ORIGINAL ARTICLE
PEREIRA, Holda Maria de Jesus [1], OLIVEIRA, Tatiane Alves Cortez de [2], ALMEIDA, Leandro Augusto [3]
PEREIRA, Holda Maria de Jesus. OLIVEIRA, Tatiane Alves Cortez de. ALMEIDA, Leandro Augusto. Physiotherapy management to patients with COVID-19 in intensive care units. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year 06, Ed. 01, Vol. 01, pp. 123-138. January 2021. ISSN: 2448-0959, Access link: https://www.nucleodoconhecimento.com.br/health/physiotherapy-management
ABSTRACT
Coronavirus (SARS-COV-2) has infected many people in Brazil and worldwide. The disease showed importance of the physiotherapy professional being up to date and having knowledge of the techniques and resources for the correct management of patients within the Intensive Care Unit. The general objective of this study was to delineate physical therapy care to patients with COVID-19 in the intensive care unit. This is a bibliographic review, based on the analysis of scientific articles published in 2020. Data were searched from March to September 2020, where articles were selected in accordance with the proposed theme, and a bibliographic survey was carried out in the databases: Scientific Electronic Library Online (SciELO), Latin American Literature in Health Science (LILACS), Google Academic, Physiotherapy Evidence Database (PEDro) and PubMed. Although a large part of the infected population has only mild symptoms, some may have a more severe form of the disease and hospitalization in a clinical bed or even in the Intensive Care Unit is necessary, as some cases of patients with COVID-19 may progress to different levels of disease severity, which may lead to acute respiratory failure (AKI), acute respiratory distress syndrome (ARDS), or even multiple organ failure. Thus, it is concluded that physical therapy care is extremely important for the patient, both at admission and during the entire time of hospitalization in the intensive care unit.
Keywords: COVID-19, Acute Respiratory Distress Syndrome, Intensive Care Unit, Physiotherapy, Coronavirus.
INTRODUCTION
In December 2019, a new epidemic arose in the city of Wuhan and spread throughout China. It was initially pneumonia of unknown etiological origin and that through genetic sequencing was classified as a new genus beta coronavirus, the same being defined as new pneumonia by the World Health Organization (WHO) (SILVA et al., 2020).
Symptoms are similar to those of a common flu, however, patients with this pathology may need intensive care (MATOS and SCHAPER, 2020). According to a study by the Center for Diseases Control and Prevention of the United States, based on data from China, the mortality rate is higher in the elderly, especially those with some underlying disease (IMOTO et al., 2020).
Although most patients present mild symptoms such as fever, dry cough and sore throat, some have evolved into major complications, such as organ failure, pulmonary edema, septic shock, severe pneumonia and Acute Respiratory Distress Syndrome (ARDS) (SOHRABI et al., 2020).Second (SILVA et al., 2020) the impairments of this virus go beyond the respiratory system, also aggravating other systems, such as cardiovascular, causing a decompensation of this system, especially in patients with coronary artery disease and heart failure.
Transmission of the virus occurs mainly through the airways, through inhalation of droplets, eliminated by sneezing or coughing, during procedures such as noninvasive ventilation (NIV), intubation and extubation, aspiration, cardiopulmonary resuscitation, and bronchoscopy (FRESCA et al., 2020).
Given the high rate of infected people, the rapid spread of the virus and the significant number of people who need care in an UTI, the problem established in this review is: how can physical therapy provide quality care to these patients?For among the various professionals who work to promote the recovery of patients with COVID-19, the physiotherapist stands out. Its attributions aim to prevent and rehabilitate respiratory problems and functional limitations of daily life activities (ADLs) caused by it (SILVA et al., 2020).
Respiratory physiotherapy in wards and intensive care unit (UTI) may be indicated for patients with suspected or confirmed cases who jointly or later develop hypersecretion, exudative pulmonary consolidations and/or difficulty in removing airway secretions (MATOS, 2020).
The need for invasive mechanical intubation and ventilation (IMV) is usually necessary, as some patients fail oxygen therapy and noninvasive ventilation (NIV) or already have direct indication of MV and need to be quickly intubated (SILVA et al., 2020).
This is a bibliographic review, based on the analysis of scientific articles published in 2020. Data collection was performed from March to July 2020, selecting articles in accordance with the proposed subject, through bibliographic survey in the electronic databases Scientific Electronic Library Online (SciELO), Latin American Literature in Health Science (LILACS), Google Scholar, Physiotherapy Evidence Database (PEDro) and PubMed. The Health Sciences Descriptors (DCS) used will be COVID-19, acute respiratory distress syndrome, intensive care unit, physiotherapy and mechanical ventilation and its correreports in the English language acute respiratory distress syndrome, intensive care unit, physiotherapy and mechanical ventilation. The inclusion criteria determined will be articles in Portuguese and English related to the theme and published this year.
DEVELOPMENT
COVID-19 HISTORICAL PROFILE
The current pandemic caused by coronavirus 2019 (SARS CoV-2) has caused serious damage to health systems in Brazil and worldwide (PINTO and CARVALHO, 2020). The World Health Organization (WHO) declared on March 11, 2020, that the outbreak was a pandemic. The first confirmed case in Brazil was on February 25, 2020, with a continuous increase in people affected in several Brazilian states (GUIMARÃES, 2020).
The rapid spread of the virus worldwide and the increasing number of cases led health systems to collapse due to insufficient number of health professionals, lack of beds in intensive care units (UTI) to meet the increased demand and lack of mechanical ventilators (WITTMER et al., 2020).
While the world struggles to control the advance of the disease, a great strain to accommodate the growing number of patients have affected cities. This has made extreme measures be taken to alleviate the bed crisis and the lack of professionals in hospitals (YEO et al., 2020).
This pandemic showed how a very infectious virus is capable of overloading health systems even in economically developed countries, being one of the main aggravating factors for this to occur the lack of beds in UTIs and the lack of resources for the treatment of patients on mechanical ventilation (SEVERIN et al., 2020).
ROLE OF PHYSIOTHERAPIST IN COVID-19
In view of the crisis that has taken place in the world due to the advance of the new coronavirus, it has highlighted the importance of the multidisciplinary health team, among which we can emphasize the importance of the physiotherapist’s action on the front line of care for patients suspected of infection or even contaminated by SARSCoV-2 (COSTA and LOIOLA, 2020).
Because it is a new disease where there was not enough time for clinical studies and systematic reviews that could direct interventions, treatment has been made from the experience of countries that have faced or are still facing a number of high cases, as well as in studies on Acute Respiratory Distress Syndrome (ARDS), Severe Acute Respiratory Syndrome (caused by coronavirus SARS-CoV) and Middle Eastern Respiratory Syndrome (caused by the CORONAVirus MERS-CoV) (GUIMARÃES , 2020).
Knowing the signs and symptoms is a decisive condition for the choice of physical therapy techniques and resources to be used, however, care should be planned and adequate according to the available ecosystem conditions, considering that there is a great risk of virus dissipation (FURLANETTO et al., 2020).
Studies already published on the role of the physiotherapist in the context of this pathology address the importance of this professional being up-to-date and possessing the necessary competence to provide quality care in the various levels of severity of the patient, in the management of invasive and noninvasive mechanical ventilation, during oxygen therapy, in the techniques for attenuating the generation of aerosols, in the care of hypersecretory patients , to patients with impaired respiratory system or dyspnea, among other comorbidities.
Although some publications direct the care to patients with more severe health status, not indicating physical therapy if the patient with COVID-19 presents mild symptoms in which there is no expressive impairment of the respiratory system, currently physical therapy care has become indispensable during the hospitalization process, acting in the prevention and treatment of respiratory disorders resulting from secretion retention and atelectasis , as well as in the preservation of muscle strength and functionality in the time of hospitalization, assisting in intubation, mechanical ventilator adjustments – programming the initial ventilatory parameters – in the monitoring of respiratory mechanics, weaning from mechanical ventilation (MV) and during extubation.
Therefore, it is recommended the performance of expert professionals and/or with experience, titration and/or dedicated training in Intensive Care and/or Respiratory Physiotherapy, in addition to knowledge of the available resources (MUSUMECI et al., 2020). For just as pulmonary changes require significant attention, the effects of the time elapsed from immobility in bed in the same way. Therefore, exercises should be included as early as possible, whether passive, active-assisted, active exercises, electrostimulation, bed positioning, breathing exercises, with the intention of reducing as much as possible the loss of the patient’s functional capacity and a better recovery of quality of life after infection (MATTE et al, 2020).
It is expected that some results can be achieved, including:
- Reduction in the number of intubations;
- Reduction in UTI and MV stay time;
- Reduction in the number of respiratory infections;
- Reduction in the mortality rate over the hospitalization period after hospital discharge.
During treatment, there is a possible risk of aerial transmission of the virus causing COVID-19, because some techniques used to improve respiratory dysfunctions are large aerosol generators, which we can highlight manual hyperinflation, respiratory muscle training and NIV. Therefore, it is necessary to carefully evaluate the recommendation and use of these resources, where there is a higher risk of contamination (MUSUMECI et al., 2020).
In relation to the techniques used by the physiotherapist, another concern is focused on increasing excessive energy expenditure, especially in patients in severe condition. Because this situation caused by active mobilizations or even physical exercise can aggravate respiratory muscles and generate a respiratory arrest (FURLANETTO, 2020).
NONINVASIVE VENTILATION
According to some publications, the use of NIV is not recommended as a first-line ventilatory strategy, due to the high percentage of failure and the increase in viral dissemination resulting from the generation of aerosols in the environment caused by some techniques such as hyperinflation with manual resuscitator and the use of the high-flow nasal cannula (CNAF). However, in some cases, defined by the multidisciplinary team, a NIV response test can be performed for 30 minutes, provided that the patient has a peripheral oxygen saturation (SPO2) <93% no cateter nasal a 5l/min (MARTINEZ et al., 2020).
The test can be performed as long as there are ideal circumstances for its execution, such as the use of mask without exexation valve coupled to ventilatory circuits with double branch, as well as the correct use of heat and humidity exchanger filters, similar to the standard used in the MV of filters and passive humidification devices and personal protective equipment (EPIs) (MARTINEZ et al. , 2020).
In cases where NIV use is indicated, the patient should be monitored carefully, and if there is no improvement in clinical patterns it is necessary to alert the team to the indication of IMV, because the delay in intubation due to the time-consuming use of NIV may be related to a high mortality rate, especially in more severe patients (MUSUMECI et al. , 2020).
As previously seen, there are authors in their publications who do not recommend the use of NIV or high-flow nasal cannula (HFNC). However, some experiments conducted in China recommend the use of NIV and HFNC early, may generate a lower mortality rate and decrease in cases of intubation (WINCK and AMBROSINO, 2020).
Despite the uncertainties and lack of scientific evidence, the positive results in most observational studies already suggest that in a safe environment, such as a negative pressure room, with patients carefully evaluated and without any indication of IMV, the use of NIV can be considered (GÓMEZ et al., 2020).
Thus, the use of NIV as a treatment should be a resource to be used provided that there is careful monitoring to verify if there is a risk of failure or if it is necessary to make the change to an IMV.
MECHANICAL VENTILATION
It is important to observe signs of hypoxemic respiratory failure, as increased respiratory work and low blood oxygen levels can gradually worsen, despite the use of conventional oxygen therapy and endotracheal intubation should be performed as soon as possible (BLANCO and DUDARYK, 2020). The health team should make use of EPIs (personal protective equipment) such as gloves, bonnet, cap, protective mask (N95/ PFF2), as well as glasses or face protector. Moreover, patients with severe respiratory failure who require elevated ventilatory support, as they can progress rapidly from spontaneous ventilation to the need for intubation and mechanical ventilation, which can last for up to 3 weeks. (GUIMARÃES, 2020).
During IMV, a protective ventilation strategy should be proposed in order to reduce the risk of lung injury caused by ventilation, so it is recommended to:
- Volume-controlled ventilatory mode (VCV) or pressure (PCV);
- Maintenance of distension pressure (driving pressure) less than 15 cmH2O;
- Individually perform the adjustment of the final expiratory positive pressure (PEEP);
- Tolerate permissive hypercapnia;
- A respiratory rate close to the ideal of 20 irpm.
- Schedule a FiO2 from 92 to 96% (REIS, 2020).
Studies have shown that the use of high volume and pressure parameters may be factors causing pulmonary injury and are related to a higher number of deaths. Therefore, patients presenting with a clinical picture of ARDS should be prioritized a protective ventilatory strategy (FURLANETTO, 2020).
DESMAME AND EXTUBATION
The patient’s extubation process involves the gradual transition from artificial ventilation to spontaneous ventilation, performed with patients on invasive mechanical ventilation for more than 24 hours. Therefore, a spontaneous ventilation test is performed with the aid of an endotracheal tube that allows the patient to ventilate by itself. Patients with satisfactory test results should be analyzed for indication of patient withdrawal from the mechanical ventilator (BRANCO and ARRUDA, 2020). The World Health Organization recommends the use of weaning protocols where spontaneous breathing allows spontaneous breathing to be evaluated daily, whenever the patient’s clinical picture allows. For the weaning process to occur, the following conditions must be considered (CASTRO et al., 2020):
- Level of consciousness (Glasgow Coma scale > 8).
- Adequate oxygenation: PaO2 > 60mmHg with FiO2 < 0,40 e Peep < 10.
- Absence of hypersecretion (more than 1 aspiration every 2 hours).
- Hemodynamic stability: mean blood pressure > 60 mmHg without the need for vasopressors (or in low doses).
- Airway protection capability: peak expiratory flow > 60 L/min.
- Do not present suspected airway edema.
In the event of weaning failure, it is important to investigate what led to the failure. Evaluate the general picture of the patient, hemodynamic stability, signs of ventilatory effort, if necessary to perform further evaluations. Before a new weaning attempt it is recommended to wait 24 hours (CASTRO et al., 2020).
PRONA POSITION
As some patients have rapidly impaired lung function causing severe hypoxemia and serious changes in gas exchange, immediate treatment is required. Thus, many care units began to treat patients in the prona position, and in some cases, oxygenation levels increased significantly. Although not all showed an improvement, there are reports of patients with COVID-19 who were treated in the prono and obtained good results in treatment. Therefore, many centers began to offer early pronation as an alternative for patients with spontaneous breathing, even before intubation and mechanical ventilation (LINDAHL, 2020).
The prona position is one of the therapeutic resources that stands out in the treatment of patients with ARDS. The method consists of pouring the patient into ventral decubitus, with the objective of distributing tension and stress on the lungs more evenly, improving the ventilation/perfusion ratio, improving pulmonary mechanics so that mv time and mortality rate decrease. It is important that pronation is introduced as soon as possible preferably within the first 24 hours, or within 48 hours, in patients with severely impaired gas exchange and in case of ARDS. It is indicated that the patient remains in this position for at least 16 hours and can reach up to 20 hours, before positioning him again in a supine position (supine position) (BORGES et al., 2020).
One of the key factors for positioning execution to occur smoothly and safely, with a higher probability of success is having a trained and experienced team. Therefore, it should be considered that units that performs the pronation, offer courses and training to the entire team that performs the maneuver. (BORGES et al., 2020).
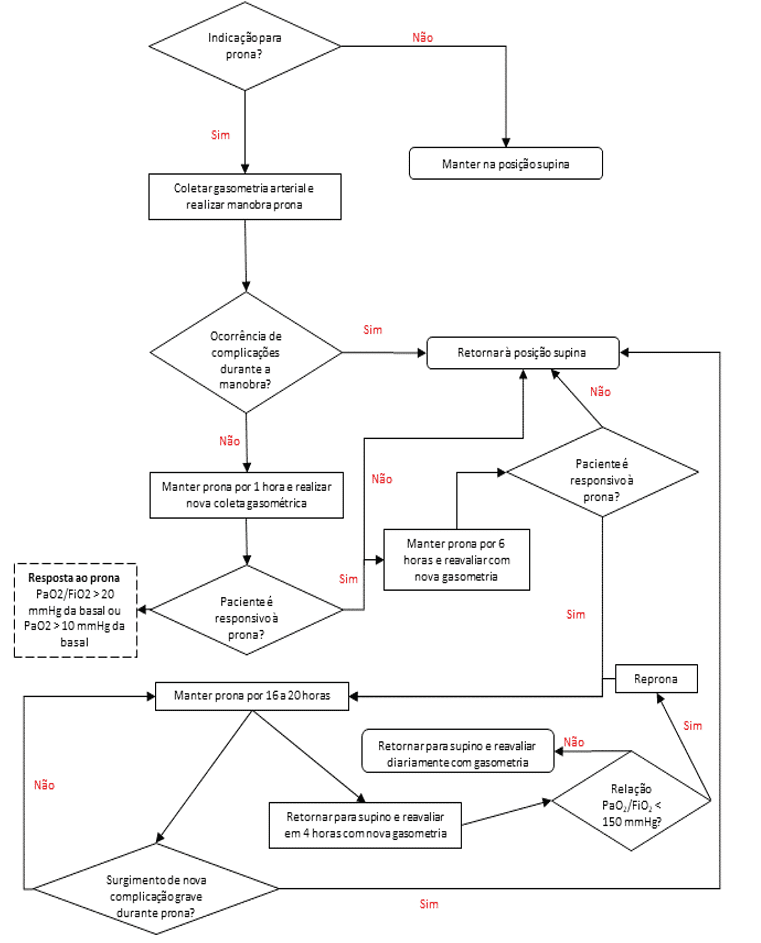
Some factors are analyzed to see if the response to the prona position is being satisfactory or not. An arterial blood gas analysis should be done 1 hour after pronation, to consider whether or not the patient is responding to the technique used. Positioning should be maintained if the patient has a good response, i.e., if he/she has a 20 mmHg increase in PaO2/FiO2 or 10mmHg in PaO2, remembering that some patients may respond to the process more slowly and may take up to 6 hours to show a favorable response. After 6 hours a new evaluation should be performed, if the result is adequate, if the prono for 16 to 20 hours, otherwise it happens and the patient does not present a good response after the new evaluation, the patient returns to the supine position. Monitoring should be constant, and it is suggested that a new evaluation occurs every 6 hours (BORGES et al., 2020).
Figure 1: Technique is recommended by the World Health Organization (WHO).

Figure 2: Protocol flowchart for head position.
FINAL CONSIDERATIONS
Since COVID-19 is a new disease and the evidence on the subject to date is still reduced, this literature review covers some of the physiotherapist’s duties in an intensive care unit, acting in the prevention and treatment of respiratory disorders; in the maintenance of muscle strength (which may be impaired due to the prolonged period of bed rest) with passive, active-assisted, active, mobilization exercises; using NIV as one of the resources for treating patients with COVID-19, always maintaining careful monitoring of this patient; assisting in intubation; in the adjustments of the mechanical ventilator – programming the initial ventilatory parameters and seeking to offer a protective ventilation in order to reduce the risk of a lung injury – in the monitoring of respiratory mechanics; weaning from mechanical ventilation (MV) and during extubation; and the benefits of the prona position to the patient.
It is also worth noting the importance of the physiotherapist being trained, trained and updated regarding the methods used as a form of treatment.
REFERENCES
BORGES, D. L.; RAPELLO, G. V. G.; DEPONTI, G. N.; et al.. Prone position in the treatment of acute respiratory failure due to COVID-19. ASSOBRAFIR Ciência; Agosto 2020. DOI: https://doi.org/10.47066/2177-9333.AC20.covid19.011
BRANCO, A. B. A.C.; ARRUDA, K. D. S. A.; Atendimento psicológico de pacientes com COVID-19 em desmame ventilatório: proposta de protocolo. Revista Augustus; v. 25 n. 51; 2020. DOI: https://doi.org/10.15202/1981896.2020v25n51p335.
CASTRO, L. A.; RONCALLI, A.; CAMILLO, C. A. Desmame da ventilação mecânica na COVID-19. ASSOBRAFIR; Junho 2020.
CORRÊA, T. D.; MATOS, G. F. J.; BRAVIM, B.A.; et al..Intensive support recommendations for critically-ill patients with suspected or confirmed COVID-19 infection. Einstein (São Paulo). 2020 May 29.
FRESCA et al. Recomendações relacionadas ao fluxo de atendimento para pacientes com suspeita ou infecção confirmada pelo COVID-19 em procedimentos cirúrgicos ou endoscópicos. SOBECC Março 2020.
FURLANETTO, K. C.; HERNANDES, N. A.; MESQUITA, R. B.. Recursos e técnicas fisioterapêuticas que devem ser utilizadas com cautela em pacientes com COVID-19. ASSOBRAFIR; Abril 2020.
GATTINONI, L.; CHIUMELLO, D.; CAIRONI, P.; et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes. Intensive Care Med 46, 1099–1102 (2020). DOI: https://doi.org/10.1007/s00134-020-06033-2.
GÓMEZ, C. C.; RODRÍGUEZ, Ó. P.; TORNÉ, M. L.; et al.. Clinical consensus recommendations regarding non-invasive respiratory support in the adult Patient with acute respiratory failure secondary to SARS-CoV-2 infection. Arch Bronconeumol. Julho de 2020; 56: 11-18.
GUIMARÃES, F. Approach of the physiotherapist in intensive care units in the context of the COVID-19 pandemic. Fisioter. Mov., Curitiba, v. 33, e0033001, 2020. DOI: http://dx.doi.org/10.1590/1980-5918.033.ED01.
GUO, T.; FAN Y.; CHEN M.; et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardio; March 27, 2020.
IMOTO et al. Cloroquina e hidroxicloroquina no tratamento da COVID-19: sumário de evidências. Com. Ciências Saúde 2020;31 Suppl 1:17-30.
LINDAHL, S. G. E.; Using the prone position could help to combat the development of fast hypoxia in some patients with COVID-19. Acta Paediatr. 2020 Aug;109(8):1539-1544. Epub 2020 Jun 17. DOI: https://dx.doi.org/10.1111%2Fapa.15382
MARTINEZ, B. P.; ANDRADE, F. M. D.; RONCALLI, A. et al..Intervenção na insuficiência respiratória aguda. ASSOBRAFIR; Março 2020.
MATOS, C. M. P.; SCHAPER, F. C.. Manejo fisioterapêutico para COVID-19 em ambiente hospitalar para casos agudos: recomendações para guiar a prática clínica. Dep. de Fisioterapia da Somiti. DOI: http://www.somiti.org.br/arquivos/site/comunicacao/noticias/2020/covid-19/documentos/manejo-fisioterap-utico-para-covid-19.pdf.
MATTE, Darlan Laurício; ANDRADE, Flávio Maciel Dias de; MARTINS, Jocimar Avelar. et al.. O fisioterapeuta e sua relação com o novo SARS-CoV-2 e com a COVID-19. ASSOBRAFIR CIÊNCIA; 2020 Ago;11(Supl 1):17-26. DOI: http://dx.doi.org/10.47066/2177-9333.AC20.covid19.002
MUSUMECI, M. M.; NOGUEIRA, I. C; ALCANFOR, T. A. F. et al.. Recursos fisioterapêuticos utilizados em terapia intensiva. ASSOBRAFIR; Maio 2020.
MUSUMECI, M. M.; MARTINEZ, B. P.; NOGUEIRA, I. C. et al.. Recursos fisioterapêuticos utilizados em unidades de terapia intensiva para avaliação e tratamento das disfunções respiratórias de pacientes com COVID-19. ASSOBRAFIR; Agosto 2020; 11 (Supl 1): 73-86.
PINTO, T. F.; CARVALHO, C .RF..SARS CoV-2 (COVID-19): lessons to be learned by Brazilian Physical Therapists. BJPT Associação Brasileira de Pesquisa e Pós-Graduação em Fisioterapia (ABRAPG-Ft). DOI: https://doi.org/10.1016/j.bjpt.2020.04.004.
REIS, M. A. S.. Suporte ventilatório COVID-19. AMIB – Associação de Medicina Intensiva Brasileira.
SEVERIN, R. et al.. Respiratory Muscle Performance Screening for Infectious Disease Management Following COVID-19: A Highly Pressurized Situation. O American Journal of Medicine. 2020. DOI: https://doi.org/10.1016/j.amjmed.2020.04.003.
SILVA et al. Evidências científicas sobre fisioterapia e funcionalidade em pacientes com COVID-19 adulto e pediátrico. J Hum Growth Dev. 2020; 30(1):148-155. DOI:http://doi.org/10.7322/jhgd.v30.10086.
SOHRABI et al.. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020 Apr; 76: 71–76.
WINCK, J. C.; AMBROSINO N. COVID-19 pandemic and non invasive respiratory management: Every Goliath needs a David. An evidence based evaluation of problems. Pulmonology. 2020 July-August; 26(4): 213–220.
WITTMER, V. L.; MOULIM, M.C.B.; GUIMARÃES, R. F.; et al.. Diário de exercícios fisioterapêuticos – pacientes estáveis com suspeita de COVID-19.Universidade Federal do Espírito Santo. 21 de abril de 2020.
THOMAS, P.; BALDWIN, C.; BISSETT, B.; et al.. Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. Journal of Physiotherapy. Volume 66, Issue 2, April 2020, Pages 73-82. DOI: https://doi.org/10.1016/j.jphys.2020.03.011
YEO, T. J.; WANG, Y. L.; LOW, T. T.. Have a heart during the COVID-19 crisis: Making the case for cardiac rehabilitation in the face of an ongoing pandemic. National Heart Centre, Singapore. Apr, 2020.
[1] Physical therapist. Santa Catarina Educational Institute – Guaraí College (IESC/FAG). Physiotherapy course.
[2] Physical therapist. Educational Institute Santa Catarina Faculdade Guaraí (IESC/FAG). Physiotherapy course.
[3] Master in Bioengineering with Emphasis on Health. Physical therapist.
Submitted: December, 2020.
Approved: January, 2021.















