmation, immediately after instrumentation, then introduced tetra acetic ethylenediamino acid (EDTA) inside the canal for 3 minutes, shaking it with the file for 1 minute.
The last irrigation of the canal was performed for the removal of the EDTA and then the drying of the root canal.
The tooth was stained with endodontic cement (Endomethasone N, Septodont, Brazil) and sealing with Glass Ionomer Cement (Vidrion R, SS White, Brazil) as temporary restoration (Figure 5).
Figure 5 – Endodontic Treatment Completed
Subsequently, the surgical procedure was initiated, complementing with local infiltrative anesthesia by the vestibular and palatine.
Then, a modified Newman incision was made, promoting a flap from the distal of element 11 to the distal of element 23. Periosteal mucus detachment occurred, allowing curettage and observation of bone injury in this region.
After curettage of the lesion, the #702 drill was used to improve the surgical store. The procedure was constantly irrigated with 0.9% Saline.
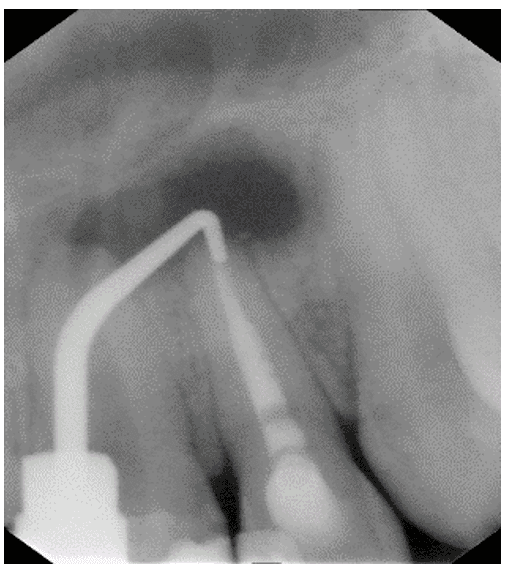
After cleaning the region, tooth 22 was apicectomy, with a cut of approximately 3 mm from the apical portion, with the #Endo Z drill at a 90° angle (Figure 6).
Figure 6 – Tooth Apicectomy 22

Continuing the procedure, 3mm gutta-percha was removed from the apex, leaving it prepared to be filled with white MTA (MTA, Angelus, Brazil), which was inserted and sealed with the aid of condensers (Figure 7 and Figure 8).
Figure 7 – Retro Filling With Mta

Figure 8 – Radiography Of Retro Filling With Mta
The surgical shop was filled with biomaterial Bio-Oss® and the Fibrin-Rich Plasma (PRF) membrane stimulated osteoinduction and osteoconduction (Figure 9 and Figure 10).
Figure 9 – Graft With Bio-Oss®

Figure 10 – Prf System

After filling, excess material was removed and the surgical shop was cleaned (Figure 11) and the flap was repositioned, ending with interdental suture for better adaptation of the edges (Figure 12).
Figure 11 – Immediate Postoperative Radiography

Figure 12 – Nylon Thread Suture 5-O In Immediate Postoperative

2.3 PROSERVATION
Among the postoperative care, the following medications were prescribed: antibiotic Amoxicillin associated with Clavulanic Acid 875 mg (1 tablet every 12 hours for 7 days); anti-inflammatory Ibuprofen 600 mg (1 tablet every 8 hours for 6 days); and, anti-inflammatory Dexamethasone of 4 mg (1 tablet for 3 days).
The patient was instructed to follow liquid/pasty feeding for 10 days, until the date of her return for suture removal and proservation (Figure 13).
Figure 13 – Intraoral Aspect Of Proservation After 10 Days
-ERR:REF-NOT-FOUND–ERR:REF-NOT-FOUND-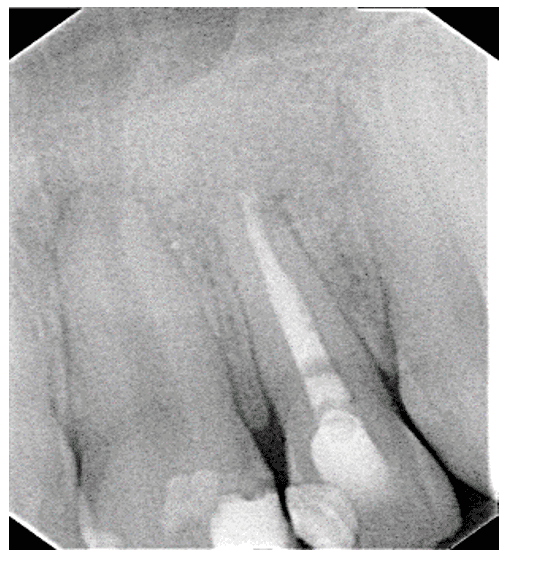
3. Discussion
3.1 ENDODONTICS
Espíndola et al. (2002) they conceptualize Endodontics as the dental specialty that deals with the prevention, diagnosis and treatment of diseases or injuries that affect the dental pulp, the main responsible for tooth development.
For Cohen; Hargreaves (2007), a fairly safe and effective means when it comes to preserving teeth, which by various factors could be lost.
Thus, as comments Gabardo et al. (2009) e Occhi et al. (2011), endodontics has as its primary objective, the maintenance of the dental element as a function in the stomatognathic system, thus avoiding damage to the patient’s health.
3.2 PAREDODONTIC SURGERY
According to Gabardo et al. (2009), it is extremely necessary that scientific and biological principles are maintained to ensure the minimization of failures and accidents, which may also arise from many other factors, such as incorrect diagnosis, professional inability, etc. according to Alvares (1997), such diagnoses may also be consequences of an iatrogenic, which occurs due to non-observance of certain basic care, use of erroneous techniques, such as endodontic file may have been widely used previously and has not been ruled out, or its choice may have been made inadequately.
Apical surgery is indicated, usually in cases of endodontic treatment that have not been successful in tooth repair.
According to Bramante and Berbet apud Cappellari (2015, p.11):
it is up to the professional to know when to indicate periapex surgery. It is of paramount importance to emphasize that the procedure should be indicated only when the other alternatives performed by the conventional method are exhausted. Among the indications, we can highlight the following: anatomical complications, iatrogenic problems, trauma, failures, problems during conventional treatment and need for biopsy.
According to Oliveira; Bernabé (2003) and Holland (2004), parendodontic surgery may also solve many other cases such as persistent periapic lesions, with cystic characteristics and calcified root canals with periapic lesions. In the latter, it is impossible to access through the pulp chamber, fractured instruments, apical perforations and steps.
Bramante, Bramante; Berbert (2000) and Kuga et al. (1992) guide this type of surgery by facilitating instrumentation with the hands, such as files, drills, reamers, etc. of the root canal, as well as to avoid the forced exit of the material used for septicemia, calming pain and other problems, besides having concern with the patient having contraindications for surgery.
Orso and Filho apud Cappellari (2015, p.7), recommend that:
There are different methods for the surgical approach, and it is common for all of them to promote disinfection that was not achieved by the conventional endodontic procedure. They also point out that, regardless of the technique selected, it is extremely valuable to achieve the proposed objective, that is, to obtain tissue regeneration. This is usually achieved by removal of periapical pathological tissue and by excluding any irritant substance.
This type of parendodontic surgery also facilitates, in the case of a filling, by condensing better, without leakage of the material used.
According to what Orso and Filho apud Cappellari treats (2015, p.20):
Periaptic surgery is the most widely used resource when it is not possible to remove the causative agent of apical pathology through conventional endodontic treatment. Any technique used is valid, as long as it achieves the goal of removing the lesion from the apex. For this, we must have a good planning of the surgery and follow the protocol of the surgical technique in order to succeed.
For the surgery of this clinical case report, the radiographic procedure was used to verify the extent of the lesion and what type of treatment would be used.
According to Von Arx apud Cappellari (2015, p. 11), “the goal of periapic surgery is to keep the tooth in the oral cavity, but before surgical practice it is essential to perform a good clinical and radiographic examination in order to evaluate whether or not the surgical procedure should be performed”.
It can be observed the cleaning of the site and then the apicectomy with the drill #ENDO Z before the start of surgery.
To Kuga et al. (1992), the correct tracing of the incision facilitates access to the surgery region.
It was possible to observe a retro filling with the use of white MTA for the sealing of the apex, since it is a material biocompatible with the peripal tissues, and with the ability to regenerate them, if they have been modified by pulp and periapic diseases. This is the most used material in tissue sealing and regeneration.
3.2 BIOMATERIAL GRAFT
The dental bone graft is conceptualized as a surgical procedure whose procedure refers to the removal of a bone fragment from an appropriate site and, consecutively, place it or implant it where it is intended to be repaired. It is also used to reconstruct the area that has lost height or thickness.
About graft, Soares (2015, p.13) comments that:
Graft is a piece of tissue that is transferred from a donor site to a recipient site with the aim of reconstructing the recipient site. This tissue may or may not receive treatment during transfer. It implies the presence of tissue with vitality that was obtained and used at the same surgical time. Example: free gingival graft, connective tissue graft, autogenous particle or block bone graft.
About biomaterial products, Soares (2015, p.11) states that:
In Dentistry, new products are constantly launched in the market. Such products are used in close contact with biological tissues such as pulp, dentin, periodontal tissue and alveolar bone. Thus, biomaterials should be used with caution. Its indication in the various clinical situations should always be well evaluated, taking into account clinical and ethical criteria regarding the risks and benefits of treatment. For this, there is a need for the Dentist to know the characteristics and properties of biomaterials.
On the use of living tissues, Soares (2015, p.11) explains that:
Humanity, since ancient times, has been looking for ways to replace living tissues, either because they are lost or sick, using synthetic or natural substances as substitutes, which, more recently, have been called biomaterials. Biomaterials when used in contact with biological systems whose purpose is to repair or replace tissues, organs or functions of the organism, must have physical and biological properties compatible with the biological tissues of the host, in order to stimulate an adequate response of them.
Second Bernabé; Holland (2004), the use of biomaterials to aid in the promotion of bone regeneration is strongly indicated in large bone destructions surrounding the root apex.
As Soares (2015, p. 13) states, “Biomaterial is any substance or combination of substances, natural or not, other than drugs or drugs, that interact with biological systems, that treat, increase or replace any tissues, organs or functions of the body.”
There is still no general consensus on the use of these biomaterials as an indispensable method in the formation of a new bone and a remodeling remodeling. However, it is agreed with its use in cases of major bone destruction.
Soares (2015, p.11) comments on the need for bone tissue reconstruction, which:
The need for reconstructions of the lost bone tissues led to technical improvement and the advancement of the study of biomaterials that could replace or improve grafting procedures. Bone grafts can be obtained from different origins: autogenous (from the same individual), allogen (from individuals of the same species), xenogen (of different species) or alloplastic (synthetic).
The materials for the graft have the function of acting as a mechanical support structure for the membrane and soft tissues and also act as a biological component improving or recovering bone neoformation.
According to Soares (2015, p.11): “The need for reconstructions of lost bone tissues led to technical improvement and the advancement of the study of biomaterials that could replace or improve grafting procedures”.
Generally, this material can be classified as: osteoconductive, those that provide a frame for bone development; and osteoinductives, which stimulate the proliferation of new cells so that bone healing occurs more quickly. It is up to the professional to discuss its use with the patient, stating that the use of this type of matter entails an additional cost in the surgery, the need for more time for the treatment of the wound and possible complications in the postoperative period.
The Biomaterial used in this procedure was selected according to research in comparison with other types, because it presents excellent osteoconductive properties, conducting bone regeneration in a predictable and efficient way, where particles become an integral part of the newly formed bone structure, allowing an uncomplicated regeneration in the grafted area, besides having as characteristic the long-term volume conservation.
3.3 PLATELET-RICH FIBRIN SYSTEM (PRF)
According to Rodrigues et al. (2015), platelet-rich fibrillams appeared in France specifically for use in oral and maxillofacial surgeries. A technique that does not require anticoagulant or any other gelling agent. It is centrifuged blood without any addition, making it possible to avoid all the restrictions existing in the French law of the time, which had any relation to the reimplanting of a product that was derived from blood.
Fibrin is conceptualized as a protein that, whenever the body has an injury, acts as a first response and whose purpose is blood clotting, that is, an extremely significant and important role.
When blood leakage occurs followed by coagulation, then the body starts the production of fibrin. In the form of long wires, each fibrin molecule interweaves to form a thin mesh around the lesion. The mesh formed by fibrin, which is presented in the form of long intertwined wires, leads to the stagnation of blood. This is because there is a capture of red blood cells, leukocytes and platelets, causing a clot to generate a clot and the appearance at the injured site of a kind of buffer. Thus, with the objective of accelerating regeneration and healing in various surgical procedures, Platelet-Rich Fibrin (PRF) has been used in surgeries in various areas of health such as orthopedic, neurological and plastic surgeries. However, it is usually used in various dental procedures, such as in small bone grafts for dental implants, in periodontal and maxillofacial surgery.
The use of Fibrin Rich Plasma (PRF) in dentistry is very similar to a fibrin dressing and serves to accelerate the healing of the edges of the wound, as it removes the danger of rejection or infection, although this material is removed from the patient himself. This technique is currently much studied due to its efficiency in accelerating tissue regeneration, its integration and remodeling of the biomaterial that has been grafted. It forms a clot that reconstitutes the graft made with the cells, healing very fast.
As Peterson et al. comments. apud Cappellari (2015, p.15-16):
The achievement of the success of periapical surgery depends on some factors. Clinical and radiographic follow-up, as we mentioned, is essential to judge success after endodontic surgery. Generally, the patient is asymptomatic and, in these cases, the evaluation is made only through radiographic findings.
Bramante and Berbet (2000) stressed: “that no parendodontic surgery will result in success if the canal is not well filled or it is not possible, through surgery, to improve its sealing conditions”.
One can sequentially, after a new clinical and radiographic evaluation, organize the cases according to Zuolo and Peterson et al. apud Cappellari (2015, p.16):
-
-
- Success: absence of clinical signs and symptoms. The patient does not report discomfort or any symptomatology and, in radiographic analysis, presents complete repair or scar formation in the surgical region;
- Dubious success/uncertainty of success: the patient does not present clinical signs and symptoms and, in radiographic classification, the repair is uncertain;
- Failure: the patient reports the presence of clinical symptoms and, in the radiographic classification, the repair is unsatisfactory, and may present lucid radio image of the periapex.
-
After the test result, a good prognosis of the surgery was observed, however, it is necessary that the patient be followed for at least 4 years and that the proservation is continuous for at least 1 year.
The radiography and sutures that present are coming from the immediate postoperative period. After 10 days, a new proservation x-ray was performed.
It was observed that parendodontic surgery, although invasive, can be considered as a successful surgical treatment, since it preserves the tooth.
4. FINAL CONSIDERATIONS
After this study, it was concluded that:
- When the surgical maneuver is chosen, it is extremely necessary and essential that the professionals involved are aware of their technique, due to the recommendation of existing clinical protocols, which consist of: deep anesthesia of the operated area, choice of the appropriate flap and curettage of the pathological tissue;
- The indication of the graft with biomaterial as a proposal to assist the healing and regeneration of alveolar bone is totally effective;
- When the association of natural fibrin structures with biomaterial grafting occurs, this material stimulates tissue and bone regeneration, easily evidenced by post-surgical clinical and radiographic examination, the result of which, in this case, presented bone formation and absence of painful symptomatology and also confirmed the preservation of the tooth and its function.
- Clinical and radiographic follow-up is essentially essential and aims to confirm success after surgical intervention involving the aid of the guided tissue regeneration technique.
- Tissue repair may be classified as: complete, incomplete or uncertain. But, commonly, only after one year of the periapex surgical procedure can one notice the definitive repair of the lesion.
- When this procedure is associated with biomaterial biomaterial graft Bio-Oss®, an excellent bone regeneration is observed, due to the similarity with human bone and the use of fibrin-rich plasma membranes from the patient’s own blood, which contributes to the reduction of rejection and contamination.
- From the bibliographical research, it was observed that many authors value its use in cases that present great bone destruction, and also, these same authors claim to present quality and quantity of bone superior to cases without its use.
After the completion of all the procedures described, in the period of proservation, the observed results found that:
- Clinical control was positive and lacked fistula;
- The effectiveness of healing regarding apical curettage concomitant with the use of graft with biomaterial;
- Surgical interventions using membrane-associated grafts can promote bone defect repair to varying degrees.
- An improvement in the repair of the bone defect;
- With radiographic examination, dental resorption, in addition to the improvement of the apical area.
Finally, after all these procedures presented, it was understood that parendodontic surgery was the best therapeutic option chosen in the case described, mainly because it gave access to the apical region of the dental element, providing the removal of the foreign body inside the conduit and periapical lesion, thus proving the efficacy of the method.
5. REFERENCES
ALVARES, S. Resoluções clínicas: procedimentos endodônticos e cirurgico-paraendodôtico. 1. ed. São Paulo: Santos, 1997.
ALVES, L. J.. Cirurgia Paredodôntica com Enxerto de Biomaterial e Utilização do Sistema Fibrina Rica em Plaquetas (PRF): relato de caso. 2020. 19 folhas. Trabalho de Conclusão de Curso (Graduação em Odontologia) – Universidade Nilton Lins, MManaus-AM, 2020.
BERNABÉ, PFE; HOLLAND, R.. Cirurgia paraendodôntica: como praticá-la com embasamento científico. In: Estrela C. Ciência endodôntica. v. 2. São Paulo: Artes Médicas. 2004; 657-797.
BRAMANTE CM, BERBERT A.. Cirurgia paraendodôntica. São Paulo: Santos; 2000.
CAPPELLARI, Tuane. Cirurgia do periápice associada a enxerto com biomaterial – estudo de caso. Santa Cruz do Sul, 2015.
COHEN, S.; HANGREAVES, KM.. Caminhos da Polpa. 9.ed. (Português). Rio de Janeiro: Elsevier Editora Ltda, 2007;1079.
ENXERTO ÓSSEO. In: WIKIPÉDIA, a enciclopédia livre. Flórida: Wikimedia Foundation, 2019. Disponível em: <https://pt.wikipedia.org/w/index.php?title=Enxerto_%C3%B3sseo&oldid=54806516>. Acesso em: 13 abr. 2019.
ESPÍNDOLA, ACS, et al.. Avaliação do grau de sucesso e insucesso no tratamento endodôntico em dentes uni-radiculares. Ver. Gaúcha de Odontol. 2002; 50(3):164-6.
GABARDO, MCL, et al.. Microbiologia do insucesso do tratamento endodôntico. Ver. Gestão & Saúde. 2009; 1(1): 11-17.
KUGA, MC; TANOMARU, Filho M; BRAMANTE, CM; NISHIYAMA, CK.. Cirurgia parendodôntica com obturação simultânea dos canais radiculares. Rev. Assoc. Paul Cir. Dent. 1992; 46:817-20.
OCCHI, IGP, et al.. Avaliação de sucesso e insucesso dos tratamentos endodônticos realizados na clínica odontológica da UNIPAR, UNINGÁ Review. 2011; 8(2):39-46.
OLIVEIRA, MDC.. Remoção de instrumento endodôntico fraturado no interior do canal radicular. Caso clínico. Jornal Brasileiro de Endodontia. 2003;4(14):186-90.
REZENDE, J. M.. Proservação. Publicado no livro Linguagem Médica, 3a. ed., Goiânia, AB Editora e Distribuidora de Livros Ltda., 2004.
RODRIGUES, G.; FABRIS, Vinicius, MALLMANN, Fernando; RECHB, Carlos Alberto; CARVALHO, Rodrigo Varella de; RUSCHELC, George Herbert. Fibrinas ricas em plaquetas, uma alternativa para regeneração tecidual: revisão de literatura. DOI: 10.18256/2238-510X/j.oralinvestigations.v4n2p57-62.
SOARES, Murilo Vila Real. Biomateriais utilizados na prática odontológica: uma revisão de literatura. 2015. 27 folhas. Trabalho de Conclusão de Curso (Graduação em Odontologia) – Universidade Estadual de Londrina, Londrina, 2015.
[1] Academic of the Undergraduate Course in Dentistry, Nilton Lins University, Manaus – AM, Brazil.
[2] Specialization in Endodontics and Prosthesis, Amazonas State University (UEA), Manaus-AM, Brazil.
[3] Endodontics Specialist, Coordinator of dentistry course, Nilton Lins University, Manaus – AM, Brazil.
[4] Master’s degree in Endodontics – Professor of dentistry – Nilton Lins University, Manaus – AM, Brazil.
Sent: April, 2020.
Approved: April, 2020.