RODRIGUES, Rosana do Nascimento [1], FERREIRA, Vanessa Diellen Pinto [2], BITTENCOURT, Margarete Carrera [3], PEIXOTO, Ivonete Vieira Pereira [4]
RODRIGUES, Rosana do Nascimento; et.al. Low intensity Laser therapy on the healing of Pressure sores in a patient from the ICU. Multidisciplinary Core scientific journal of knowledge. 03 year, Ed. 05, vol. 05, pp. 359-418, may 2018. ISSN:2448-0959
Summary
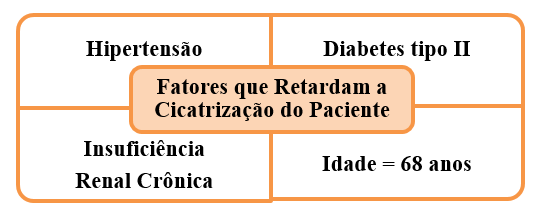
The present study is based on assignments of low intensity laser therapy as an effective option for treating Pressure Sores (LPP), with the purpose of reepithelialization of the injured tissue in shortest time possible. From the whole issue around the patients of intensive care unit (ICU), mainly by acquiring LPPs vulnerability. Having as objectives, evaluate the applicability of low intensity laser therapy (LTBI) Accelerator factor in the healing process of LPPs in stage I and II of a patient from the hospital in ICU and describe the process of tissue repair in LPPs in critical patient treated with conventional therapy dressing plus LTBI. It is a therapeutic intervention study with a qualitative approach, characterized as clinical trial of type case study, involving a 68-year-old patient from the hospital in ICU, showing pressure injuries of grade I and grade II listed, respectively in the regions of the calcaneus and sacral law affecting both buttocks. Data collection was subdivided into two stages, the first materialised for LTBI within hospitals, and the second under house arrest. The instrument used for the present study is the Xt-DMC ® Therapy equipment, which has the function of sending light red or infrared laser of low power (100 mW). The Protocol elected to use was and scan as follows: the irradiation begins the 1 cm from the edges of the wound, making individual applications, leaving between 1 cm and 2 cm between points, using a dose between 2 and 4 J/cm ² associated with a scan , where the applicator is placed 1 cm from the bed of the wound being bustling about the total area of the lesion during irradiation. The results were satisfactory given that there has been a significant improvement in the healing process of the LPPs treated with LTBI adjuvant application showing be a effective therapy as Accelerator factor on healing of a patient from LPPs in hospitalization in INTENSIVE CARE. Demonstrated by the implementation of the outcome of the healing of the wounds of the calcaneus and sacrococcygeal regions, evolving with total reepithelization LPP in 3 sessions of calcaneal LTBI sacrococcygeal region, in the LPP evolved positively showing decrease of the total area in relation to the first session of 15 cm ², being 3.7 cm in width to 53.8 cm tall. Whereas the cellular lesion unprovision homeostasis, body and the patient presents 4 systemic factors that slow down the cascade of physiological events occurring systematically in healing: hypertension; Diabetes; chronic renal failure and 68 years, and the injuries have evolved satisfactorily even with these factors to LTBI is a therapy that needs to be considered in the context of the bandages.
Key words: Pressure injury, intensive care Unit, Software, Laser, Dressings, wound healing.
1. Introduction
1.1 Theme under study
Pressure injuries (LPP) are defined as all integumentary lesion caused by unrelieved pressure and can lead to tissue necrosis. The authors Mathew, et al. (2016) highlight that the regions involved are more frequently the bony prominences, which cause damage to the skin can cause a number of complications like infections, potentializing the aggravation of the condition. The research of Mann; Lee; Jorge (2009) has shown that the number of cases of LPPs worldwide remain high, what comes to the meeting of what is being discussed in the literature, which emphasize the need for new studies on the subject, in order to improve preventive measures and therapies.
Nursing is a profession that acts in complex care and immediate decisions in all sectors of assistance in health care, especially when working in the intensive care unit (ICU). The studies of their respective authors, Zanei Ducci, Whitaker (2008) highlight that the ICU is a sector of extreme complexity, where we found bed ridden, having any difficulty or constraint to move in bed, what makes these patients susceptible to potential risks of complications due to invasive procedures, loss of muscle mass and the occurrence of LPPs.
With regard to the care of patients with tegumentary commitment, the nurse is the healthcare professional that has a key role in the treatment of wounds, since this professional has more contact with the patient, follows the evolution of injury, orients and executes the dressing, as well as holds greater mastery of this technique by virtue of owning curricular components geared to this practice and nursing team develop it as one of your assignments.
Currently, there are many choices of dressings on the market. The authors franc Gonçalves (2009) point out that the financial resources of the patient and/or health unit to the need for continued use of the dressing, wound assessment, and the evaluation of benefits and costs, are some of the aspects to be considered at the time of choosing the type of dressing, which must be appropriate to the nature, the location and the size of the wound to facilitate the healing process.
The healing process is understood as a collection of complex, interdependent processes, whose purpose is to restore damaged tissues. Corroborating with this described, the Mandelbaum study; Di Santin; Mandelbaum (2003, p. 393) States that "the study of skin repair involves a huge range of events and special situations and that requires basic knowledge of Anatomy, histology, biochemistry, immunology, pharmacology, among other sciences".
The use of low-level laser on skin wounds Treaty contributes to the optimization of the process of healing with your action shot stimulating. Is in line with these reflections the authors Andrade; Clak; Ferreira (2014), when they emphasize the low intensity laser therapy, applied on skin wounds, is able to promote the main physiological effects: anti-inflammatory response; neo-angiogênese; epithelial and fibroblast proliferation; synthesis and provision of collagen and wound contraction.
The present study is based on powers of laser therapy as an effective option for the treatment of LPPs, with the purpose of reepithelialization of the injured tissue in shortest time possible. The authors ' Rock studies, et al. (2012) highlight that the laser effects are assigned to stimuli of various biological systems when photo stimulated by radiation, proving to be an effective review, because it decreases the time of tissue replacement with increased proliferation and cellular activity , modulation and proliferation of growth factors.
1.2 Background
Patients admitted to Icus feature the profile of potentially severe State and require a more advanced support with multiple parameters monitoring and surveillance in period, where an intensive level assistance would be the only solution for evolve satisfactorily. On this, it is considered that the same report physiological conditions unfavorable for homeostasis and body performance of multidisciplinary team is essential to optimize the development of improvement.
In this context, the nursing care stand out as transaxle that pervade the health care process, providing better conditions for the patient, both in the performance of procedures and actions directed to prevent possible acometimentos from a prolonged hospitalization. Support with these reflections the authors Miyazaki; Caliri and Santos (2010), when they emphasize that patients admitted to Icus have a greater susceptibility to complications, jeopardizing your safety, such as hospital-acquired infections, errors related to medication administration process and the lesions skin integrity among others.
This study becomes relevant because of the high rate of LPPs in UTIs, that are directly related to the patient's physiological impairment. In our academic experience enjoy the discipline entitled Hospital Nursing care Practice, in which we had the opportunity to perform dressing of small, medium and high complexity and observe how this practice is present in the routine of nursing. Starting from this point of view, the theme sparked us exploring a methodology which provides a considerable improvement in the LPPs, prevenisse the evolution of the stage of damage and that optimizes the work routine.
From these assertions, we highlight the merits of using the technology of low-intensity laser in the treatment of skin wounds, based on the authors Andrade; Lima and Albuquerque (2010), which emphasise that lllt bioestimulantes effects on wound, because the responses of cells to the infrared radiation occur due to physical and chemical changes of photoreceptors that, to absorb the light, take electronic excited state, that gun clicks four primary actions: change the State of reduction and oxidation (redox State) and acceleration of electron transfer; structural changes and biochemical activity by the transitional heating of chromophores (atoms responsible for the coloration of a molecule); increased production of superoxide; generation of molecular oxygen, contributing to the healing process.
Therefore, the interest in the topic proposed in this study part of the consideration of the whole issue around the ICU patients, mainly by acquiring LPPs vulnerability, through the lack of mobility and how these injuries can cause damage irreversible physical integrity. Such claims come against what we want in order to add up with this point of view the authors point out that.
Among the risk factors that contribute to the exposure of patients to your development: mobility deficit or sensitivity, friction and shear, edema, humidity, old age, systemic diseases, use of some medications such as example, corticosteroid, anti-inflammatory drugs and antibiotics, nutritional deficiency, neurological impairment and metabolic disorders (BAVARESCO; LEROUX, p. 3, 2012).
We highlight the importance of this study from the moment the authors set out to show data that are the quality of the use of laser in tissue repair in ICU patients affected by LPPs and contribution in the feeling of taking the technological development on assistance, since there are types of injuries that need healing stimuli, that is, technologies that provide cooperative aid in biological healing steps. Without these external stimuli, the wound remains longer in the inflammatory stage and consequently exposed to infectious agents and possible infections.
1.3 Questioning
In Brazil, the studies have evaluated the incidence and prevalence of LPP both in hospitals and in the long-stay institutions and households, revealing that the numbers vary according to the scenario and the profile of the patients studied. Consistent with these assertions the authors Oliveira, et al. (2013), where Excel in their studies that, in the context of intensive therapy, the occurrence of LPPs can present themselves with higher numbers due to the severity of patients, frequent therapy procedures, use of vasoactive drugs, immobility in bed, device-specific connection and long periods of hospitalization.
Specific care to the LPPs involves the entire multidisciplinary team, so that the therapeutic actions can be integrated. It is considered a disturbing factor to changes of stage/degree of the LPPs, possible infections and consequently the worsening of the clinical condition of the patient. Considering the importance of the contribution of scientific knowledge of the multidisciplinary team, especially the nursing staff in order to prevent and treat the LPP.
It is known that in Icu beds are admitted patients that need specialized attention, monitoring among other items assists for a full-time and often aren't decubitus changes priorities. One can infer the study of the authors Pereira and Soares (2012, p. 140), say that "effectively, the existence of a pressure ulcer is a complicated process, marked by pain, discomfort with physical, psychological and emotional impact for the patient and to their loved ones ".
The nurse, in this context, to overlook the change in decubitus and patient assessment, can become possible LPPs Stimulator or encourage negative developments of these lesions by demand from patients to be cared for. It is worth mentioning that the working day stipulated by the resolution of the Collegiate Board (DRC) paragraph 26 of 2012, where States in personal sizing the amount at least 1 nurse for every 10 beds, do not match the reality.
Thus, it is considered relevant to invest in preventive and therapeutic proposals related to the confrontation of this problem. Several factors interfere with the healing process and today the market offers a variety of products that can be used with success both in prevention and in treatment of LPP.
The laser therapeutic instrument for incorporation as has been accompanied in the biomedical area since 1960, by Theodore Maiman. Since then, the low-intensity laser has a number of indications, which may be used alone or as an adjunct to other treatments. The laser treatment is painless and local, the duration and number of sessions will depend on each clinical picture, the laser operates in the healing and regeneration of all the different tissues of the human body.
The treatment of wounds, through low intensity Laser therapy (LTBI), active physiological effects contributing to the healing process, from this perspective the authors Busnardo and Simões (2010) point out in their studies that photic stimulation, In addition to providing anti-inflammatory and analgesic effects, also positively influence the function of macrophages, enabling the production of growth factors that favor for the increase of cell proliferation, improving the quality of wound healing .
In this perspective, the effective LTBI to accelerate the healing process of these injuries?
2. Goals
2.1 General
Assess the applicability of low intensity laser therapy (LTBI) Accelerator factor in the healing process of LPPs in stage I and II of a patient from the hospital in ICU.
2.2 Specific
- Perform LTBI in the lesions;
- Describe the process of tissue repair in LPPs critical patient treated with conventional therapy dressing plus LTBI.
3. Conceptual bases
3.1 Anatomy and physiology of the skin
The integumentary system performs functions related to your location on the surface of the body. The skin protects against injuries and also receptors for sensations of pain, pressure, touch and temperature. The Red author (2014) highlights, in his studies, that the skin has several functions, such as: mechanical protection; microbiological and our body's physiological; It is also responsible for the production of vitamin D.
The skin is considered the largest organ in the human body and represents about 15% of body weight, with structural changes over the course of your extension. According to the studies of camera (2009), the skin is made up of three interdependent layers: the outer layer, the epidermis; intermediate layer, the DermIS; and the internal hypodermis layer or layer of adipose tissue, on which lie the layers already mentioned, allowing the skin to move freely about the deeper structures of the body.
The epidermis is composed of stratified pavimentoso keratinized epithelium. "The most abundant cells in this epithelium are the keratinocytes. The epidermis presents three types of cells: melanocytes, Langherans cells and merkel "(JUNQUEIRA; RAM, 2009, p. 360).
In this perspective, the author elucidates Garbero (2016), in his studies, the DermIS is a thick layer of connective tissue that settles the epidermis and proceeds, in depth, with the subcutaneous tissue lipid Rico, consisting of two layers. The thinner papillary, formed of loose connective tissue with large amount of cells and a loose of slender nonlipid Collagen fibers (mainly collagen type III). The lattice is denser, with thick Collagen fibers (mainly collagen type I) arranged in large bundles. In addition to Collagen fibers, the DermIS contains abundant elastic fibers that form a nonlipid between the beams and the collagen. The cells which are found in greater quantity are fibroblasts and macrophages, but there is also a good amount of mast cells.
The hypodermis is made up of connective tissue called adipose panniculus lumpy, richly served by blood vessels and nerves. Leonardi (2008) explains that the formation of skin blood supply consists of arterial vessels, deleting it and forming two plexuses: one that is located on the boundary between the DermIS and hypodermis, and another between the reticular and papillary layer. The papillary layer is starting fine branches of the dermal papillae and each papilla has a single handle with a vascular arterial branch ascending and a descending line.
3.2 physiology of wound healing
The healing process aims to re-establish the integrity of the skin. The authors fields; White and Groth (2007, p. 51) state that "the healing of wounds is in perfect and coordinated cascade of cellular, molecular and biochemical events that interact for tissue reconstruction." This process is triggered by any tissue damage, some authors classify the physiology of wound healing in three stages: inflammatory, proliferative and remodeling (maturation).
Consistent with these reflections the authors Isaac, et al. (2010), when he explains the cellular level phases of the healing process, emphasizing that the first is characterized by the hemostasis, resulting from the formation of fibrin clot, and migration of Phagocytic leukocytes, which will remove the substances strange and microorganisms. The second involves, primarily, the migration and proliferation of three classes: fibroblasts, endothelium and keratinocytes, in addition to fibronectin deposition on the carcase of fibrin, forming the fibronexus; the secretion of collagen III, in your most, about the latter and synthesis of other matrix elements, being the most responsible fibroblasts by these structural changes.
In the third and final phase, change occurs on collagen organization pattern and your main type occurring collagen III replacement by I, increase in the number of cross-links between the monomers of this substance and orientation prevalent in the lines of skin stress, phenomena that increase resistance of the wound. All the healing process will be controlled by polipeptídios called growth factors, which will modify the physiology of their target cells.
With respect to classification as to the type of healing, may refer the authors Santos, et al. (2005), in order to show that the first intention healing wounds there is no loss of tissues and the edges of the skin are juxtaposed, healing wounds by second intention are presented with considerable loss of fabric, the edges the skin are far away from each other and healing is slower when linked with the first intention. Healing wounds by third intent are those that are surgically corrected after the formation of granulation tissue, in order to present best functional and esthetic results.
3.3 cellular Injury of skin
All forms of tissue injury starting with molecular changes in the cells, which are in a State of homeostatic balance, able to handle the physiological demands. Pathogenic stimuli and stress can lead to cell adaptation, situations that result in structural changes, but with preservation of cell viability. "If these stimuli are more aggressive, to the point of exceeding the capacity of adaptation, which had resulted in a sequence of events that will culminate the cellular injury" (SILVA et al.., 2011. p. 63).
Biologically it is known that neo-angiogênese is the development of new blood vessels, namely, the formation of a new blood supply, this procedure is necessary to provide an ideal environment for healing of the wound. In this context, we stress the Tazima studies; Vicente; Moriya (2008, p. 259), where they emphasize that "in all the wounds, the blood supply of the fibroblasts are responsible for the synthesis of collagen that stems from an intense growth of new vessels, featuring healing by second intention and the fabric of granulation ". The new vessels are formed from the solid, which migrate endothelial shoots towards the periphery to the center of the wound on the fibrin mesh placed in the bed of the wound.
3.4 pressure injuries and ratings
According to the studies of Wada, et al. (2010), LPPs occur when the interstitial pressure exceeds the pressure intracapilar, resulting in a deficiency of capillary perfusion, which prevents the transport of nutrients to the tissue by intrinsic and extrinsic factors to the patient. The study authors Mathew, et al. (2016) clarify that the primary pathophysiological development factor of these lesions is the pressure caused by the weight of the body through the lack of mobility, which is the condition that Icu patients are contributing significantly to the development of the disease, when the soft tissue of the body is compressed between a bone and a hard surface overhang causes a pressure greater than the capillary pressure, ischemia occurring at the site of compression. Nursing Protocol for the prevention and treatment of pressure ulcers of the State Institute of Hematology of Rio de Janeiro (2010) sorts them into stages: stage I II, II and IV.
In stage I, the skin remains intact, showing hyperemia of a localized area. The hyperemia doesn't regress after pressure relief, there are discrete edema. At this stage of LPP, the spontaneous healing if preventive actions are carried out, such as change of decubitus, patient positioning etc.
In stage II, there is loss of the integrity of the epidermis, with commitment of the dermis. Superficial injury with pale red bed, without esfacelo (devitalized tissue). Can still get introduced as bubble intact (serous exudate), or broken open.
Stage III presents its commitment to the subcutaneous tissue, which is visible without bone exposure, tendon or muscle. There may be esfacelo, including detachment of the skin and tuneilização (formation of tunnels related to depth).
When the lesion reaches the stage IV, there's commitment to total loss of tissue, with muscle or tendon. There may be esfacelo or eschar (dead tissue of black colour with dry texture similar to leather). This type of wound often includes detachments and tuneilização. Can affect muscles and supporting structures as fascia, tendon or joint capsule, leading to the appearance of an osteomyelitis.
3.5 pressure injury in intensive care unit
We can understand, based on the Nursing Protocol for the prevention and treatment of Pressure Ulcers (2010), that mainly affect LPPs bedridden patients and with movement limitation, in this context it is considered that the ICU patients are vulnerable to these injuries, which can cause untold damage in terms of pain and suffering, in addition to contributing to the rising costs with hospitalizations and treatments. The existence of a FUND in the period of hospitalization disrupts the body Physiology in your chemistry and your emotion, especially by the condition of impairment of physical integrity, which imposes the patient a new image and the multidisciplinary team develop a set of strategies for the prevention and recovery of injured tissue.
From this reflection, we can say that the quick guide of Pressure Ulcers, built by two nurses, Thuler and Dan (2013), Excel in their studies that people with decreased sensitivity, prolonged immobility, or jumble with old age are more susceptible to acquisition of LPP, whereas the locations most at risk of the LPP are the Chin area, occipital regions, shoulder, elbow, sacral, ischium, trocante, iliac Crest, knee, and calcaneus malleolus. The authors also argue that, despite scientific and technological advances for the prevention and treatment of the LPP, this complication is still an important cause of morbidity in hospitals, institutions of long permanence and in home care the susceptible.
The LPP is difficult to treat, generally extended and costly, which confirms the premise of prevention. "So, before people presenting risks to the development of pressure ulcers, the multidisciplinary team responsible for implementing preventive measures, in order to reduce the impact of this interlocutory appeal (GOMES, et al., 2011).
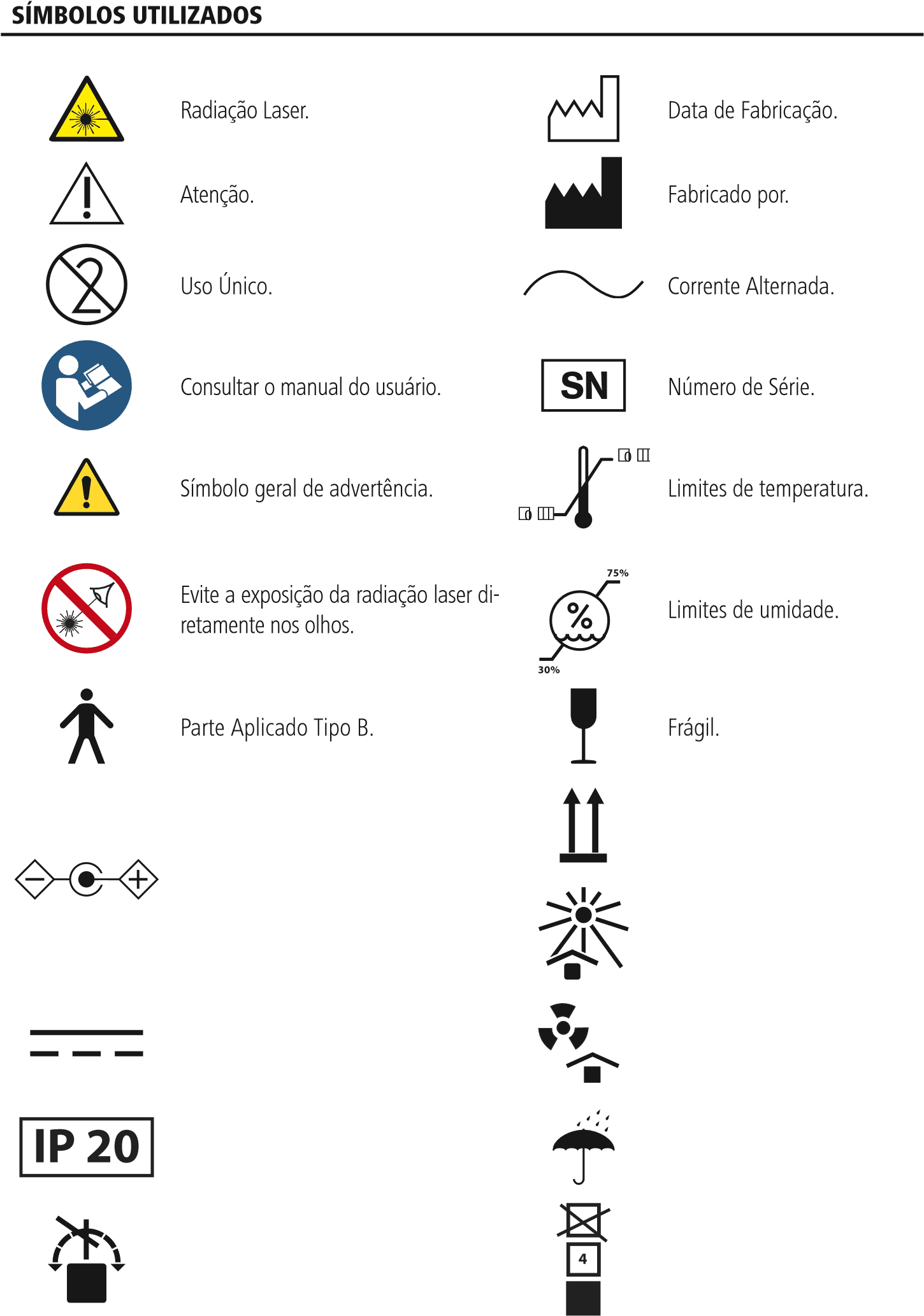
3.6 evaluation of pressure injury
There are several scales for evaluation of an LPP, among them the Braden Scale, which was developed based on the pathophysiology of the LPPs, using three determinants considered critics: intensity; duration and pressure, and tissue tolerance. The authors Barbosa, Becaria and Poletti (2014) stand out, in his study of risk evaluation of formation of LPP, the scale is made up of six sub scales as shown in figure below. The total scores range from six to twenty-three, with the highest values indicate a low risk of LPP and low scores indicate a high risk for the occurrence of these lesions.
We can infer, with authors Garcia, et al. (2011), that patients undergoing intensive care, i.e. admitted to Icus, present high risk to develop LPP, due to environmental restrictions and psicobiológicas, such as: hemodynamic instability, restriction of movement by period extended time and use of sedative and analgesic drugs, which decrease the sensory perception and hinder mobility. These patients represent a priority group for the study and identification of occurrence of such LPPs. It is important to note that currently the best known are the scales of Norton, Gosnell, Waterlow and Braden. The latter, of American origin, created in 1987, passed through validation and adaptation to the Portuguese language.
3.7 the use of laser in treatment of skin lesions
As the studies of Torres and Basha (2007), the term laser is an acronym for Light Amplification by Stimulated Emission of Radiation, which stands for light amplification by stimulated emission of radiation. Although it was Albert Einstein who devised the principles of generation of this type of light, only in 1960 was produced the first laser emitter. The low intensity laser therapy entered the arsenal of modern medicine as an effective component to aid in the treatment of a large number of diseases.
Since then, several surveys have been conducted on animals and humans to test the risks and benefits associated with LTBI, but most information obtained are still discordant. Second Kitchen (2003), the first treatments of low-intensity laser lesions in humans were made during the late 1960 's and early 1970 through the Group of professor Endre Mester in Budapest, the results of this work indicated the potential of laser irradiation of relatively low intensity were used No sources and doses of up to 4 J/cm ², obtaining success on these results in terms of faster speeds for wound healing and pain reduction.
Baxter (1998) points out that in the following decades, lllt has been evaluated in the treatment of various types of wounds and injuries by pressure, with positive results, especially in chronic and intractable cases. The aim in this type of treatment is to accelerate the process of margilinização, increase the blood flow in the area of the wound, as well as stimulate angiogenesis. Second Kitchen (2003), some authors standardize the energy density or irradiance to be deposited on the site to be treated must be between 1 to 6 J/cm ². These recommend the following treatment: anti-inflammatory-1 to 3 J/cm ²; circulatory action-1a 3 J/cm ²; action antiálgica-2 the 4 J/cm ²; regenerative action-3 to 6 J/cm ².
Bagnato (2005) States that the basic principle of operation of the laser is in the fundamental laws of the interaction of the light radiation with matter. So, the factor that determines what kind of matter and with what aim the laser is used, and your intensity. Authors (Baptista, 2003; Columbus, et al., 2013) highlight that the low-level Laser (LBI) or therapeutic, comprises a power of up to 1Watt (W) or 0.001 milliwatts (mW), being a radiation (optical), makes up part of the electromagnetic spectrum using a track between 600nm to 1000nm ( nanometers), i.e. visible light (red) and invisible (part of the near infrared and ultraviolet) (Annex B).
The COFEN Resolution 358/2009 on the Systematization of nursing care and the implementation of the nursing process in public and private environments, in which occurs the professional nursing care and other matters. The Regional Council of nursing care (COFEN), regarding their assignments, releases the use of LTBI by nurses, provided that they are properly trained and specialized for the use of the same (Annex D).
In the treatment of wounds, the nurse working in evaluation, choice and determination of conduct, as a fundamental factor for effectiveness of treatment because the improper choice will cause complications and delay the healing process (Macintosh; Kakihara, 2011). Nurse trained and specialized in procedures with laser therapy can use it for healing care, muscle relaxation, reduction of edema and pain relief (COFEN, 2011; COREN, 2014).
Considering the above, it is concluded that the conduct of the procedure with LTBI may be performed by the nurse, in the context of a multidisciplinary approach, since qualified in specific courses, recognized and regulated institutions. The use of LTBI aims to tissue repair as adjunctive therapy in the treatment of acute and chronic wounds in bone and soft tissues and the prevention of complications from inflammatory changes or inhibition of acute and chronic painful processes. Please find attached the opinion of the COFEN and COREN (Annex C).
4. Methodology
4.1 type of study
It is a therapeutic intervention study with a qualitative approach, characterized as clinical trial of type case study, involving a 68-year-old patient from the hospital in ICU, showing pressure injuries of grade I and grade II listed, respectively in the regions of the calcaneus and sacral law affecting both buttocks.
It is considered a clinical trial types of nature controlled research that evaluates over time human beings subjected to interventions targeting health outcomes, and the intervention of medical surgical, mental, nature, through equipment, or educational guidance. "Clinical trials are associated with medical research; the evaluation research; with the fields of education, social service and public policies; and the nurses were developing your own tradition on "intervention research (POLIT; BECK, p. 321, 2011).
From a qualitative approach, the author Creswell (2010, p. 43) defines it as "a way to explore and understand the meaning that individuals or groups ascribe to a social problem or human". The main qualitative procedures, according to Creswell, focus on intentional sampling, open data collection, analysis of texts or images and personal interpretation of the findings.
4.2 research site
The present study was initiated at the Hospital de Clinicas Gaspar Viana (FHCGV) in the period from 15 March-08 April 2017. 2 LTBI sessions were held under the hospital the patient subsequently was discharged and we continue with the sessions under house arrest.
4.3 research Participant
Participated in the present study a 68-year-old patient from the ICU of the FHCGV, featuring LPPs of stage I and II without signs of infection on injury.
4.4 criteria for inclusion
Patient hospitalized from the ICU, showing LPPs of stage I and II, regardless of size, location and number of lesions.
4.5 exclusion criteria
Patients with infected LPPs and in stage III. It is known that the use of laser brings many benefits, but has its contraindications that must be respected in order to avoid a further secondary. In this perspective the studies the authors Moshkovska and Mayberry (2005) and Bjordal (2005) point out that the exclusion criteria for the use of laser is established by clinical presentation of the following items:
Photosensitivity or hypersensitivity caused by laser radiation, and can generate an allergic process and consequently develop a means of contact for colonizing microorganisms; thyroid gland, hormonal changes may occur; gravid abdomen, because the transplacentário contact may occur changes and poor fetal formations; Infected, because the LPPs LTBI with your action fotoestimulante also stimulates the proliferation of bacteria when colonized; lesions of malignant origin, since the use of laser stimulates the activation of intracellular energy capacity by stimulating the proliferation of cells; injuries close to natural holes for the risk of obstruction, burns and infection, since it is a medium where the microbiota in homeostasis is constituted by bacteria resident; LPPs located around synthetic material exposed (metal plates and screws) risks of burns.
4.6 data collection
Data collection was subdivided into two stages, the first materialised for LTBI within hospitals, and the second under house arrest. It is relevant to highlight the interpersonal relationships between patient and family, who were instrumental in brokering the final result positively.
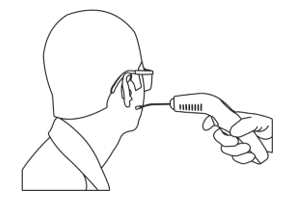
Their procedures were performed: reading of informed consent (TFCC), which is found in Appendix D; term of authorization for use of images (Appendix E), for documentation and photo exhibition on research and explanations related to inclusion and exclusion criteria of the study, as well as the risks and benefits of using of LTBI treatment of LPP; clinical examination of the LPP for evaluation, approached characteristics of injuries, such as the size, type of fabric, peri-ulceral, swelling, pain and redness; cleaning of the lesion with jets of saline 0.9%, followed by the drying process using sterile gauze, subsequently using the laser.
The methodology of radiation chosen was punctuated, where the pen is positioned perpendicularly to 1 cm from the edge peri-ulceral. 15 LTBI sessions were held on alternate days during the period of 30 days; Essential Fatty Acids was used (ACTS) as topical coverage, promoting hydration of the wound bed; There was the realization of the occlusion of the lesion using sterile gauzes and micropore and/or tape. The Protocol elected to use was the author Kitchen (2003), which associates the scoring technique with scan and determines the treatment as follows: the irradiation begins the 1 cm from the edges of the wound, making individual applications, leaving between 1 cm and 2 cm between points using a dose between 2 and 4 J/cm ² associated with a no contact (scan), where the applicator is placed 1 cm from the bed of the wound being bustling about the total area of the lesion during irradiation.
We elect this Protocol through various studies in the field of physics and biochemistry, the goal of this method is to speed up the process of marginalisation, increase the blood flow in the area of the wound, stimulating angiogenesis, increasing the potential for cellular healing energy of the radiation.
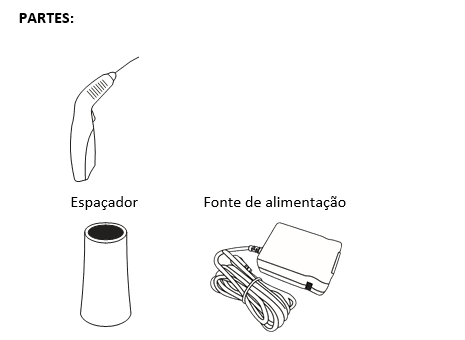
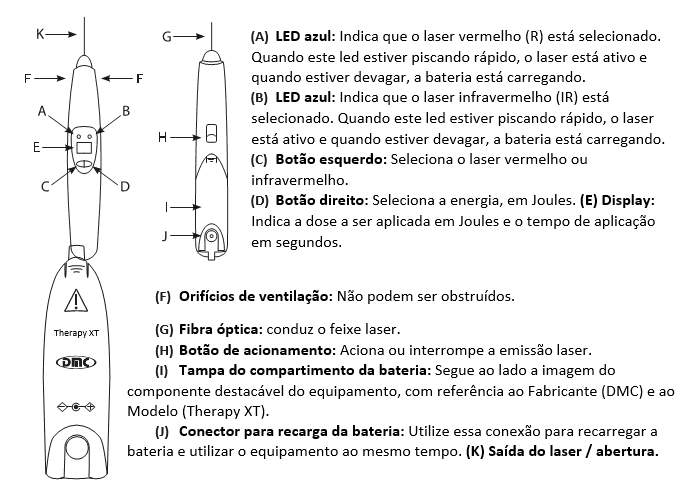
4.7 research Instrument
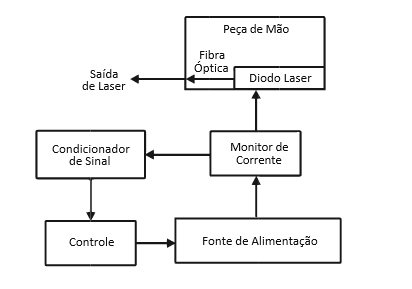
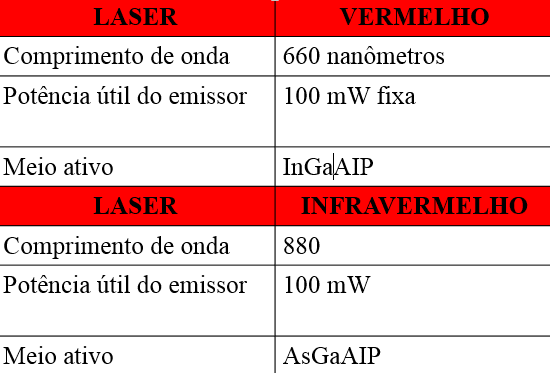
The instrument used for the present study is the Therapy equipment Xt, which has the function of sending light red or infrared laser of low power (100 mW) for application of laser stimulating collagen synthesis and healing of soft tissue ( epidermis, DermIS and hypodermis). With analgesic and anti-inflammatory action, increase the local blood supply, aiding the formation of granulation tissue.
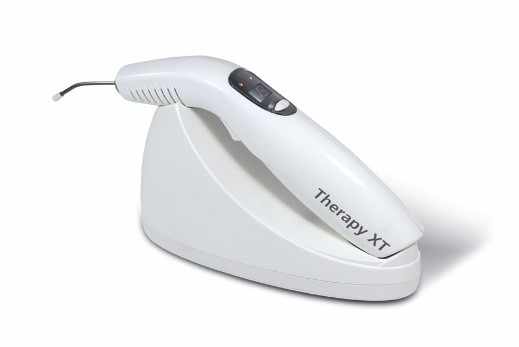
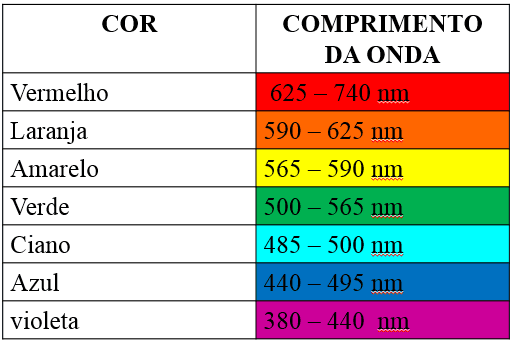
We highlight some functions that are related to the choice of the type of wave and the Joule power used on local application of the fabric. The study of author Colls (1986), held in Barcelona in Laser documentation centre, referred to the relationship between wavelength and cellular action potential, emphasizing that the methodology used in the infrared band stimulates fotofísicos and effects on photoelectric cell membranes. As a result, promotes excitation of electrons, vibration and rotation of molecules, which result in increasing the synthesis of ATP. It is well-known that the laser wavelength depends on the type of component that emits light, led by the optical system and the way to energize you, the light emitted is always monochrome, i.e. a specific element. As shown in figure below.
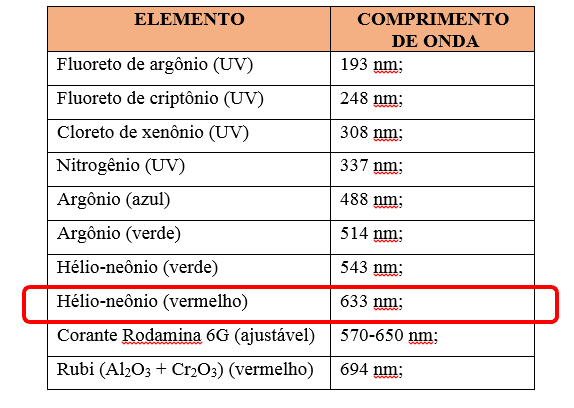
Based on studies of the authors Meirelhes, et al. (2014), the lasers that feature power until 1watt when used at length in red band as shown in the figure 4, include in your action mechanism of the photochemical reactions mediated induction by direct activation of enzyme synthesis, its primary targets are the mitochondria and lysosomes.
The light emitted by the laser medium is of waves that have a specific length, the author Péroca (1999), in a publication entitled Understanding the physics of Laser, highlights that the wave length corresponds to the distance between two Maxima and two minimal, where the same is measured in the direction the wave is moving. The frequency is given by the equation F = C/L, where F is the frequency, C is the speed and L is the wavelength. It should be noted that the frequency is the number of waves that pass a given point during the time of a second.
The equipment used to mediate the patient referred to the LPPs LTBI features ability to emit lasers with their respective characteristics, however it stands out that the wavelength used to perform LTBI was 660 nanometers. Shown in the image below.
Joule is the International System (SI) unit for energy and Watt is the SI unit of power. These units refer to different magnitudes and the relationship between these variables is measured by mathematical calculation that can be realized from two formulas. As image B.
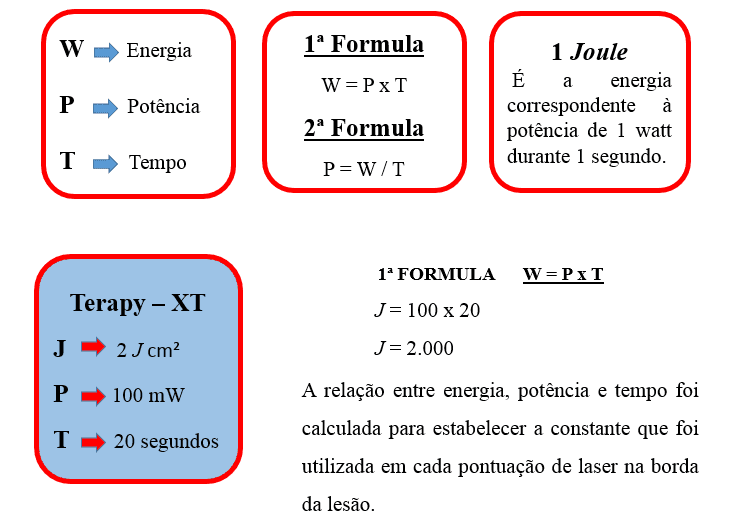
The application of 2 Joules with the power of 100 mW in the time of 20 seconds per score, i.e. each score in peri-ulceral region corresponds to these three constants: J = 2, P = 100 mW and T = 20 seconds. In addition to the scanning method with the same constants, but with different power distribution.
The authors Brugnera Junior and Patel (1998) describe the absorption of energy by means of laser and interface cell, occurs when a stable atomic structure reacts with a photon passing a State more energized. The use of LTBI, this reaction takes place in a manner deliberately after each session, since the steady state corresponding to the minimum level of energy and to receive more energy passes to the excited state.
4.8 Data Analysis
The technique chosen for use in this study was a type of digital analysis through an application titled Mobile Wound Analyser (MOWA). This tool is little used in Brazil and is routine LPPs assessment in hospitals in North America and Europe. It is a mobile software solution for the management of LPP, being an application for smartphones and tablets, which uses color classification to evaluate tissue type; the dimensions of the lesions are made in the form of anatomical plan measurement (height, length, depth and type of fabric) with digital photography. It is relevant to note that the application does not perform the reading of epithelial tissue, or reepitelizado, i.e., it is calculated the total area of the lesion and from this parameter, is the percentage of each type of tissue present.
According to the guidelines of treatment of injuries under pressure from the European Pressure Ulcer Advisory Panel (EPUAP) and National Pressure Ulcer Advisory Panel (NPUAP), monitoring methods of wounds should be considered the photographic documentation and the use of electronic devices for data collection.
For the verification of the patterns of healing of injuries, especially with regard to the decrease in ulcer area over the period stipulated, the accompaniment was with fortnightly evaluation of tissue types that exist in the bed of the wound, because these fabrics are an important indicator of the stage of healing and a sign of any complication present. This color system is an easy method to observe the prevailing characteristics on injury, being used the rating scale of the system Red, Yellow, Black (RYB), where the granulation tissue (red), esfacelo (yellow) and necrosis (black) identified as shown in Figure 5.

4.9 ethical and Legal Aspects of research
This study followed all the guidelines contained in resolution 466/12 the National Council of ethics in research (CONEP). The research was subdued to the Research Ethics Committee of the Public Foundation Hospital de Clínicas Gaspar Vianna (FHCGV). The participant will remain in a State of absolute secrecy and confidentiality. The research takes the referred in its resolution 466/12 of CONEP. The procedures will be performed by signing the consent form free clear participation in the project, and term of release of images of the LPPs.
During the making of LTBI within hospitals, a screen was used as insulation contact to avoid any kind of embarrassment by exposure. Home monitoring, procedures were carried out in the patient's room under the supervision of your caregiver (wife) according to the code of ethics in nursing and the rules of research that involves humans, represented by Resolutions 466/12 and 251 /97 of CONEP, without prejudice to the participants.
4.10 risks and benefits
The use of LTBI in lesions of cutaneous level can lead to physical damage such as photosensitivity, from this point of view the author Kitchen (2003) emphasizes that the ideal is to make a dose of testing prior to treatment; high voltages may lead to Burns for improper handling of the laser. In the present study was conducted a test session, with 2 Joules, 1 cm from the edge peri-ulceral brokered by 2 cm, a score and another. After 24 hours, proceed with thorough assessment step in search of signals like skin irritation, dark spots on the site of the score, then the patient was designated fit to continue the LTBI.
The risk of contamination and infection may exist because, the pen that radiates the laser is not disposable and the patient shows a LPP in calcaneus infected and not law accomplished this injury. LTBI This risk was minimized in order that all recommendations were used for antisepsis and asepsis obeyed in the handling of the equipment, and the order of the bandages was observed, providing a therapeutic treatment with security and protection.
The bioactivity of the laser on collagen synthesis stimulation promotes and assists in the healing of soft tissue (epidermis, DermIS and hypodermis), with analgesic and anti-inflammatory action, increases local Vascularity by assisting the formation of granulation tissue. We can understand, based on the authors Busnardo and Simões (2010), the healing process is complex and includes vascular and cellular changes, epithelial and fibroblast proliferation, synthesis and provision of collagen, elastin and production proteoglycans, and wound contraction.
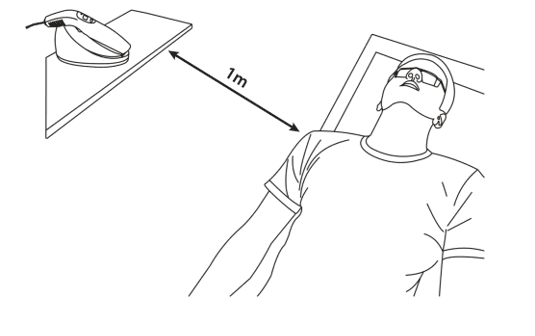
4.11 Biosecurity
Biosecurity can be defined as a set of measures that seeks to minimize the risks inherent in a given activity. In this sense, real is considered the risk of contamination during the realisation of the dressings and this aspect needs to be respected. Hand-washing techniques, used for antisepsis and asepsis, the use of gloves, serum and sterile gauze, the order of carrying out of the procedure in each injury, disposal were fundamental for the biological effectiveness of treatment. For eye protection, goggles were used during procedures of LTBI.
5. Results and discussion
The results of this study were discussed and presented according to the objectives proposed. First, clinical evaluation and description of Mowa and later software LPPs discussion.
5.1 calcaneal pressure injury
This injury, 3 LTBI sessions were used on alternate days. Cleaning was performed with 0.9% saline jets with aid of 40×12 gauge needle connected to the serum, drying performed with sterile gauze, then 4 point applications associated with LTBI scan. Topical coverage elected was to ACT, later the dressing was occluded with gauze and micropore, as shown in the pictures C, D and e.
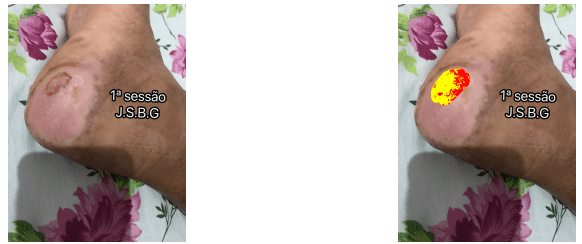
According to the classification of the Mowa, in the first session the LPP submitted the following features: exsuldato absent; infection; no bleeding; not deep; 0.0% necrosis; 65.9% fribrina; 34.1% granulation; 63.5 cm ² area (width: 10.0 cm-height: 9.4 cm).
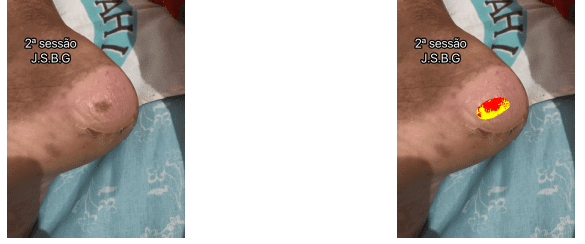
In the second session, the LLP evolves without exsuldato, infection, bleeding, and necrosis. Presented the percentage: fribrina: 51.4%; Granulation: 48.6%; Area: 8.1 cm ² (width: 4.2 cm – height: 2.8 cm). Evolving positively with fibrinous tissue percentage loss of 14.5%; increased 14.5% granulation tissue; and reduction of the total area of 55.4 cm ², being 5.8 cm wide 6.6 cm ² ² of time.

In the third session, the LPP evolves satisfactorily getting zero percentage by the application, since the same does the reading of epithelial tissue. Exsuldato: missing; infection: no; bleeding: no; deep: no; necrosis: 0.0%; fribrina: 0.0%; granulation: 0.0%; area: 0.0 cm ² (width: 0.0 cm-height: 0.0 cm).
5.2 pressure injury in sacrococcygeal
This injury, 15 were used LTBI sessions every other day. Cleaning was performed with 0.9% saline jets with aid of 40×12 gauge needle connected to the serum, realization of mechanical debridement with scalpel blade No. 20 when necessary and drying with sterile gauze, then LTBI with 12 applications punctual associated with scan. Topical coverage elected was to ACT, later the dressing was occluded with gauze and micropore, as shown in the images F, G and H.

According to the classification of the Mowa, in the first session the LPP submitted the following features: Exsuldato: missing; infection: no; bleeding: no; deep: no; necrosis: 8.3%; fribrina: 30.4%; granulation: 61%; area: 15.6 cm ² (width: 4.5 cm-height: 55 cm).
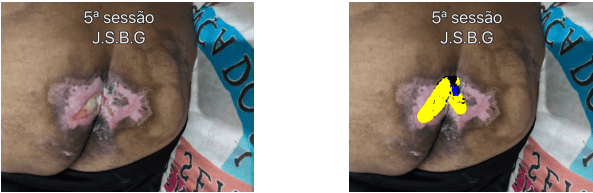
Fifth session, LLP has evolved without exsuldato; infection: no; bleeding; depth; showing the percentage of necrosis: 11.1%; fribrina: 88.8%; granulation: 0.5%; area: 7.4 cm ² (width: 3.8 cm-height: 3.6 cm). Evolving positively with the total area decrease uses 8.2 cm ², being 0.7 cm wide ² to ² 51.4 cm tall.
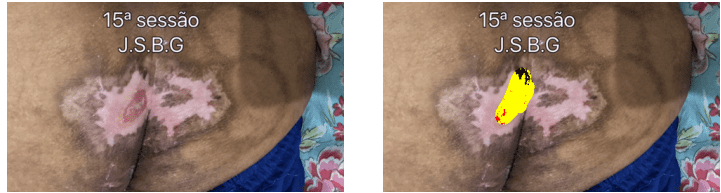
At the 15th session, the LLP evolves without exsuldato; infection; bleeding; depth; showing percentage of 8.6% necrosis; fribrina: 8.8%; granulation: 3.4%; area: 0.6 cm ² (width: 0.8 cm-height: 1.2 cm). Progressing satisfactorily having total healing nádegada, showing the total area decrease uses 15 cm ², being 3.8 cm wide ² to ² 53.8 cm tall.
5.3 factors that interfere with wound healing and use laser
Understanding the cascade of physiological mechanisms available in the process of healing the wounds heal by different mechanisms, depending on their condition. The author Hess (2002) highlights in your study that there are factors that interfere with physiological process which are of local origin and systemic, local factors are characterized as excessive amount of dressing changes and use of inadequate coverage; systemic factors are related to nutritional deficiencies, immunological, circulatory problems and advanced age.
The patient in this study presents three chronic illnesses: diabetes type II, hypertension (SAH) and Chronic Renal Failure (CRF), which is related to systemic factors that interfere in the process of healing beyond the age factor since the same has 68 years.
One of the patient's LPPs is located in calcaneal region, soon the local tissue perfusion is compromised not only by the diabetes, but also for hypertension, which is a pathology related to progressive loss of elasticity of the arteries wall. "SAH, more popularly called ' high pressure ', is related to the force that the heart does to propel the blood to the whole body" (LIMA et al., 2012 apud NOBLE et al., 2001, p. 10).
Still in the context of Comorbidities, it is worth mentioning that the IRC of the patient is a predictor of poor results for any cutaneous pathology. According to Lupi et. Al., (2011), the long-standing kidney pathology causes difficulty to maintain serum protein levels within the normal range, which leads to a delay in the repair process. In the case here, even with the IRC, noted the total healing of injuries, at one time considered favorable, showing the effectiveness of the method.
Age has been reported in several works as a factor of poor prognosis, since there is an inversion of the physiological metabolism. In studies of Mann (2006), the author describes the age factor can interfere on way in the treatment of skin diseases by hydration changes, composition of collages and cell replacement. This infers that lllt might have an early success if the patient hadn't advanced age, as they needed just 15 sessions for healing of one of the buttocks of LPP in the sacrococcygeal region of stage II and 3 sessions for total healing LPP of the calcaneus.
5.4 topical Coverage
The bandages involve cleaning the wound with the use of techniques and fluids which seek to minimize mechanical trauma and chemicals. For Fan et al., (2012), the nurse occupies an essential role in the scenario of indications of toppings and need continuous updates to optimize the use of topical coverage in the wounds, since, on the world market, are offered a range of products that can be used in different stages of treatment of wounds.
The covers feature active differentiated functions, including: cleaning, debridement, bacterial population decline, control of exudate, stimulating granulation and re-epithelialization protection. In this study, coupled with the proper treatment of the patient's injuries and based on various surveys, was shown the use of ACTS.
According to Ferreira, et al. (2012) and Dealey (2007), there are several types of fatty acids, but when it comes to treating wounds, linoleic acid and linolenic acid are the most important. Contribute to the tissue repair process possessing antioxidant and protect cell membranes from free radical attack. In addition to being a protection agent, provides the maintenance of tissue hydration and helps in the healing process of the skin.
As the authors Jorge et al., (2007), papain is a proteolytic enzyme that has the property of non-viable protein substances decomposed. Is marketed in different forms as powder, gel and cream. Has the action debriding, liquefy all devitalized tissue, acting as bacteriostatic and bactericidal, developing and stimulating the granulation. Some care in relation to the handling and packaging of papain are needed, noting that the solution should be used immediately after your preparation to reduce the factors of oxidation, avoid contact with metals and substances composed of iron, iodine and oxygen for these are the elements that turn off the active site of the molecule of papain, protect from light, moisture and heat, and avoid prolonged contact with the air.
The injuries that were treated in this research had a very small percentage of necrotic tissue and papain is still an unstable substance with respect to oxidation, the loss of its effects and still use your topics be little widespread in Brazil, we chose use the ACT on the assumption that the ACT is intended to treat any skin lesion infected or not, regardless of the stage in the healing process.
Angelis and Tirapegui (2013) relating to the ACTS are part of the essential components for maintaining the integrity of the cell membrane and transepidérimica barrier layer of the skin. In Brazil, the use of medium-chain triglycerides and ACTS (ACTS-TG) was popularized in 1994, where he observed clinical effects, in the prevention and treatment of pressure sores. Most of the authors surveyed showed the effectiveness of topical application of the ACTS in pressure injuries for your moisturizing action, showing great result in healing. From this overview, since this product is widely used in Brazil, we try for your use and we achieved positive results.
5.5 Complications of skin and laser
Of acoro with Ribeiro et al. (2010), low-intensity lasers can produce effects in other parts of the body beyond the site where it is irriado. A possible reason for the systemic effect is that cells in the tissue in which they are irradiated produce substances that spread and circulates in the blood vessels and lymphatic system.
Agne (2009) reports that the effects of such radiation on tissues depend on your energy absorption and transformation of this in certain biological processes, since the effect on living structure depends mainly on the amount of energy deposited and the absorption time. To Maxbasnet and Magalhães (2008), the use of laser light at different wavelengths is able to speed up the formation of the epidermis, increase the thickness of the epithelial layer, promoting neovascularization and reorganization of collagen fibers.
When the Professional without qualification performs this type of treatment, the chance of success always exists, but the risk of complications that, so far, is very low, most high. The most common is the treatment doesn't work, leading to patient dissatisfaction, however mild and severe complications can occur such as: redness; burning; swelling that, with appropriate treatment, are reverted in no time. The most serious complications are Burns and can evolve to changes in skin pigmentation, which may be reversible or not, or even leave scars.
In the present study, it was observed that LTBI was to mediate the healing process and complications cited by the authors, because they were taken proper care described in the literature and the LPPs evolved satisfactorily.
5.6 types of dressings and the laser
In the present study, we used laser technology with AGE, we emphasize that the equipment cost is relatively high, approximately R $4,000, but it is relevant to point out that the same is for portable use, with battery and charger and the opportunity to usefulness in other patients, showing a higher benefit costs. Silveira et al. (2016) used the technology of vacuum dressings in patients who had serious injuries to end and achieved positive results.
It is known that the use of cellulose membrane on the wound can be potentiated when associated with propolis extract for your production, this is because antibacterial characteristics of this natural component. The author Sanchez (2012, p. 72) used bacterial cellulose dressings (CB) associated or not to the lllt and emphasizes that "pure CB membranes with propolis are promising materials for treating chronic ulcers hard to heal. For best results, it is suggested the Association of LBI to CB membranes ".
5.7 how much Laser scar provider
Laser therapy promotes cell proliferation, stimulant effects in this feeling, Felice et al. (2009) describes that this fotoestimulante becomes the mitotic process accelerator in skin microbiota, including infectious micro-organisms present. These, when fotoestimulados, they multiply very rapidly by cell excitation, however in the studies the authors Welcome et al. (2007) concluded, from a in vitro research, laser therapy and low power photodynamic (InGaP, 670 nm) did not produce antibacterial effects and/or bacteriostatic, either having been biostimulant effect on bacteria.
The equipment used by the authors was the InGaP Bioset ® brand laser, Dual Physiolux model, with the following parameters: output of 30 mW, 670 nm wavelength light only red, continuous and direct emission with relatively low doses of energy density, and in a single session, this type of irradiation method for zone in an application can generate energy losses.
In the present study, the equipment supplied was the Therapy Xt ®, the methodology of application was of 2 J with the transmitter power output of 100 mW, in the time of 20 seconds per score at a wavelength of 660 pressure gauges. The output power is 70 mW higher when compared for used in bacteria; the length of the wave is 10 smaller gauges, i.e. the length of the wave is less and were used more than a score in relationship to the study before referred to. From this difference constant presented between the equipment and method, means that the potential of the equipment energy Therapy ® Xt is greater and this aspect was the need to use the only uninfected LPPs LTBI.
On comparison between treatment of cutaneous lesions using physical means, Yamada et, al. (2009) conducted a work by applying laser therapy versus high-voltage electrical stimulation, with some advantage to this last, but a significant number we cannot conclude that the result can drive new protocols.
Other assignments for the use of laser therapy are in the current study, such as tummy tuck surgery, Santos (2013) treatment of Burns, Andrade et al., (2010) in bad perforans plant in diabetics Alves et al., (2013). In this way opens up a range of possibilities with the trend of using the common method, if being watched positivity in patients ' prognoses using laser technology, such as the case here discussed.
The author Scott et al. (2009) used the laser on carpal tunnel syndrome and describes which obtained better results than the conventional surgical technique, because the chromophores of greater absorption is the mitochondria, which is numerous in the cell body, dendrites, us in synaptic endings and outnumbered in motor axons. Have the authors Raj et al. (2016) used LTBI in musculoskeletal injuries, including being able to regulate the release of some cytokines responsible for the proliferation of fibroblasts and collagen synthesis, such as fibroblast growth factor (FGF-b) beta factor Transformer Growth (TGF).
Recently, Mejia et al. (2015) reported that the low intensity laser therapy modulates the production of collagen in patients with diabetic foot and the biomodulation is related to several mechanisms, among them the proliferation of fibroblast shown by Maiya et al., (2010), through Histopathological studies. To analyse scientific databases, we decided to use the LTBI in pressure injury grade I and II results of satisfactory healing.
Final considerations
On the above, it was concluded that there was significant improvement in the healing process of the LPPs treated with LTBI adjuvant application showing be a effective therapy, such as Accelerator factor on healing of a patient from LPPs of hospitalization in the ICU. Demonstrated by the outcome of the healing of the wounds of the calcaneus and sacrococcygeal regions, evolving with total reepithelization LPP in 3 sessions of calcaneal LTBI sacrococcygeal region, in the LPP evolved positively showing decreased total area regarding the first session of 15 cm ², being 3.7 cm in width to 53.8 cm tall.
Whereas the cellular lesion unprovision the body homeostasis, and the patient presents 4 systemic factors which slow down the cascade of physiological events occurring systematically in healing: hypertension; Diabetes; chronic renal failure and 68 years, and the injuries have evolved satisfactorily even with these factors to LTBI is a therapy that needs to be considered in the context of the bandages.
Thus, it is suggested the possibility of LTBI in treatment protocols of LPP therefore this intervention accelerated tissue proliferation and increased the local blood supply, with the formation of granulation tissue more organized, favoring a quick healing of the injury. The case study proved an important method to support the design of future clinical studies with a larger sample and randomized capable of producing greater evidence of the benefits of this therapy, since this research has as the limitation of a single patient.
Also concludes that the technological developments of recent times, such as laser treatments, occupy a prominent position. Medicine and more recently aesthetics has been one of the major beneficiaries. In this sense, the use of laser Accelerator factor in the healing process becomes important, especially the importance of improving scientific and technological development in the area of health, in order to contribute to the efficiency of assistance during tissue healing and engaging facilitators of this possibility.
References
AGOSTINI, T.; SILVA. D Hyaluronic acid: active ingredient in cosmetic products. 2014. Available at:<http: siaibib01.univali.br/pdf/tatiane%20agostini.pdf=""> accessed: 17, 2016.</http:>
ANDRADE, F. S. S.D.; CLARK, R. M.; FERREIRA, m. l. effects of Low level laser therapy Promotes healing of skin wounds. Rev. Col.. 2012. Available at: < http://www.scielo.br/pdf/rcbc/v41n2/pt_0100-6991-rcbc-41-02-00129.pdf=""> </>, accessed: 16, Mar, 2016.
ANDRADE, g.; Lima, c. F; ALBUQUERQUE, a. k. (B). Therapeutic laser effects in the process of healing of Burns: a literature review. Rev. Bras. Burns. 2010. Available at:<http: www.sbqueimaduras.com.br/revista/marco-2010/05efeitosdolaser.pdf=""> accessed: 05, Jun of 2017.</http:>
AHMED, G. M; Ubaldo Duarte de Lima MOSER, A.D. of l. Lllt in pressure ulcers: limitations for evaluation of response in people with spinal cord injury. Text Context Nurses, Florianópolis, 2013. Available at: < http://www.scielo.br/scielo.php?script="sci_arttext&pid=S0104-07072013000300035"> </>accessed: 05/06/2017 > data access on: 05 June 2017.
BAGNATO, V.S. the magnificent laser. São Carlos Institute of physics. São Paulo. 2005.
BABU, T. P; BECCARIA, L. M; POLETTI, n. a. risk assessment of pressure ulcers in INTENSIVE CARE and preventive nursing assistance. Rev. of Enf. UERJ. p. 350. may/jun. 2014.
BAPTISTA, i. m. c. Analysis of the effect of low-power laser on prevention of Incisional Dehiscence in cardiac surgery. 2003. 127 f. Dissertation (master in Biomedical Engineering)-University of Vale do Paraíba, São José dos Campos, 2003.
WELCOME, R. G; BRAUN, G; de CARVALHO, a. R; BERTOLINI, G. R. F. effects of photodynamic therapy and a single low-power Laser application in bacteria In Vitro. Rev. physical therapy and research. 2008.
BUSNARDO, V.; BIONDO-SEN, M.L.P. The helium-neon laser effects of low intensity on healing of cutaneous lesions induced in rats. Rev. Bras. Fisioter. San Carlos, v. 14, n. 1, p. 45-51, jan/fev. 2010.
BJORDAL, J.M.; LEE, M.R., JOENSEN, J.; COUPPE. (C); LJUNGGREN, A.; STERGIOULAS. A. systematic review with meta-analysis and procedural assessments of low-level laser therapy in lateral elbow tendinopathy (tennis elbow). BMC Musculoskelet Disord. 2008.
CAMPOS, A. C. L.; BORGES WHITE; GROTH, A.K. healing of wounds. ABCD Arq Bras Cir Dig. 2007 review article. Available in: <http: www.scielo.br/pdf/abcd/v20n1/10.pdf="">.</http:> Access in: 01 Sep. 2016.
CAMERA, v. l. Anatomy and physiology of the skin. São Paulo – SP, 2009. Available at:<http: www.medicinanet.com.br/conteudos/revisoes/2054/anatomia_e_fisiologia_da_pele.htm=""> accessed: 17, 2016.</http:>
COFEN-Opinion-SP-009/2014 COREN CT Menu: Use low-intensity Laser (LBI) by the nurse. Available at: < file:///c:/users/14220208/downloads/coren%20ltbi%20por%20enfermeiros.pdf=""> accessed: 05, Ten of 2016.
CTGAE-opinion No. COFEN 001/2016 PAD number 608/2015 GENERAL COORDINATION of TECHNICAL MANAGEMENT TECHNICAL CHAMBER CHAMBERS and NURSING ASSISTANCE-CTGAE available at: <file: :/users/14220208/downloads/compet%c3%aancia%20do%20enfermeiro%2 ="" 0para%20o%20tratamento%20de%20feridas.pdf="">accessed: 05, Ten of 2016.</file:>
COFEN-Opinion COREN/GO No. 026/CTAP/2016 subject: USE of LASER in the TREATMENT of WOUNDS by PROFESSIONAL NURSES. Available at: <file: :/users/14220208/downloads/parecer-n%c2%ba026.2016-utiliza%c3%a7%c3%a3o-laser-no-tratamento-de-feridas-pro-profissional-enfermeiro.pdf="">accessed: 05, Ten of 2016.</file:>
COLLS, j. La laser therapy, hoy. Centro Documentación Laser, Barcelona, p. 30-70, 1986.
CUNHA, d. Q. Development of an application for laser therapy in wound. 2016. Available at: < http://www.univas.edu.br/mpcas/docs/dissertacoes/27.pdf=""> </>accessed: 03, June 2017
CRESWELL, J.W.W. research project: qualitative, quantitative, and mixed methods. 2. Ed. New York: Bookman, 2010.
DUCCI, A. J.; ZANEI, S.S. V; WHITAKER, I.Y. Nursing workload to Quantify Professional Nursing/patient Ratio in Cardiology ICU. Rev. Esc.de's Nurse. the USP. Vol. 42, no. 4, 10, 2008. Universidade de São Paulo, São Paulo, Brazil. Available in: <file: :/tcc/referencias/2%20duci,%20zanei,%20jorge%20uti.pdf="">.</file:> Access in: 31 Aug. 2016.
FAN, K; TANG, J; ESCANDÓN, J; KIRSNER, R.S. Systematization of dressings for the treatment of wounds. Rev Bras Cir Plast. 2012.
FAREED, L. A.; PINEIRO, A.R. Using Low Power Laser in the healing of wounds. 2009. Available at: <http: www.unigran.br/interbio/paginas/ed_anteriores/vol3_num2/arquivos/artigo6.pdf="">accessed: 16, Mar, 2016.</http:>
FRANCO, D.; Gonçalves, L.F. skin wounds: the choice of appropriate dressing. Rev. Col. Bras. CIR. 2009. Available at: <http: www.scielo.br/pdf/rcbc/v35n3/a13v35n3.pdf="">accessed: 17, 2016.</http:>
GARBERO, M.F. The Skin. Juiz de Fora/MG. Available in: < http://dramariadefatimagarbero.site.med.br/index.asp?pagename="Artigos"> </>. Access in: 01 Sep. 2016.
GARCIA, F.S. L; BASTOS, M.A.; MATOZINHOS, F. P.; TEMPONI HAS, H. R; MELÉNDEZ, G.V. evaluation of risk for pressure ulcer in critical patients. Rev. esc. nurses. USP vol. 45 No. 2. São Paulo. 2011.
Hemorio. State Institute of Hematology. Nursing protocol prevention and treatment of Pressure ulcers. Rio de Janeiro 2010.
HESS, C.T. treatment of wounds and ulcers translatio[ da 4. ed. original]n of Maria Angelica Borges dos Santos; technical review of Sonia Regina de Souza-Rio de Janeiro: Reichmann & Affonso ed., 2002.
ISAAC, C; LADEIRAP. R. S; REGO, F.M. P; ALDUNATE, J. C. B; FERNANDEZ, M.C. healing process of wounds: Physiological Healing. Rev. Med. São Paulo. 2010. Paragraph p. 125, pp. 125-31. Available in: <http: www.revistas.usp.br/revistadc/article/viewfile/46294/49950="">.</http:> Access in: 01 Sep. 2016.
JUNQUEIRA, L. C. U.; LAMB, J. Basic Histology. 11th Ed. Rio de Janeiro: Guanabara Koogan, 2009.
KITCHEN, low intensity laser therapy Electrotherapy: evidence-based practice. 11. Ed. São Paulo. Manole, p. 171-179. 2003.
LEONARDI, R. L. Cosmetology Applied. São Paulo: Editora Santa Isabel, 2008.
MANDELBAUM, S. H.;D I SANTIN, E.P.; MANDELBAUM, M.H.S. Healing: current concepts and Auxiliary Resources. Rev. An bras Dermatol. Rio de Janeiro .2003. Available at: <http: www.scielo.br/pdf/abd/v78n4/16897.pdf="">, accessed: 15, Marc, of 2016.</http:>
LUPI, THE; REZENDE, L; ZANGRANDO, M; SESSIM, M; SILVEIRA, C. B; SEPULCRI, M.S.; DUARTE, D. J.; CARDIM, P; FERNANDES, M; Santos, r. Cutaneous manifestations in terminal kidney disease. Rev. Anais Brasileiros de 2011 Dermatology. Available at: < http://www.scielo.br/pdf/abd/v86n2/v86n2a15.pdf=""> accessed: 04, June 2017.
Medeiros, a. b. f. pressure ulcer in elderly patients: analysis of the prevalence and risk factors. 2006. Fortress available at: < http://srvweb.uece.br/cmacclis/dmdocuments/adriana_bessa_fernandes_medeiro.pdf=""> accessed: 07, June 2017.
MEDEIROS, A. B. F; LEE, C. H. A. F; GEORGE, m. s. b. analysis of prevention and treatment of pressure ulcers by nurses. Rev. esc. nurses. USP, São Paulo, v. 43, n. 1, p. 223-228, Mar. 2009. Available in: <http: www.scielo.br/scielo.php?script="sci_arttext&pid=S008062342009000100029&lng=en&nrm=iso">.</http:> Access in: 31 Aug. 2016.
MEJIA, D. P. M; COSTA, V. C. Laser therapy and ultrasound in the treatment of postoperative tummy tuck plastic surgery: review of the literature. 2015. Available at: < http://_laserterapia_e_ultrassom_no_tratamento_pys-operatyrio_da_cirurgia_plystica_de_abdominoplastia_revisyo_de_literatura.=""> accessed: 05, June 2017.
MANNING, G. C. (C); da SILVA, C. A; MARQUES, A. M.; PATEL, A. L. B. The effectiveness of Laser Phototherapy in Tissue Repair in patients with Systemic Functional Disorder. C&D-Electronic Journal of Fainor, malkajgiri, v. 7, no. 2, p. 71-84,/dez.. 2014. Available in: <http: srv02.fainor.com.br/revista/index.php/memorias/article/viewfile/321/194="">. Access in: 06, June 2017.</http:>
MIYAZAKI, M. Y; CALIRI, M.H. L; SANTOS, C. B. On Pressure Ulcer Prevention knowledge Among Nursing Professionals. Rev. Latin Am. ENF[online]. 2010, vol. 18, no. 6, pp. 1203-1211. ISSN 1518-8345. Available in: < http://www.scielo.br/pdf/rlae/v18n6/22.pdf=""> </>. Access in: 01 Sep. 2016.
MATTHEWS, J.; BORGES, AND L; C. R; LAMB, D.C.; ROSA, E. G; Rock, N.A. Concept and classification of pressure injury: updating the national Pressure ulcer advisory panel. Rev. of Enf of the Midwest v. 6i2 Miner, p. 2293. May/Aug. 2016.
MOSHKOVSKA. T; MAYBERRY. J. It is time to test low level laser therapy in Great Britain. Post Grad Med j. 2005
OLIVEIRA, S. H.; WALK, R. T.; SILVA, M.L. N; DINIZ, E.R. Pressure Ulcers In intensive care Unit: analysis of the incidence of injuries and installed. 2013. Available at: <http: www.abeneventos.com.br/anais_senpe/17senpe/pdf/0684co.pdf="">accessed: 10, Apr from 2016.</http:>
OLIVEIRA, c. a. g. s. Association of laser therapy with papain on healing of diabetic ulcers on the lower limbs. 2007. Available in < http://biblioteca.univap.br/dados/000002/00000241.pdf=""> Access in: 04 June 2017
PEREIRA, S; Smith, h.m., Pressure Ulcers: perception of the relatives about the emotional impact and intangible costs. Rev of Enf, Series-n° 7-July 2012, pp. 139-148. Available in: <http: www.scielo.mec.pt/pdf/ref/vseriiin7/seriiin7a15.pdf="">.</http:> Access in: 01 Sep. 2016.
PEROCA, j. d. Understanding the physics of Laser. Available in:< http://143.107.153.201/restauradora/laser/fisica.html="">. Access in: 06, June 2017.
PARKER, P. R; PAULA, j. (B); CIELINSKI. J; PILONETTO. M; BAHTENE, L.C.V. low intensity laser effects on bacterial culture in vitro and in vivo infected wound. Rev. Col. Bras. CIR. 2014. Available in< http://www.scielo.br/pdf/rcbc/v41n1/pt_0100-6991-rcbc-41-01-00049.pdf=""> </> Access in: 06, June 2017.
POLIT, D. F; Beck, C.T. Fundamentals of Nursing Research: evaluation of evidence for the practice of nursing. Porto Alegre: New Haven, 2011.
RAMIRES, R.C; MEJIA, d.p.m. The effects of laser on treatment of decubitus ulcer – literature review. 2011. Available at: < http://www.unifafibe.com.br/revistasonline/arquivos/revistafafibeonline/sumario/21/21112012211553.pdf=""> accessed: 07, June 2017.
ROCK, C. L. J. V. JUNHIOR ROCK, M; AARESTRUP, B.J. V; AARESTRUP, f. m. Inhibition of the expression of Cyclooxygenase 2:00 pm skin wounds of NOD Mice subjected to low intensity Laser therapy. Vasc Bras 2012.
SANTOS, j. (B); PORTO, S. G; SUZUKI, L.M.; SOSTIZZO, L.R. Z; ANTONIAZZI, J. L.; ECHER, i. c. evaluation and treatment of wounds: Guidelines for health professionals. Hospital das Clinicas de Porto Alegre. 2011.
SANCHEZ, f. evaluation of processor of tissue repair in chronic ulcers using bacterial cellulose dressings associated or not to laser therapy. 2012 available at:< https://www.passeidireto.com/arquivo/5880596/avaliacao-do-processo-de-reparacao-tecidual-em-ulcera-cronicas-utilizando-curati=""> </> accessed: 09, June 2017.
SILVA, L. A.; LEE, T. F.; FAREED, L. A.; PINEIRO, A.R. Using Low Power Laser in the healing of wounds. 2009. Available at: <http: www.unigran.br/interbio/paginas/ed_anteriores/vol3_num2/arquivos/artigo6.pdf="">accessed: 16, Mar, 2016.</http:>
SILVA, FR. D; BARBOSA, M. H; AGUILAR, d. F, OLIVEIRA, l. P, MELO, A.F.: evaluation of Pressure ulcer risk factors in hospitalized patients in a university hospital.
Rev. Email Nurses. [Internet]. 2011.
SILAVA, R.C.L.; FIGEREDO, N.M.A.; MANOHAR, I.B.; COSTA, M.M.; SILVA, C.R.L. Wounds: basics and updates in nursing. São Caetano do Sul. SP: Yendis Publisher, 2011.
SILVEIRA, D.; SON, W.V.N. F; GUIMARÃES, J.; CASTRO, D.; FERRACINI, A.M. application of negative pressure therapy in the treatment of infected wounds. Case study. Rev. bras. ortop. Vol. 51 No. 6 São Paulo Nov. 2016/Dec.
SIMON, c. m. f. pressure ulcer in the intensive care unit and compliance of nursing actions. Ribeirão Preto. 2010.
TAZIMA, M. F. G. S.; VICENTE, Y. A. M. V. A.; MORIYA, t. wound Biology and Healing. 2008.
THULER, S. R.; Dantas, S. R. P. E. Pressure Ulcers prevention and treatment: quick guide. Available at: <http: www.coloplast.com.br/global/brasil/wound/cpwsc_guia_pu_a5_d7.pdf="">accessed: Apr 10, 2016.</http:>
WADA, A. P; GRANDSON, NO T; FERNANDEZ, M.C. pressure ulcers. Rev of São Paulo. p. 172. Jul. 2010.
YAMADA, AND F; RAO, P. L; PARKER, T. F;. Case report: comparison of laser therapy and high-voltage electrical stimulation in surface ulcer. 2009 Available:<http: www.inicepg.univap.br/cd/inic_2009/anais/arquivos/re_0802_0625_01.pdf="" ="">Access in: 06, June 2017</http:>
CLARIFICATION OF THE RESEARCH
The research has as main objective to investigate the healing effects, through the application of the laser as a therapeutic resource complement in Pressure Sores (LPP) of grade I (GI) and grade II (GII), in an intensive care unit. The study will be carried out in the period from January to March 2017, will have data collection through the realization of lllt and the monitoring of the LPP, the data obtained will be analysed and organized in the form of scientific work.
After the signature of this term, participants authorized your participation in the study and will not have their identities revealed. It is important to note that this research will not have the same costs, will not give the right to remuneration in cash and will not bring secondary damage the health of individuals. The case included judge research embarrassing or for any reason feel harmed by your participation in this study, may decide by giving up participating in the study, refusing to sign this document, and may request deletion of your research, although it has signed previously, without any kind of represaria, coercion or retaliation.
The risks to physical, moral or psychological integrity of the participants of the study may exist because the subject may possibly be victims of iatrogenic, this risk will be minimized since the procedures will be performed by a skilled professional to exercise such function, patients will be monitored on a multidisciplinary squad and the achievements of the procedures will be made with the use of appropriate materials and in no time the data will be used for the purposes are not scientific in nature.
ATTACHMENTS
ANNEX A: EQUIPMENT MANUAL
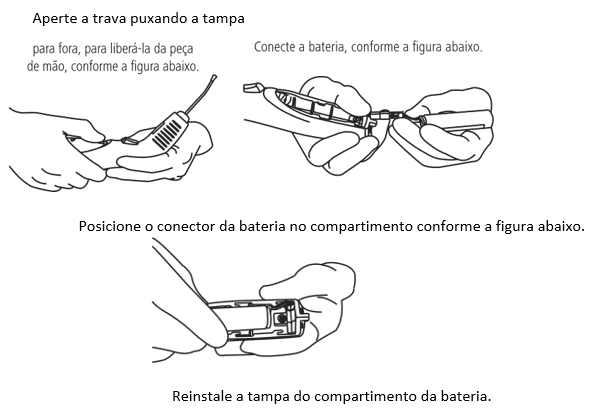
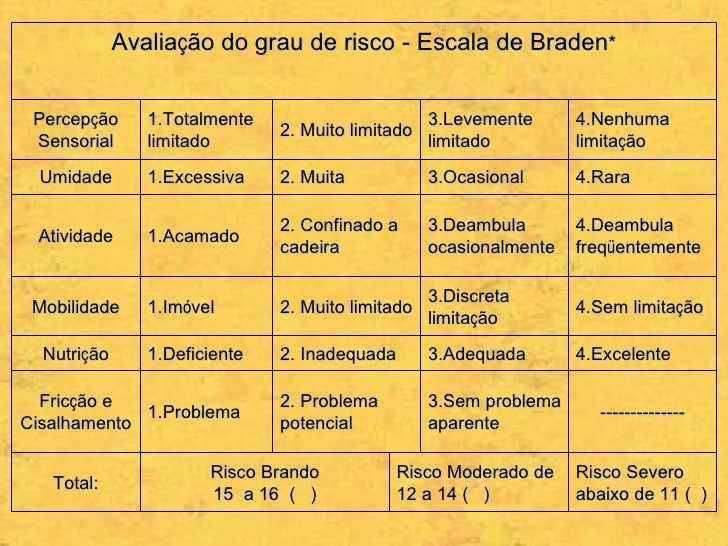
The Therapy XT is an equipment manufactured with the highest technology, according to the latest national manufacturing standards required by ANVISA – national health surveillance Agency.
The Therapy XT is designed to be used by medical professionals, dental and physiotherapy. The professional must be qualified for the application of the techniques related to the product. Misuse may result in irreversible damage.
EQUIPMENT FUNCTION
The Therapy XT red and infrared laser light emits to the anti-inflammatory, analgesic and healing purposes.
OPERATION OF THE EQUIPMENT
Through a small display and three buttons displays and operator performs all the functions and settings of the unit.
INDICATIONS
The Therapy XT features the following information in the respective fields:
DENTISTRY
- Repair of soft tissue (Red Laser): canker sores and ulcers, traumatic systemic diseases with oral manifestation, Lichen Planus, Lupus Erythematosus, Pemphigus Vulgaris, hiperplástica gingivitis (diabetic), angular Cheilitis, gingivitis, post-op, TMJ dysfunction.
- Repair of bone tissue (infrared Laser): orthodontics, implantology, Periodontology, dental extraction, trauma, bone biostimulation.
- Repair of Dental Tissue (Red and infrared Laser): pós-preparo, cavity pós-raspagem hypersensitivity hypersensitivity, amelogenesis imperfecta, Dentinal hypersensitivity. • Nerve repair (infrared Laser): neuralgia, paresthesia, paralysis, pain syndrome.
- Other applications (Laser red and infrared): Alveolitis, edema, xerostomia, pericoronarite, benign migratory Glossitis, anesthesia, herpes simplex, herpes zoster.
MEDICINE IN GENERAL
- Chronic wounds (Red Laser): lower limb ulcers, venous ulcers, arterial ulcers, diabetic ulcers, skin ulcers, Venous Stasis ulcers different etiologies, skin wounds.
- Chronic wounds (Infrared and Red Laser): decubitus ulcers.
- Fractures (Red Laser): fracture of femur closed fracture of the middle third.
- Regeneration (Red Laser): regeneration of cartilage and bone, increase of white blood cells and leukocytes.
- Inflammation (Red Laser): lung inflammation.
- Inflammation (Red and infrared Laser): acute inflammation, acute inflammation and carrageenan.
- Other (Laser red): diabetes, post-operative surgical vascular micro-current platform.
- Other (infrared Laser): Sjogren's syndrome.
PHYSICAL THERAPY
- Red Laser: Contact Dermatitis, Burns, pressure ulcers, diabetic ulcers, varicose ulcers.
- Infrared laser: articulating hand, arthritis, rheumatoid arthritis, biomodulation, neck pain, Pain, inflammatory processes DMED DMED, epicondylitis, faceite plant, fibromyalgia, gonartrose, rotator cuff injury, muscle injury, injuries to cartilage, peripheral nerve injuries, low back pain, osteoarthritis, facial paralysis, paresthesia, post-surgical, nerve repair, carpal tunnel syndrome, boost myofascial release pain syndrome, tendinitis of the calcaneus, patellar tendinitis, tendinopatias.
CONTRAINDICATIONS
Avoid use in patients with the following characteristics:
- Pregnant or lactating.
- Individuals with skin cancer episode in irradiated region.
- Patients with glaucoma.
- Patients with cataracts that are not under medical supervision.
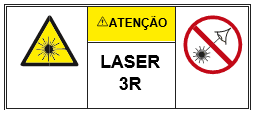
CLASSIFICATION
| Standard/Directive | Classification |
| IEC 60601-1 | Internally Powered equipment and type B applied part |
| MDD 93/42 (European Union) | IIB |
| DRC 185/2001 (ANVISA) | III |
| IEC 60825-1 | 3R |
SPECIFICATIONS
| Infrared laser | Features | |
| Wavelength | 808 nm ± 10 nm | |
| Transmitter power output | 100 mW ± 20% | |
| Red Laser | Features | |
| Wavelength | 660 nm ± 10 nm | |
| Red Laser | Features | |
| Transmitter power output | 100 mW ± 20% | |
| Red Laser (Laser Sights) | Features | |
| Wavelength | 660 nm ± 10 nm | |
| Transmitter power output | 0.5 mW-2.5 mW | |
GENERAL CHARACTERISTICS
| Features | Specifications |
| Supply voltage | 100-240 V ~ |
| Current (input) | Alternating current |
| Current (output) | Direct current |
| Input power | 25 VA |
| Mode of operation | Continuous |
| Protection against electric shock | Internally powered |
| Uncertainty of time (seconds) | ± 4% |
| Uncertainty of energy (Joules) | ± 20.4% |
| Frequency | 50/60 Hz |
| Degree of protection against penetration of water and solid objects | IP20 |
| The lasers operating mode | Continuous operation |
| Dimension of handpiece | 21 cm (height) x 3 cm (width) x 5 cm (depth) |
| Dimension of handpiece holder | 11 cm (height) x 6 (width) x 19 cm (depth) |
| Handpiece weight | 0.18 Kg |
| Support weight of handpiece | 0.12 Kg |
| Useful diameter optical fibers | 600 µm each fiber |
| Operating temperature | 10° C-30° C |
| Battery | Li-ion 3 .7V 18650 with protection circuit |
| Manufactured and tested according to: | IEC 60601-1, IEC 60601-1-2, IEC 60685-1 and IEC 62034. |
| Version of the software | 11 |
SAFETY-IMPORTANT SAFEGUARDS
- Read this manual completely before using the equipment.
- Caution – use of controls or adjustments or performing other procedures not specified here may result in hazardous radiation exposure.
- Caution – fumes and/or smoke may contain laser particle of living tissue.
- Considering that the product will be used by qualified personnel, additional training specific to the operation of the equipment is not necessary. However, we recommend reading the complete instruction manual before using the equipment.
- If the equipment is not used for some time, the battery must be removed.
- Battery replacement by personnel with inadequate training can result in a hazard (such as excessive temperatures, fire or explosion).
- The laser light may cause eye injuries. All the people present at the place where there is light emission laser must protect the eyes. Three green glasses (for operator, Assistant and patient) are provided with the Therapy XT. Only the glasses provided by DMC should be used with the equipment.
- Never look directly into the laser light emitted and mainly do not direct it on anyone, but that is under treatment.
- Shiny surfaces can reflect the laser light toward the eyes.
- Never radiates tumor processes directly, the laser can stimulate them.
- Never radiates infectious processes directly, the laser can exacerbate them.
- Never radiates an undiagnosed injury.
- Don't radiate the beam on the womb of women with less than three months of gestation.
- Only qualified professionals should operate the equipment. Misuse may result in irreversible damage.
- Only the components mentioned in this manual must be used in conjunction with the equipment.
- The equipment must not be used with cord or power supply other than those provided by DMC, as this may result in increased emissions or decreased immunity of the unit.
- To avoid the risk of electric shock, this equipment must be connected only in power outlets with grounding.
- Do not connect the power cord in hard-to-reach outlets.
- When removing the mains cable always pull by the plug.
- Any modification to the equipment is allowed.
- The inputs/outputs of air for ventilation of the equipment must not be obstructed.
- Do not apply any type of protective film on handpiece to prevent the obstruction of air input/output for ventilation.
- Do not install the equipment in a location subject to direct sunlight, excessive dust or mechanical vibration.
- There is risk of fire and/or explosion when the output of the laser has been used in the presence of flammable materials, solutions or gases, or in an environment Rico in oxygen. The use of flammable anesthetics or oxidative gases such as nitrous oxide (N2O) and oxygen, should be avoided. Some materials, e.g. cotton, when saturated with oxygen, can ignite the high temperatures produced. The solvents of adhesives and flammable solutions used for cleaning and disinfecting must evaporate before the equipment being used. One should pay attention to the danger of endogenous gas ignition.
- The user must be exposed to the noise of the equipment for a maximum of 8 hours per day.
- Due to the small size of the equipment, some security items could not be entered as: means of protection against unauthorized use, control and emergency stop of the laser. In this way, the user must keep the equipment in a safe place and protected.
ITEMS OF SAFETY EQUIPMENT
Aiming beam
The equipment uses a targeting beam of low intensity. This laser is visible and for the indication of the anticipated impact of the laser point infrared.
As the targeting beam passes through the same beam delivery system, this work offers a good way to check the integrity of the delivery system. If the aiming beam is not present on the distal end of the delivery system, if your intensity is reduced or if this seem diffuse, this is a possible indication that the delivery system is damaged or is not working properly.
Alarms
For operator safety, the equipment will beep while the laser is active.
Spacer
Sending a spacer to be inserted in the optical fiber tip, so as to have an application for contact, i.e. the spacer is a product applied part. To perform the replacement of the spacer just pull what has already been used, cleaning of the equipment and the new spacer, as item "cleaning/disinfection", and inserts it at the tip of the optical fiber.
Led handpiece
When the led of the handpiece is flashing fast, the laser was fired.
LIST OF COMPONENTS
The Therapy XT is made up of the following parts and accessories:
Accessories:
- Electronic media
- 3 goggles
- User manual
- Warranty
- Carrying case
Parts or additional accessories can be purchased at DMC through the following codes:
- Power cord: 010130131
- Power supply: 010990317
- Goggles: 050020001
- Battery: 110030182
- Spacer: 110030078. The spacer has an individual package with the product code, with the forbidden symbol reuse and the manufacturer's information, i.e. DMC equipment Ltd import and export, as below:
Code: DMC EQUIPMENT LTD import and export. | Street Sebastião de Moraes, 831-Jd. Dawn-São Carlos/SP | CEP 13562-030 | w ww.dmcgroup.com.br
All accessories and parts described above are for the exclusive use of the Therapy equipment XT.
LASER NOTICES
Warning the handpiece:
The label below indicates the exposure class 3R laser radiation.
Warning the handpiece:
The label below illustrates the laser radiation alert, according to IEC 60825-1.
HANDPIECE
EQUIPMENT/PATIENT/OPERATOR POSITION
The equipment should be used in medical clinics, dental or physiotherapy. It must be positioned on a bench and connected to a power outlet, as shown in the illustration below.
The spacer inserted into the handpiece must be in contact with the patient and the professional must be holding the handpiece, as the image below:
INSTALLATION
To install the battery cartridge into the handpiece follow the procedures below:
Before connecting the equipment for the first time it is necessary to charge the battery.
There are two ways to charge the battery: connecting the power supply directly to the handpiece or the support with the handpiece.
Connect the power cable of the power supply into a grounded outlet. A complete recharge of the battery takes approximately 3 hours and is indicated in the display by the code "CC" and the blue led flashing slowly into the handpiece.
INSPECTION BEFORE USE
Before each use check the condition of the handpiece and the power supply cables. The cables must not be broken, twisted, crushed, with external protection covers cut or with the inner conductors exposed. The plastic housing of the handpiece must not be broken. Optical fiber must not be damaged.
USE
Press any button to switch on the equipment. To turn it off, press both the left and right buttons to switch off (the code "of" appears in the display). After 90 seconds of inactivity the equipment switches off automatically to save battery.
Select the laser transmitter by pressing the left button on the handpiece. Select the energy irradiated by the laser emitter, by pressing the right button on the handpiece. The values are indicated in the display. The irradiation time is automatically adjusted depending on the selected energy and displayed on the display in seconds, Countdown when you press the activation button.
To activate the laser transmitter press the activation button. If the user wishes to stop the laser emission, simply release the activation button. To resume the laser emission from the breakpoint, press the activation button or press the right button to start a new cycle of application. At the end of the cycle, the timer is restarted automatically to the last value selected and the transmitter is turned off.
The code "Cb" on the display indicates the end of the battery charge, requiring re-charging. The battery can be recharged with the handpiece on the support with the power supply connected to same or with the power supply connected directly to the handpiece.
A complete recharge of the battery takes approximately 3 hours and is indicated by a blue flashing of the LEDs as incomplete and by display when full (code "CC").
By pressing the left and right buttons simultaneously, will be displayed in the display the battery charge level. The level is indicated by code "b" followed by a number from 1 to 9 (ex. "b5"), and "b1" indicates minimum charge and "b9", full load, since the charger is not connected.
When not in use, keep the handpiece on the bracket to prevent falls and charge the battery.
The equipment will be always available mode, i.e. When you press the activation button the laser will be issued.
SUBMISSION PROCEDURE
To pull the plug, press the left and right buttons until turn off. Otherwise, after 90 seconds of inactivity the equipment switches off automatically to save battery.
REPLACING THE BATTERY
The battery capacity of storing cargo decreases with time. When the battery is too low you will need to replace it. Follow the replacement procedure below:
- Press the latch on the battery compartment cover and pull out of the handpiece.
- Remove the battery from the compartment and release the connector.
- Connect the new battery, positioning correctly the connector into the battery compartment.
- Insert the battery into the compartment and reinstall the lid. The procedure is illustrated in item "installation".
New batteries must be purchased exclusively at DMC.
The battery of the XT lithium Therapy on composition and should not be discarded in the household waste.
NETWORK ISOLATION
In case of emergency or to clean the appliance, the power cord must be removed from the power socket.
CLEANING/DISINFECTION
- Before being cleaned/disinfected, the equipment should be disconnected from the power outlet, to avoid the risk of electric shock;
- The handpiece and your support should be cleaned/disinfected using a soft cloth dampened with 70% alcohol;
- The goggles can be washed in lukewarm water and neutral detergent.
THE SPACER IS FOR SINGLE USE ONLY. Therefore, this should be cleaned/disinfected with 70% alcohol before use and then discarded. New spacers must be purchased from the DMC equipment.
Do not wash or drain liquids into the handpiece or your support.
The equipment, parts and accessories are not Sterilizable. Any method of sterilization will damage the same resulting in the cancellation of the warranty.
Cleaning/disinfection of handpiece and your support can be performed multiple times, not affecting the finishing surface.
PREVENTIVE MAINTENANCE
The equipment should be calibrated annually by the manufacturer. The manufacturer assumes no responsibility for the safe operation of the equipment if the calibration is not held.
All technical assistance services, such as updates, repairs, calibration, etc. should be performed only by the manufacturer. Circuit schematics, parts lists, descriptions, instructions for calibration and verification are not made available to unauthorised by the manufacturer.
If maintenance or other technical assistance service is carried out by unauthorized personnel, the manufacturer assumes no responsibility for the safe operation of the equipment.
Before each use check the condition of the handpiece and the power supply cables. The cables must not be broken, twisted, crushed, with external protection covers cut or with the inner conductors exposed. The plastic housing of the handpiece must not be broken. Optical fiber must not be damaged.
Do not attempt to disassemble the handpiece or your support. In case of malfunctions contact equipment with the technical assistance of the DMC.
STORAGE AND TRANSPORT
The equipment must be stored in a dust-free environment, without direct exposure to sunlight and away from chemicals and cleaning agents.
The equipment must be stored, transported and used in the following environmental conditions:
- Temperature: + 10oC to + 40
- Humidity: 30% to 75%.
- Atmospheric pressure: 700hPa to 1060hPa.
Avoid mechanical shocks, blows and vibrations in equipment.
PROBLEMS AND POSSIBLE SOLUTIONS
| Problem | Possible solution |
| The equipment will not turn on | -Check that the battery is well connected.
-Check that the outlet is energized. -Recharge the battery. -Contact the DMC. |
| The battery charge runs out quickly | -Check the battery charge level (see item "use") and recharge the same. If the charge level does not change with the shipment, contact the DMC. |
| Seemingly weak laser emission | -Remove the optical fiber spacer and check for accumulation of residues on the face. Clean with cotton moistened in 70% alcohol. |
DISCARD
At the end of the useful life of the equipment and its components, these may cause environmental contamination or be used improperly. To minimize these risks, the client should discard the equipment pursuant to local laws.
The battery contains lithium and XT Therapy should not be discarded in the household waste.
LASER DELIVERY SYSTEM
The equipment has a red laser diode and an infrared laser diode. Two optical fibers lead the laser light emitted by each transmitter. The optical power emitted is controlled through electric current in laser diodes.
CALCULATION OF BEAM DIVERGENCE
Applied standard: 60825-1:2014/3.13 Sub-clause
The beam divergence to 600 µm fiber is 0.45 ± 0.03 rad rad.
ELECTROMAGNETIC EQUIPMENT SAFETY STANDARDS
Below are described in the tables that represent the emission standards and electromagnetic immunity.
| Guidance and manufacturer's declaration – electromagnetic emissions – for all equipment and
System [IEC 60601-1-2 / 2007 – subcl. 6.8.3.201 a) 3)] |
|||
| The Therapy XT is intended for use in the electromagnetic environment specified below. The client or user of the Therapy XT must ensure that it is used in such an environment. | |||
| Immunity test | Compliance | Electromagnetic Environment-Guidance | |
| RF emissions
ABNT NBR IEC CISPR 11 |
Group 1 As | The Therapy XT uses RF energy only for its internal functions. Therefore, its RF emissions are very low and are not likely to cause any interference in nearby electronic equipment. | |
| The Therapy XT is convenient for use in all establishments other than intended for domestic use or that are not directly connected to a public network of electric power supply of low voltage feeding buildings used for domestic purposes. | |||
| RF emissions
ABNT NBR CISPR 11 |
Class "A" | ||
| Harmonic emissions
IEC 61000-3-2 |
Not applicable | ||
| Emissions due to voltage fluctuation/flicker. IEC 61000-3-3 | Not applicable | ||
Table 1: compliance information electromagnetic emission requirements based on Table 201 – 60601-1-2, 2007.
| Guidance and manufacturer's declaration – electromagnetic immunity – for all Therapy XT-
[IEC 60601-1-2 / 2007 – subcl. 6.8.3.201 a) 6)] |
|||
| The Therapy XT is intended for use in the electromagnetic environment specified below. The client or user of the Therapy XT must ensure that it is used in such an environment. | |||
| Immunity test | Test level
ABNT NBR IEC60601 |
Conformance level | Electromagnetic Environment-
Guideline |
| Electrostatic discharge
(ESD) IEC 61000-4-2 |
± 6 kV contact
± 8 kV air |
As | Floors should be wood, concrete or ceramic. If floors are covered with synthetic material, the relative humidity should be at least 30%. |
| Electrical fast transients/pulse train (Burst)
IEC 610004-4 |
± 2 kV on the mains lines
± 1 kV on the input/output lines |
As | Power quality should be that of a typical commercial or hospital environment. |
| Outbreaks
IEC 61000-4-5 |
± 2 kV line (s) to Earth
± 1 kV line (s) the line |
As | Quality of supply of energy should be that of a typical commercial or hospital environment. |
| Voltage dips, short interruptions and voltage variations on power supply input lines IEC 61000-4-11 | 5% < Ut
(> 95% voltage drop in Ut) for 0.5 cycles. 40% Ut (60% of voltage drop in Ut) for 5 cycles 70% Ut (30% of voltage drop in Ut) for 25 cycles. 5% < Ut (> 95% voltage drop in Ut) for 5 seconds |
As | Quality of supply of energy should be that of a typical commercial or hospital environment. If the user of the Therapy requires continued operation during XT power interruption, it is recommended that the Therapy XT is powered by an uninterruptible power supply or a battery. |
| Power frequency magnetic field (50/60 Hz)
IEC 61000-4-8 |
3 A/m | As | Power frequency magnetic fields should be at levels characteristic of a typical location in a typical commercial or hospital environment. |
| NOTE: Ut is the supply voltage c. a. prior to application of the test level. | |||
Table 2: compliance information electromagnetic immunity requirements based on Table 202-60601-1-2, 2007.
| Guidance and manufacturer's declaration – electromagnetic immunity – non-Equipment
LIFE SUPPORT- [IEC 60601-1-2 / 2007 – subcl. 6.8] |
|||
| The Therapy XT, is intended for use in the electromagnetic environment specified below. The client or user of the Therapy XT must ensure that it is used in such an environment. | |||
| Immunity test | Test level of ABNT NBR IEC 60601 | Conformance level | Electromagnetic Environment-
Guideline |
| RF Conducted
IEC 61000-4-6 Radiated RF IEC 61000-4-3 |
3 Vrms
150 kHz to 80 MHz 3 V/m 80 MHz to 2.5 GHz |
3 V
3 V/m |
Equipment for portable and mobile RF communication should not be used near any part of the Therapy XT, including cables, with the separation distance, calculated from the equation applicable to the frequency of the transmitter.
Recommended separation distance D = 10.10 m D = 10.10 m (80 MHz to 800 MHz) D = 20.20 m (800 MHz to 2.5 GHz) Where P is the maximum power output of transmitter rated in watts (W) according to the transmitter manufacturer and D is the recommended separation distance in meters (m). It is recommended that the field intensity established by the RF transmitter, as determined by an electromagnetic inspection on location, is less than the compliance level in each frequênciab range. Interference may occur around equipment marked with the following symbol:
|
NOTE 1 – 80 MHz and 800 MHz, the higher frequency range.
NOTE 2 – these guidelines may not apply in all situations. Electromagnetic propagation is affected by absorption and reflection from structures, objects and people.
AAS field intensities established by fixed transmitters, such as base stations, telephone (cellular/wireless) and land mobile radios, amateur radio, AM and FM radio broadcast and TV transmitters cannot be predicted theoretically with precision. To assess the electromagnetic environment due to fixed RF transmitters, an electromagnetic inspection is recommended on the site. If the measured field strength in the location in which the Therapy XT is used exceeds the level of conformity used above, the Therapy XT should be observed to verify normal operation. If abnormal performance is observed, additional procedures may be necessary, such as reorientation or replacement Therapy XT.
b above the frequency range 150 kHz to 80 MHz, field strength should be less than 3 V/m
Table 3: compliance information electromagnetic immunity requirements for equipment that does not target the LIFE-SUPPORT based on Table 204-60601-1-2, 2007.
| Minimum recommended separation distances between portable RF communication equipment and mobile and the Therapy XT. | |||
| The Therapy XT is intended for use in the electromagnetic environment in which radiated RF disturbances are controlled. The client or user of the XT Therapy can help prevent electromagnetic interference by maintaining minimum distance between RF portable communication equipment or mobile (transmitters) and the Therapy XT, as recommended below, according to the maximum power communication equipment output. | |||
| Nominal maximum power output of transmitter (W) | Separation distance according to frequency of transmitter (m) | ||
| 150 kHz to 80 MHz | 80 MHz to 800 MHz | 800 MHz to 2.5 GHz | |
| 0.01 | 0.12 | 0.12 | 0.23 |
| 0.1 | 0.37 | 0.37 | 0.74 |
| 1 | 1.2 | 1.2 | 2.3 |
| 10 | 3.7 | 3.7 | 7.4 |
| 100 | 12 | 12 | 23 |
| For transmitters with a maximum rated output power not listed above, the recommended separation distance (in metres) can[m] be determined using the equation applicable to the frequency of the transmitter. | |||
| Note 1: at 80 MHz to 800 MHz, the separation distance for the higher frequency range. | |||
| Note 2: these guidelines may not apply in all situations. Electromagnetic propagation is affected by absorption and reflection from structures, objects and people. | |||
WARRANTY
- The equipment manufactured and/or marketed by DMC are guaranteed for 24 (twenty-four) months from the date of purchase against manufacturer's defects.
- The warranty only covers manufacturing defects or materials used in the manufacture of the products. The warranty does not cover shipping costs.
- The warranty is automatically canceled if any electrical, physical abuse, if the parts are changed, or if applications other than those for which the equipment has been developed.
- In the case of equipment repaired outside of the warranty period, it will only be extended to components replaced.
- The causes of most common defects come from physical shock applied to the unit, where the warranty is cancelled.
- The DMC shall not be liable for personal injury or property damage resulting from improper use of the equipment for her produced and/or marketed, getting up to the user to provide security measures, in order to avoid such occurrences.
- DMC's liability with respect to the use of the equipment and its consequences, is limited to the replacement value of the same.
The equipment will only be guaranteed by the manufacturer:
- Assembly operations, extensions, adjustments, modifications or repairs are carried out by persons authorized by him;
- The wiring of the environment in question is in accordance with the appropriate requirements;
- The equipment is used according to the instructions.
[1] The eighth academic semester of nursing of the Centro Universitário do Pará State.
[2] The eighth academic semester of nursing of the Centro Universitário do Pará State.
[3] Guidance counselor, Nurse, doctor and Professor of Nursing course at Centro Universitário do Pará State.
[4] Coorientadora, Nurse, doctor and Professor of Nursing course at Centro Universitário do Pará State.