ORIGINAL ARTICLE
PEIXOTO, Leonardo Ribeiro [1], NASCIMENTO, Vanessa Daniele de Sousa [2], ALVES, Renata Maria Coutinho [3], BRITO, Caio Vinícius Botelho [4]
PEIXOTO, Leonardo Ribeiro. Et al. Aspects of prevention of venous thromboembolism in patients admitted to a clinical ward. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year 06, Ed. 04, Vol. 11, pp. 71-83. April 2021. ISSN: 2448-0959, Access link: https://www.nucleodoconhecimento.com.br/health/venous-thromboembolism
ABSTRACT
The aim of this research was to analyze the adequate coverage and achievement of venous thromboembolism (VTE) prophylaxis used in high-risk patients admitted to the clinical ward. For this, 91 medical records of patients at high risk for VTE during a period of 3 months were analyzed. VTE prophylaxis was performed correctly in 70% of patients, the prevalence of thrombosis was: 7.6% overall, 10.7% in patients who did not receive adequate prophylaxis and 6.3% in those who received adequate prophylaxis. Therefore, it is observed that adequate prophylaxis for VTE was underutilized, following global and national trends; strategies such as: the formulation of a clear protocol for the prevention of VTE – whose completion was mandatory – and which was attached to medical records; use of electronic medical records and continuing education of health professionals are valuable strategies to increase adequate VTE prophylaxis coverage, mitigating hospitalization time, avoidable deaths and costs to the health system.
Keywords: Venous Thromboembolism, Prophylaxis, Hospitalized Patients.
1. INTRODUCTION
Venous thromboembolism (VTE) consists of the formation of a thrombus that completely or partially occluded the vessel light. Therefore, it comprises two related diseases: deep vein thrombosis (DVT) and pulmonary embolism (PE). These teeth, DVT is the most common (80-95% of cases) and PE is usually secondary to DVT; this is a serious and potentially lethal complication (SOCIEDADE BRASILEIRA DE ANGIOLOGIA E CIRURGIA VASCULAR, 2015). In Brazil, between 2008 and 2018, the number of hospitalizations related to venous thromboembolism exceeded 419,000, with a total of more than 10,000 deaths (MINISTÉRIO DA SAÚDE, 2018).
The conditions that favor VTE are: vascular endothelium injury, venous stesis and hypercoagulability states; virchow triad (YAMADA, 2015). Therefore, all pathologies and conditions that predispose VTE affect one or more elements of this triad. Among these, the main pathologies related to hospital care are: surgical procedures, mobility restriction, active infection, congestive heart failure, chronic kidney disease, decompensated diabetes mellitus, recent trauma, smoking, active cancer and previous VTE. Other physiological conditions also increase the risk of VTE, such as pregnancy, puerperium and advanced age (> 70 years) (COMPLEXO HOSPITALAR UNIVERSITÁRIO PROFESSOR EDGAR SANTOS, 2013).
The main complication of DVT is postthrombotic syndrome, characterized by pain, edema and skin changes in the affected limb. As for pulmonary embolism, the main complication is acute respiratory failure, leading to cardiac arrest and death (SOCIEDADE BRASILEIRA DE CIRURGIA VASCULAR, 2015).
Despite these scenarios, VTE is the main cause of preventable death within the hospital, however, many hospitals do not employ or inadequately employ prophylactic care (mechanical and pharmacological) in their wards (ALCKIMIN, 2013). The main obstacles to this are fear of side effects of medications, lack of protocols that standardize preventive practices and failure to adequately train professionals (FARHART, 2018).
The occurrence of a thromboembolic event leads to increased hospital stay, increased hospital costs and increased morbidity and mortality. In addition, therapeutic anticoagulation after VTE lasts at least 3 months, significantly increasing the adverse effects of the medication when compared to its prophylactic use (MAYNARD, 2016).
On the other hand, thromboprophylaxis in hospitalized at-risk patients reduces the chance of a thromboembolic event by 30% to 65% and, due to the shorter time of anticoagulation, has a lower chance of causing bleeding (RAYMUNDO, 2019). The use of elastic compression stockings, intermittent pneumatic compression, early ambulation and anticoagulation, when used appropriately in patients at risk for VTE, has been proven to be a positive cost-benefit ratio; reducing hospital stay, accelerating recovery and preventing deaths (KARLISCH, 2014).
Given its importance, evaluation models were created to track patients at high risk of developing a thromboembolic event. The main model used to elect those who will receive anticoagulation in clinical patients is the Padua Score. This score uses the identification of relevant risk factors and assigns a score to each of them, according to their degree of importance, patients who scored between 0-3 have low risk for VTE (0.3%) and patients who scored ≥ 4 have a high risk for VTE, about 11% (SOCIEDADE BENEFICENTE ISRAELITA BRASILEIRA ALBERT EINSTEIN, 2016).
Pharmacological prophylaxis should be instituted in high-risk patients by Padua score. The drugs administered are usually non-fractionated heparin, low molecular weight heparin (Enoxaparin being the most common). A care protocol for the application of these drugs in appropriate dose, time and route of administration was issued by the Hospital Israelita Albert Einstein (HIAE). In addition, the protocol also has guidance on non-pharmacological measures such as early mobilization, elastic compression and motor physiotherapy. This was elaborated following the recommendations of the 9th consensus of the American College of Chest Physicians (SOCIEDADE BENEFICENTE ISRAELITA BRASILEIRA ALBERT EINSTEIN, 2016).
In view of the above, the objective of the research is to analyze the coverage and adequate performance of prophylaxis for venous thromboembolism used in high-risk patients hospitalized in the clinical ward. As well as: identify their sociodemographic characteristics; the most frequent risk factors and calculate the prevalence of thrombosis in high-risk patients admitted to a clinical ward.
2. METHODS
This is a cross-sectional and retrospective study with a quantitative approach. The research scenario was a Medical Clinic ward of a tertiary public hospital in the state capital of Pará. The medical records of patients at high risk for thrombosis were included in the study, according to the Padua Score (set out in Table 1) and aged ≥ 18 years. Patients who had absolute contraindication to the use of anticoagulants were excluded from the study; patients diagnosed with VTE as the cause of hospitalization; medical records not available or with incomplete information and patients whose anticoagulation was the treatment of the underlying pathology, since the purpose of the study is to perform an analysis on prevention and not on the treatment of the disease.
Table 1 – Stratification of the risk of thrombosis by Padua score.
| Risk factor | Punctuation |
| Active cancer | 3 |
| History of previous VTE | 3 |
| Reduced mobility | 3 |
| Primary or secondary thrombophilia | 3 |
| Recent trauma (last month) | 2 |
| Advanced age (≥ 70 years) | 1 |
| Heart or respiratory failure | 1 |
| Rheumatologic infections or diseases | 1 |
| Previous acute myocardial infarction or stroke | 1 |
| Obesity (BMI ≥ 30) | 1 |
| Current hormone therapy | 1 |
|
Total score High Risk ≥ 4 Low Risk < 4 |
Source: Protocol of venous thromboembolism Sociedade Beneficente Israelita Brasileira Albert Einstein, 2016.
In the period analyzed (January 1, 2020 to March 31, 2020), the total number of medical records found were 207, among these 91 met the inclusion criteria. The analysis of numerical data was performed by descriptive statistics by the Microsoft Office Excel program and, the judgment to consider the prophylaxis method as adequate or inadequate, was made by comparison with the thromboprophylaxis protocol of the Brazilian Israeli Charity Society Albert Einstein provided in Table 2.
Table 2 – Thromboprophylaxis protocol according to risk of thrombosis of the Hospital Israelita Albert Einstein – adapted.
| Risk stratification | Thromboprophylaxis |
| Stratification by Padua score | |
| Low risk < 4 pontos | Early ambulation |
| High risk ≥ 4 points | Mechanical prophylaxis associated with: HNF 5,000 IU every 8 or 12 hours. HBPM 40mg, if creatinine clearence < 30, ajustar para 20mg em dose única diária. |
UFH: Non-fractionated heparin; LMWH: low molecular weight heparin.
Source: Protocol of venous thromboembolism Sociedade Beneficente Israelita Brasileira Albert Einstein, 2016.
The research commended the guidelines set out in Resolutions 196/96 and 466/12 of the National Health Council and the analysis of medical records was initiated after approval by the Ethics and Research Committee (CEP) of the hospital, in which the research was carried out. No terms of free and informed consent were applied, because the research was not performed directly with the patients, all personal information was preserved.
3. RESULTS
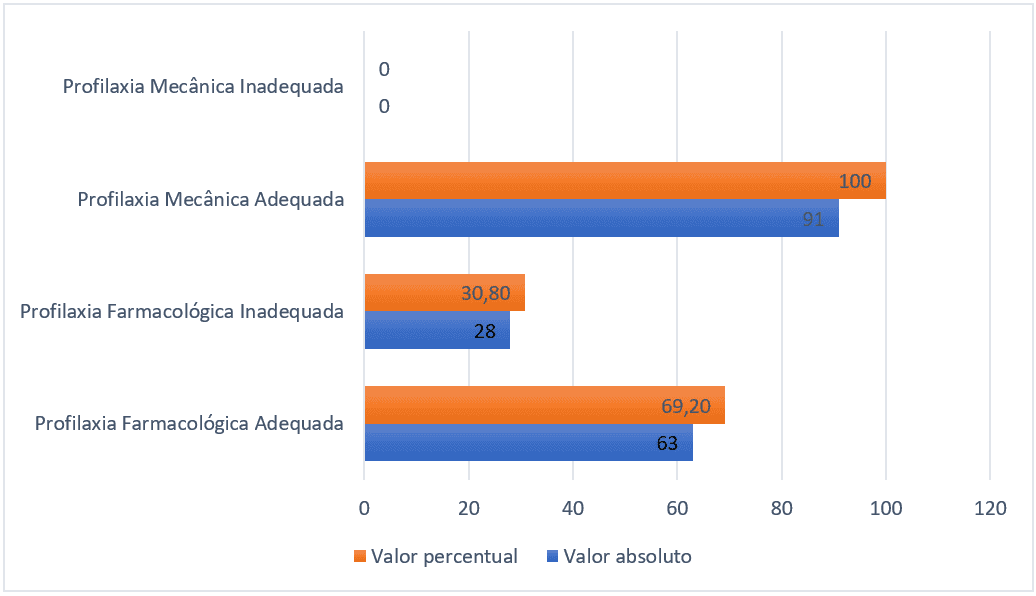
Among the 91 patients who should have received pharmacological prophylaxis, 28 (30.8%) did not receive or received it inadequately, that is, in a subtherapeutic dose or with drugs inadequate for the prevention of thromboembolism. Regarding mechanical prophylaxis, all 91 patients received some appropriate modality.
Figure 1 – Number of patients who received pharmacological and mechanical prophylaxis or not, Belém-PA, Brazil, 2021.
Regarding the sociodemographic characteristics, 43 (47%) were women and 48 (53%) were men. The age distribution of adults between 18-59 totaled 47 (51%), the elderly aged between 60-79 years totaled 35 (38%) and the group of very elderly totaled 9 (11%), and the mean age in years was 57 with standard deviation of 17 points. The mean number of days of hospitalization was 25 with a standard deviation of 20 points.
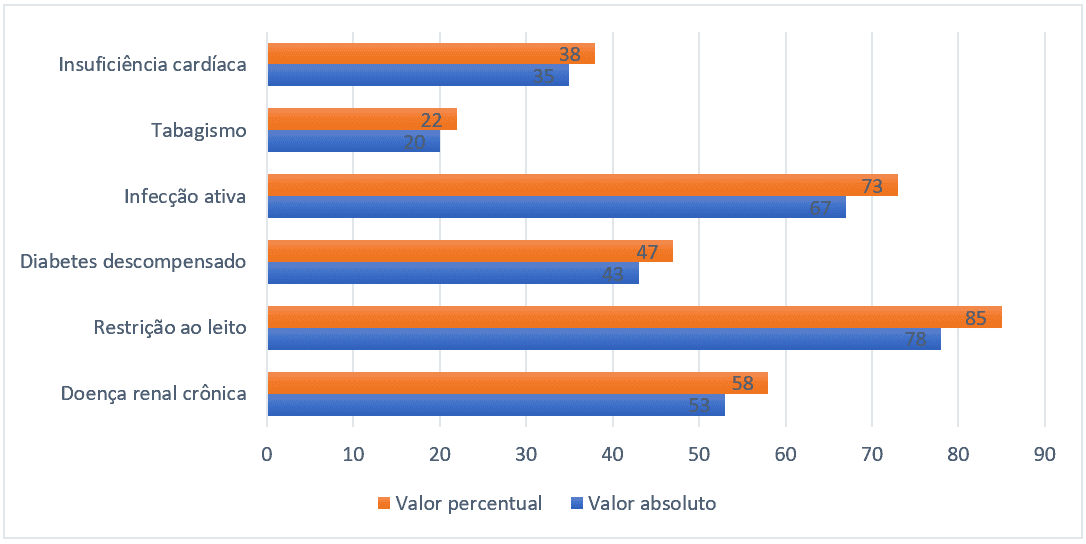
Regarding the epidemiological profile, the most prevalent risk factors were bed restriction (85%), active infection (73%), chronic kidney disease (58%), heart failure (38%) and smoking (22%). Only the relevant risk factors regarding the predisposition of VTE were reported and that met in some way criteria for the Padua score.
Figure 2 – Risk factors more prevalent in hospitalized patients, Belém-PA, Brazil, 2021.
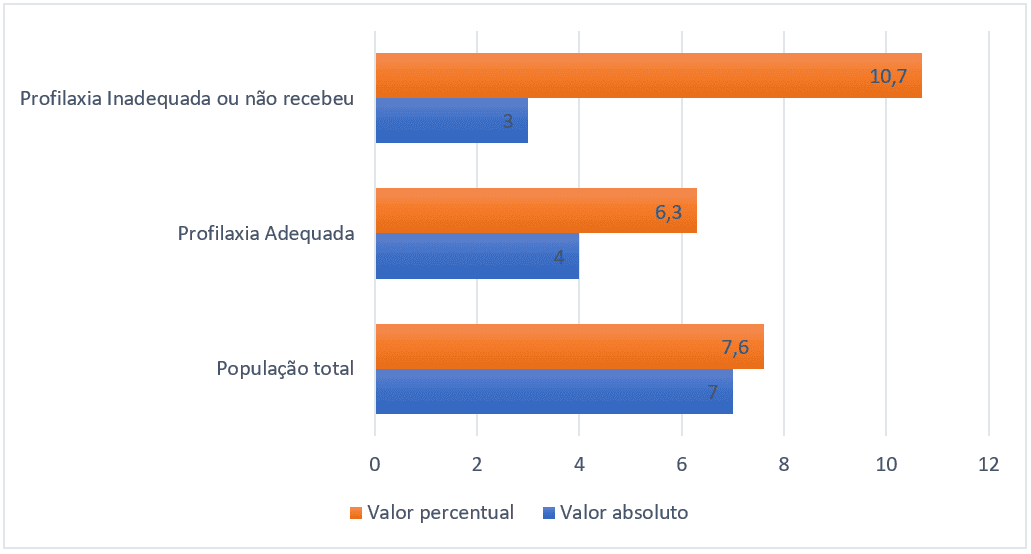
The total prevalence of thromboembolic events was 7.6% (7 in the sample universe of 91). The group of patients who received adequate pharmacological prophylaxis had a prevalence of 6.3% (4 patients of 63), while the group that did not receive pharmacological prophylaxis or received it inadequately had a prevalence of 10.7% (3 patients of 28), the graph below explains the percentage relationships and absolute number of events.
Figure 3 – Prevalence of thromboembolic events of each group, Belém-Pa, Brazil, 2021.
4. DISCUSSION
A significant number of medical records submitted to analysis was compromised by lack of data or illegibility. The hospital uses a system of manually filled-out medical records. This makes it difficult to acquire data clearly both for conducting research, as well as to continue the care of the multidisciplinary team itself. The implementation of electronic medical records, despite a high initial investment, has proven cost-effective and can be used as a valuable ally in the implementation of strategies for the prevention of VTE and other injuries (PATRÍCIO, 2011).
Insufficient use of prophylaxis for thromboembolism is a worldwide phenomenon. The ENDORSE study, which evaluated the use of adequate prophylaxis in 358 hospitals in 32 countries, concluded that only half of these patients received adequate prevention. Therefore, under-use of Prevention for VTE is a global problem. In Latin American countries, the correct utilization rate was 47% (LOPES, 2017). Studies of other services in Brazil have found discrepant proportions among themselves. Busato (2014) found 74% of adhering to correct prophylaxis in clinical patients, while Andrade (2008) found 26% in hospitals in the capital of Amazonas.
In the hospital analyzed, the appropriate use of pharmacological prophylaxis was 70%, while some type of mechanical prophylaxis was used in all patients. Although higher than the global average and the national average of the studies consulted, this adequacy rate is still far below the expected 95%, stipulated by the VTE safety zone program, which aims to transform hospitals into VTE-free zones. This is a global continuing medical education program for the implementation and optimization of VTE prevention in the hospital environment (ROCHA, 2020).
In a general survey, a laboratory that promotes the program in Brazil made contact with hospitals in all regions to evaluate how VTE prevention was performed. Among the results, the main factors that hindered prophylaxis were: the lack of a clear and accessible protocol for the prevention of VTE, lack of adhering to the completion of the protocol by physicians and mandatory risk assessment for VTE only in specific hospital wards (ROCHA, 2020).
Strategies suggested by both the Safety Zone VTE programand Leal (2020), which evaluated the scenario before and after the implementation of a VTE prophylaxis protocol in a hospital, concluded that the use of multimodal strategies has a significant impact on the support of preventive actions. Among the suggested methods are: mandatory completion and annexation of the prophylaxis protocol in the medical records of hospitalized patients; risk stratification for VTE in all hospitalized patients; the installation of automatic blocking of the electronic medical records if the protocol has not been completed, the development of simplified flowcharts for clinical practice and the continuing education of professionals on the subject.
It is important to highlight the effort of the multidisciplinary team regarding the appropriate use of mechanical prophylaxis, although this alone is insufficient in high-risk patients without contraindication to anticoagulation. The use of mechanical prophylaxis is cost-effective and easy to apply and has proven to be a valuable strategy to combat thromboembolism (PEREIRA, 2020).
The absolute value and percentage of men and women was very similar and there was no relevance when submitted to the analysis of prophylaxis coverage for thrombosis. The age group, in turn, has an average of 57 years, but with great variation in age (standard deviation of 17 years). This occurred due to the presence of extremes of age among hospitalized patients, making the calculation of the mean less accurate. Finally, the mean number of days of hospitalization was 25 days with a standard deviation of 20 days; the calculation was also impaired due to the presence of extremes, ranging from periods such as 5 days up to 100 days.
Despite the great variability, an average of 20 days of hospitalization is an important aggravating factor when assessing the risk of VTE. A long hospital stay is not synonymous with poor care provided, since the study was conducted in a tertiary hospital of the SUS network, implying a profile of more severe patients. However, prolonged hospitalization time is associated with an increase in the rate of hospital infection, increased morbidity and mortality and increased costs for the hospital (SILVA, 2014).
In the sample studied, 85% of the patients had infection during their stay, creating a feedback loop: permanence increases the chance of infection, which increases the length of stay. Following the morbid sequence, the infection increases the risk of VTE, which again increases the hospitalization time (SILVA, 2014).
The absolute prevalence of thromboembolic events was 7.6%. Nevertheless, the group of patients who received adequate pharmacological prophylaxis had a prevalence of 6.3%, while the group that did not receive pharmacological prophylaxis or received it inadequately had a prevalence of 10.7%. That is, despite a relatively low absolute prevalence, when compared to the 11.3% to 32.9% found in the literature (CHARLO, 2020) and a study population that did not reach a large scale, the group that did not receive adequate prophylaxis had a significant increase in the risk.
However, this prevalence is questioned, because according to Carneiro (2010), in most hospitals the prevalence of thrombosis is underestimated, since almost 50% of cases are subclinical. Moreover, for a reliable diagnosis of thrombosis it is almost always necessary to use complementary tests, and within the medical records analyzed it was not always clear how the diagnosis was reached. Thus, having only clinical evaluation without systematic search for thrombosis in patients at risk results in underdiagnosis.
The profile of the risk factors of the patients studied is consistent with that reported in the literature, but a particularity of the hospital was the number of nephropaths that required dose adjustment. Despite creatinine clearence not always described, the fit was considered adequate in this group of patients. Another important relationship is that the higher the number of risk factors, the lower the chance of the patient receiving adequate prophylaxis. Although there is fear of the risk of bleeding, since the contraindications are respected there is no support in the literature to adopt this conduct. On the contrary, patients with many risk factors thrombosam more and have their morbidity and mortality increased when compared to those not properly anticoagulated (CARNEIRO, 2010).
5. CONCLUSION
Therefore, it is observed that adequate prophylaxis for VTE was underutilized, following global and national trends, strategies such as: the formulation of a clear protocol for the prevention of VTE – whose completion was mandatory – and which was attached to medical records; use of electronic medical records and continuing education of health professionals are valuable strategies to increase adequate VTE prophylaxis coverage, mitigating hospitalization time, avoidable deaths and costs to the health system
REFERENCES
ALCKMIN, Carolina. Venous thromboembolism risk assessment in hospitalized patients: A new proposal. Clinics, São Paulo, v.68, n.11, p.1416-1420, nov. 2013. Disponível em:( http://www.scielo.br/scielo.php?script=sci_arttext&pid=S180759322013001101416&lng=pt&nrm=iso). Acesso em: 24/02/2019.
ANDRADE, Edson de Oliveira. Fatores de risco e profilaxia para tromboembolismo venoso em hospitais da cidade de Manaus. J. bras. pneumol., São Paulo, v. 35, n. 2, p. 114-121, Fev. 2009. Disponível em: ( http://www.scielo.br/scielo.php?script=sci_arttext&pid=S180637132009000200003&lng=en&nrm=iso). Acesso em: 30/11/2020.
BUSATO, Cesar Roberto. Avaliação de tromboprofilaxia em hospital geral de médio porte. J Vasc Bras., v. 13, n. 1, p. 5-11. Jan.-Mar 2014. Disponível em: (https://www.scielo.br/pdf/jvb/v13n1/pt_1677-5449-jvb-13-01-00005.pdf) Acesso em: 30/11/2020.
CARNEIRO, João Luiz de Aquino. Avaliação da profilaxia do tromboembolismo venoso em hospital de grande porte. Rev. Col. Bras. Cir., Rio de Janeiro, v. 37, n. 3, p. 204-210, Jun. 2010. Disponível em: ( http://www.scielo.br/scielo.php?script=sci_arttext&pid=S010069912010000300008&lng=en&nrm=iso). Acesso em: 30/11/2020.
CHARLO, Patricia Bossolani. Relação entre trombose venosa profunda e seus fatores de risco na população feminina. Glob Acad Nurs, Maringá-Paraná. V.1, n. 1, p. 1-7, 2020. Disponívelem:(http://globalacademicnursing.com/index.php/globacadnurs/article/download/35/19). Acesso em: 30/11/2020.
COMPLEXO HOSPITALAR UNIVERSITÁRIO PROFESSOR EDGARD SANTOS. Prevenção de Fenômenos Tromboembólicos Venosos em Pacientes Internados. Salvador, v.1, n.1, p. 4-12, jan. 2013. Disponível em: (http://www2.ebserh.gov.br/documents/1975526/2520527/diretriz_1_prevencao_de_fenomenos_tromboembolicos_venosos_em_pacientes_internados_revisada.pdf/0a924d80-6b7b-430a-b75c-2bd11211a1b9). Acesso em: 24/02/2019.
FARHAT, Fátima. Avaliação da profilaxia da trombose venosa profunda em um hospital geral. J. vasc. bras., Porto Alegre, v. 17, n. 3, p. 184-192, set. 2018. Disponível em (http://www.scielo.br/scielo.php?script=sci_arttext&pid=S167754492018000300184&lng=pt&nrm=iso). Acesso em: 24/02/2019.
KALISCH, Beatrice. Outcomes of inpatient mobilization: a literature review. J Clin Nurs. 2014 Jun;23(11-12):1486-501. doi: 10.1111/jocn.12315. Epub 2013 Sep 13. PMID: 24028657. Disponível em: (https://www.ncbi.nlm.nih.gov/pubmed/24028657). Acesso em: 24/02/2019.
LOPES, Bruno Abdala Candido. Sabemos prescrever profilaxia de tromboembolismo venoso nos pacientes internados? J Vasc Bras. V. 16, n. 3, p.199-204, Jul-Set. 2017. Disponível em: (https://www.ncbi.nlm.nih.gov/pubmed/29930647/) Acesso em? 30/11/2020.
LEAL, Lisiane Freitas. Implementação de protocolo para profilaxia de tromboembolismo venoso: um estudo antes e depois em pacientes clínicos e cirúrgicos. J. bras. pneumol., São Paulo, v. 46, n. 4, p. 1-7, 2020. Disponível em: ( http://www.scielo.br/scielo.php?script=sci_arttext&pid=S180637132020000400200&lng=en&nrm=iso). Acesso em: 30/11/2020.
MINISTÉRIO DA SAÚDE. Banco de dados do Sistema Único de Saúde-DATASUS. Internações por Região segundo Região Lista Morb CID-10: Flebite tromboflebite embolia e trombose venosa Período: Jan/2008-Nov/2018. Disponível em (http://www.datasus.gov.br). Acesso em: 02/03/2019.
MINISTÉRIO DA SAÚDE. Banco de dados do Sistema Único de Saúde-DATASUS. Óbitos por Região segundo Região/Unidade da Federação
Lista Morb CID-10: Flebite tromboflebite embolia e trombose venosa
Período: 2008-2018. Disponível em (http://www.datasus.gov.br). Acesso em: 02/03/2019.
MAYNARD, Greg. Preventing hospital-associated venous thromboembolism: a guide for effective quality improvement. Agency for Healthcare Research and Quality, US Department of Health and Human Services, 2016. Disponível em: (https://www.ahrq.gov/sites/default/files/publications/files/vteguide.pdf). Acesso em: 24/02/2019.
PATRÍCIO, Camila Mendes. O prontuário eletrônico do paciente no sistema de saúde brasileiro: uma realidade para os médicos? Scientia Medica (Porto Alegre), volume 21, número 3, p. 121-131, maio 2011. Disponível em: (https://revistaseletronicas.pucrs.br/ojs/index.php/scientiamedica/article/viewFile/8723/6722). Acesso em: 30/11/2020.
PEREIRA, Nikacia Torres. A frequência do uso de profilaxia mecânica em pacientes com trombose venosa profunda: uma revisão integrativa de literatura. Trabalho de Conclusão de Curso (Bacharelado em Fisioterapia) – Curso de Fisioterapia, Centro Universitário CESMAC, Maceió, 2018. V. 1, p. 1-19, 2020. Disponível em: (https://ri.cesmac.edu.br/handle/tede/677). Acesso em: 30/11/2020.
RAYMUNDO, Selma Regina. O que mudou nas últimas décadas na profilaxia do tromboembolismo venoso em pacientes internados: artigo de revisão. J. vasc., Porto Alegre, v. 18, fev. 2019. Disponível em: (http://www.scielo.br/scielo.php?script=sci_arttext&pid=S167754492019000100402&lng=en&nrm=iso&tlng=en). Acesso em: 25/02/2019.
ROCHA, Ana Thereza Cavalcanti. Protocolos de profilaxia de tromboembolismo venoso (TEV) em hospitais brasileiros – PROTEV Brasil. J. vasc. bras., Porto Alegre, v. 19, p. 1-7, jan. 2020. Disponível em: (http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1677-54492020000100314&lng=en&nrm=iso). Acesso em 30/11/2020.
SILVA, Ana Maria Nunes. Fatores que contribuem para o tempo de internação prolongada no ambiente hospitalar. J. res.: fundam. care. online. v. 6, n. 4, p. 1590-1600, out./dez 2014. Disponível em: (http://www.redalyc.org/pdf/5057/505750770023.pdf). Acesso em: 30/11/2020.
SOCIEDADE BENEFICENTE ISRAELITA BRASILEIRA ALBERT EINSTEIN. Protocolo de Profilaxia de Tromboembolismo Venoso, 2016. Disponível em:(http://pubdiretrizes.einstein.br/download.aspx?ID={CD7022C363284063930B3D3E68D5F967}). Acesso em: 25/02/2019.
SOCIEDADE BRASILEIRA DE ANGIOLOIG A E CIRURGIA VASCULAR. Trombose venosa profunda diagnóstico e tratamento, 2015. Disponível em: http://www.sbacv.org.br/lib/media/pdf/diretrizes/trombose-venosa-profunda.pdf. Acesso em: 24 /02/ 2019.
YAMADA, Norikazu. Occurrence of deep vein thrombosis among hospitalized non-surgical Japanese patients, junho 2015. Disponível em: (https://www.ncbi.nlm.nih.gov/pubmed/26421068). Acesso em: 25 /02/ 2019.
[1] Student of the faculty of medicine of the State University of Pará.
[2] Student of the medical school of the State University of Pará.
[3] Master in Health, Environment and Society in the Amazon by PPGSAS/UFPA.
[4] Master in Surgery and Experimental Research – CIPE from the State University of Pará. PhD student in the Virology program – PPGV of the Evandro Chagas Institute. Effective Professor of the Faculty of Medicine of the State University of Pará in the axes Of Interaction Management and Community Education (GIESC) and Scientific Research 1 (PC1).
Submitted: March, 2021.
Approved: April, 2021.















