ITIYAMA, Andressa Ferreira Alves [1]
ITIYAMA, Andressa Ferreira Alves. Lymphohemangioma: Coping with a Teenager with Congenital Chronic Disease. Revista Científica Multidisciplinar Núcleo do Conhecimento. Issue 05. Year 02, Vol. 01. pp 513-528, July 2017. ISSN:2448-0959, Access link: https://www.nucleodoconhecimento.com.br/health/lymphohemangioma
SUMMARY
This qualitative study seeks to know the critical view of a patient in relation to the hospital environment revealed in the recurrent hospitalizations. It aims to analyze the nursing-patient and hospital-patient relationship. Data collection was performed through an interview recorded on cassette tape using oral life history as a methodological reference. Later this interview was transcribed, textualized and transcreated. From the data obtained, we found that the collaborator observed that nursing is technically well trained to assist, but there is still a lot to fail in the question of “knowing how to hear” the patient’s needs. It is considered, therefore, that nursing practice aims beyond the cure of the client a humanized treatment aiming to lead to the recovery of the psychosocial balance of the individual.
Keywords: Oral History of Life, Lymphohemangioma, Chronic Disease, Congenital Disease, Hospitalization.
1. INTRODUCTION
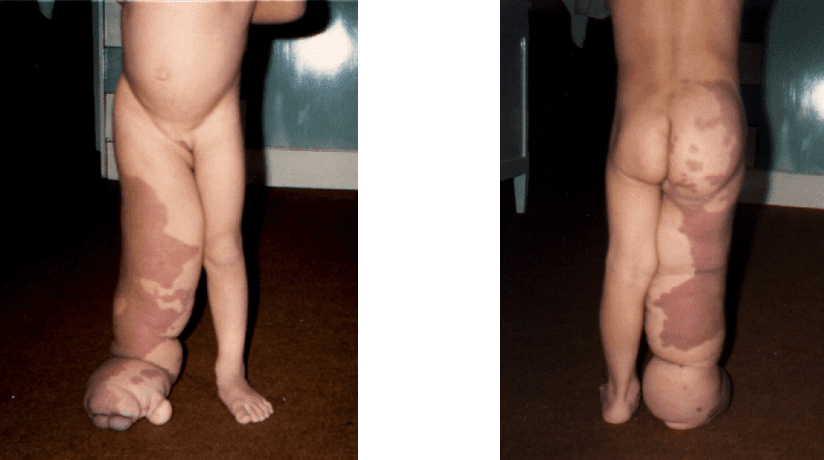
The operating room of a large hospital is the scene of countless stories of personal and family lives sometimes rich in philosophical and technical teachings for the best performance of the health professional. She was an employee of one of these surgery units, in which I came into contact with a patient with extensive lymphohemangioma, congenital chronic disease, and who had undergone a series of surgeries since early childhood and because it is a rare pathology that has no cure, I was curious to inform myself more about the subject and especially about the patient who at no time presented herself discouraged or defeatist and who , finally motivated me to carry out this study.
According to Magalon; Paty (1989), lymphangiomas are the result of a poor development of the lymphatic system, which can occur at different stages of embryology. Lymphohemangiomas or hemolymphinfangiomas are lymphangiomas associated with vascular or capillary malformations. These rare anomalies are usually congenital or may appear soon after birth, but can also occur at any age (KOÇER, 2003).

They can be classified into three types: Simple, Cavernous; poorly delimited lesion, often associated with hemangioma, cystoid; small malformation (MAGALON; PATY, 1989).
According to Magalon; Paty (1989), the most frequently affected areas are the head, neck and extremities, and the extremities are very difficult to be treated.
Other structures may be affected, such as studies carried out in the spine (WATKINS et al., 2003), orbit (KALISA et al., 2001), lung (WILSON et al., 2001), hepatic (DATZ et al., 2001), stomach (KIM et al., 2001), spleen (KWON et al., 2001), mediastinal (OSHIKIRI et al., 2001), ovary (KEAMEY et al., 2001), retroperiton (UCHIDA et al., 2002) among others.
Specific manifestations appear according to the location of the lesion. In the cervical region lymphangiomas are most often located laterally (below the mandible, along the carotid groove and above subclavicular depression). Diffuse forms can lead to life-threatening, involving the peritracheal areas, pharyngolaryngeal muscles and the floor of the mouth, thus justifying an emergency surgery (MAGALON; PATY, 1989).
In the tongue, both diffuse and localized lymphangiomas are passive to occur. The full thickness of the tongue can be infiltrated, giving it a firm and bulging appearance. Diagnosis can be made based on the presence of small cysts on its surface. The consequences can reach the mechanism of speech and even a severe mandibular prognathism (MAGALON; PATY, 1989).
Orbital lymphangiomas cause a certain degree of exophthalemia, with impediment of eye movement or ptosis. Diagnosis is easier if there is involvement of the eyelashes or conjunctiva. The mean age of the appearance of orbital lymphangiomas is at six years of age (MAGALON; PATY, 1989).
According to Magalon; Paty (1989), lymphangiomas can occur at any end. The lesion may be superficial, with some skin vesicles; it can also be deep, diffuse and infiltrating, with muscle involvement and extremity deformation. Hemolymphangiomas (vascular malformation) are common in the extremities.
During clinical examination of the malformation, the degree of functional degeneration, as well as the extent or depth of development, should be evaluated (MAGALON; PATY, 1989).
Radiology allows the evaluation of the depth of infiltration and, in particular, the extent of muscle development, in cases involving diffuse lymphangioma of the extremity. Lymphography may be useful for detecting communication between lymphangioma and the deep lymphatic system (MAGALON; PATY, 1989).
The treatment aims firstly to make the extremity work again and secondly also obtain acceptable aesthetic results through plastic surgery techniques (MAGALON; PATY, 1989). Sclerotherapy with substances such as OK-432 (Picibanil) with relative success (HALL et al., 2003; GIGUÈRE, 2002; CLAESSON, 2002), radioteapia (BRUNS, 2002), CO2 laser (LAY; Hanson, HANSON, MALLORY, 2001) and Nd:YAG laser (HARASHIMA et al., 2001).

Berenguer et al. (2002) highlights the need for multidisciplinary collaboration to provide the patient with an accessible and comprehensive treatment
Quayle, 2010. Lucia (2003), remind us that health professionals and patients live in different universes: one revolving around the objectivity and scientificity of pathological phenomena, while the other is immersed in the solitary and human experience of falling ill […] taking into account the meanings belonging to the patient […].
Nursing work is continuous and uninterrupted, since it remains in constant expedients with the frequent presence of strong emotions in the face of life often in danger and also the permanent need for adaptation to people, makes the nursing team need good working conditions, so that the care provided is adequate and effective. Often this is not possible, but as recurrent hospitalizations of patients who require constant care occur, it is necessary that there be an awareness of nursing professionals in order to offer help, self-esteem and subsidies for the faster recovery of the patient, but without forgetting to listen to the needs of this patient in particular.
With this thinking, we have the importance of this study, to better understand the view of a adolescent with stigmatizing disease in relation to the hospital environment, and aims to identify the flaws in the nursing-patient relationship to outline strategy and offer more humanized care.
According to Mezomo (1995), humanization is the communication of the word, gesture and gaze. Remembering that each patient has different ways of approach, respecting their needs and expectations.
2. OBJECTIVE
This research aims to know the critical view of a patient in relation to the hospital environment unveiled in the recurrent and prolonged hospitalizations, reported through oral history of life. Analyzing the nursing-patient and hospital-patient relationship.
3. METHODOLOGY
This research was developed with an experience report of a adolescent with chronic disease. Oral History of Life was used as a methodological framework, which is a modern technique for the preparation of documents, filings and studies related to the social life of people. It is always a story of the present time and also known as living history. Oral history is presented as a way of capturing the experience of people willing to talk about aspects of their life, maintaining a commitment to the social context. In the former days, the procedures for capturing statements were made through notes and memorization, and today there is mandatory electronic participation in oral history, and statements recorded the basis of the existence of oral history (MEIHY, 1998).
It is necessary to adopt some measures in the conduct ionof recordings such as (MEIHY, 1998):
- Schedule the interviews according to the convenience of the employee;
- Attend the place at the scheduled time and date;
- Create a climate of solidarity open to warmth, trust and respect;
- Request consent to record, as well as the consent form and signature of the legal guardian.
For Meihy (2002), the interviewees are the people heard in a project and should be recognized as collaborators […] who have greater freedom to lecture, as freely as possible, about their personal experience.
After approval of the research project by the Philanthropic Hospital of Londrina, which has the Committee of Bioethics and Ethics in Research in Human Beings, she was invited to be the subject of the research, L. M. C., white, female, 17 years old, third-year high school student, middle class, had extensive lymphohemangioma detected at birth. In which she underwent several reparative surgeries since childhood.
Because she was a minor, I initially had an informal approach with her and her mother to explain the objective of the work, that is, to report her life history of some situations experienced in the hospital environment. With his consent was drawn up a consent form signed by the minor and his legal guardian his mother, in which he clarified his freedom to, at any time give up the research without causing any kind of damage or embarrassment.
Data collection was performed through a recorded interview mediated by a pre-prepared instrument with pre-established script (Annex C), in a quiet and friendly climate, in her residence in the municipality of Cornélio Procópio – PR, where the author moved.
After the interview, the transcription (process of changing the stage of oral recording to the written code), textualization (reorganization of the narrative where the researcher’s questions are suppressed and aggregated the collaborator’s answers) and transcreation (interview already worked in its public presentation phase with the grammatical corrections and the completed sentences, everything should be established in this stage) as described by Meihy (2002).
4. RESULTS AND DISCUSSION
To unseeand interpret the situations experienced by patient L.M.C. we describe below the conductive wires for the development of the research, as (annex – c).
First, it was addressed regarding their hospitalizations, through the question “How do you feel at each hospitalization?” since hospitalizations are a routine for this patient.
“The hospital is part of my home. After the surgery I spent seventy days in the hospital with the same people, I only saw them… With my family I only spoke on the phone because they couldn’t go to the hospital to see me. So it’s part of me… like it’s my beach house.
In the hospital you see a lot… you realize that there are people there who are by vocation, gift, because they like that there. You also see people who are there because there’s nothing else to do.”
Certain professionals have the ability, the gift, to establish a relationship with the patient; to know that your professional action is done with another person (the patient) and not on another person (a body). They realize that they can, through a good interaction with the patient, contribute as a powerful determinant of healing by associating with the unconscious forces that lead the patient to fight for life (MELLO, 1992).
We know that in health institutions, the scarcity of professionals cause them to overload nursing activities, often causing the failure to attend due to the lack of time for humanization with the hospitalized patient. However, nurses should not conform to these institutional problems, having the obligation to always be seeking continuous improvement of the quality of care and service through awareness and stimulation of the employee’s motivation under his direction.
Another question raised was in relation to: “What marked you during the various hospitalizations and hospital interventions?”.
“When I went to the CTI (Intensive Care Center), I had taken all the bone out of the little finger and half the second; so I was dying of pain, because it moved with tendon, with bone… was on morphine; I was really upset, and the person who was looking after me wanted to change my bed. So why change the bed, if you can see that I’m in pain… that I’m not getting to sleep… that I was without my mother, I was alone… They learn that you have to change the bed, but is it preferable for you to change the bed or let the patient rest? You see the patient’s in pain. It’s a knowing thing about measuring what’s important and not.”
In intensive care units where professionals are highly qualified on the technical issue and are accustomed to working with extremely severe patients who are generally unconscious, sedate and intubated sometimes have difficulties in dealing with patients as described in the above section who are only there for a better observation of immediate postoperative, especially when this is a teenager who is facing a hostile environment alone. For sure the staff saw the need to change the bed at that time, but was this not a time to consider the patient’s well-being first? Yes, we should never forget that the main goal of our work is to take care of the client as a “whole”. The nurse who is coordinating work actions within any unit should be sensitive to the personal needs of each patient, and also act as a bulwark.
Costenaro (2001), reports that the nurse, in addition to being responsible for assessing the patient’s needs, should also be concerned with the nature and quality of the resources available to meet this need. This is mainly due to the particularities experienced in UTI (Intensive care unit), where the client arrives in an unknown environment and is manipulated by the team, consisting of unknown people […]. In addition to going through the process of separation of the family and social environment. During the provision of care, the nursing professional should value subjectivity, intuition and sensitivity, as well as consider the experiences experienced by the patient […].
Taking advantage of the subject raised by the patient in relation to the care provided in the UTI, she was asked what she thought of the care provided by the nursing and other professionals involved.
“People are very good… are very good professionals… do very well the work, how to give medicine. These things have always been very good… have always been excellent in the services provided. Only that’s what I said, the emotional part is missing; they work a lot with techniques.”
In general, health professionals are very attentive when they start their careers, but the harsh reality of everyday life and the routine, sometimes dull, make them very technical professionals and little sensitive to the suffering of others, making the hospital a cold and uncozy place.
It is necessary that the nurse, who is the leader of the team, is able to provide patients with a humanized environment, where harmony and respect for the human being is emphasized as a person. Thus, we emphasize that it is up to nurses to accept the challenge of providing a therapeutic environment, capable of promoting physical comfort, alleviate anxiety, aiming at humanized and integral care to clients (COSTENARO, 2001).
Among the critical analyses of the collaborator, the lack of availability of some nurses in the care of their patients stands out.
“I’m tired of seeing the doorbell calling, on the little post is the nurse and she does not get up to go to answer because it is not her service … I mean, yes, but it’s not. So some should come down a little bit from the pedestal… they are not all, most are good, but have some, as the other there londrina says the “Barbie”, sit tidying her hair and passing lipstick. I think they should work a little harder.”
The nursing body should work as a group interacting with each other. Of course, it is up to the nurse to coordinate the actions of his subordinates, but he must never forget that being responsible for the sector and there being no one who can attend the patient, he is the person who should assist him, as did the copy Florence Nightgale.
According to Guimarães (1995), nurses have earmarked more time for activities that directly use the achievement of the institution’s objectives and, by doing so, have been suffering criticism stemming from their work, increasingly focused on bureaucratic administrative actions, where direct care to the patient and relegated to the background.
As health professionals, we must not forget that our messages are interpreted not only by what we speak, but also by the way we behave (SILVA, 1996).
Time is precious to you, as well as for patients, to learn how to promptly attend the campaign or justify a delay in care (SILVA, 2000).
Asked about the expectation of nursing, she vents:
“I don’t know what it’s like in college… It seems that you learn the pathology, how to treat, how to give the medicine… I’m not just talking about nurses anymore, but i’m talking about doctors anymore. You forget that the patient is a person, not a doll you’re treating… You know, anything, a doll you keep in your wardrobe and that’s it… He won’t talk to you anymore. Forget there’s someone there. so I don’t know how college works. Whether they work on it or not. But it’s something that goes a lot of the person knows how to hear… not just college. I’m not criticizing anything. only that people had to know how to listen to others.”
According to Frank (1995), listening to the one who suffers is an arduous task for the human being, particularly when the listener is a wholesome person. Their voices refer to the conditions of the body, which reveal our own vulnerability. His words are easy to ignore, as they are often articulated outside the cadence and bring conflicting messages. However, listening is a fundamental moral act, and requires an ethical attitude of listening on the part of another human being. By listening to the other, one listens to oneanother, and crystallizes the sharing of each other’s needs.
College actually always teaches how to treat the patient in a humanized way, but perhaps a greater emphasis on the subject is needed, since the students for the most part are people who are inexperienced in the subject concerned with doing what is right in the technique and sometimes do not give the necessary attention to what the patient has to say. This can bring an addiction to professional conduct that will accompany you for the rest of your life.
At the end of the interview, she was asked how she felt when she went to the operating room.
“I love the operating room. I wanted the surgery so badly that I came down awake (no sedation). All surgeries were life-threatening, in the first ones mainly because no one had ever done anything like this. But I was calm… Everything was fine and i risked dying in surgery, but I had the risk of me dying from the infection. So if I died in surgery, I’d be in a place I wanted to… now an infection with pain… I didn’t want that anymore. I had spent a lot of time in my life with infection and i didn’t want that anymore.”
Oliveira (1994), draws our attention to the fatalism that accompanies chronic disease people conform to the disease and, at the same time, with the idea of death. One faces reality, the uncertain future and death, which may be closer than one imagines. But although conformed, people do not abandon the struggle and the search for a better quality of life.
The patient with chronic disease, has the tendency to interrupt treatment for periods of discouragedness or even lack of encouragement from family members. It is up to us nurses to be close and perform continuing education and motivate them in adherence to treatment.
FINAL CONSIDERATIONS
The various events that permeate a person’s life require answers so that they can overcome moments of instability, changes in self-esteem, paper performance, anxieties, depressions and insecurity to regain balance.
Nursing, when performing care, contributes to increase the possibilities of psychosocial recovery of the individual, not focusing only on the cure of the disease. It is important to support a person in transition, helping to protect and maintain their health for the future. The objective of nursing intervention is to take care of clients, creating a condition conducive to a healthy life, coordinating the changing being as an integral holistic being.
Considering the increasing economic, political and technological pressures in the health area as well as the tendency to individualism and the lack of ethics in the relations between human beings and human beings with nature, it is believed that there is awareness for this imbalance to be perpetuated.
In view of the above, we can say that it is always more necessary to improve the nursing team, not only with techniques, but, above all, as people who communicate, sometimes in a plan of great empathy with patients.
The level of aspiration of the nursing team must be beyond the daily routine, as of people who emerge from the common society bringing conditioning and qualitative life expectancy and intend together with the patient and his/her family members to build a healthier world that is consistent with the dignity of the human person, as is the case of the patient in question, being a young woman who has much to experience.
These reflections aim to review nursing practice and improve the care that is so essential in the lives of our patients.
REFERENCES
BERENGUER, F. B. et al. Not all vascular birthmarks are angiomas. Anáis Español Pediatría, Espanha, v.56, n.2, p. 127 – 138, feb. 2002.
BRUNS, F. Lymphangiolipoma of the lower extremity: 5-year radiological follow-up after radiotherapy treatment. British Journal Radiologic, Inglatera, v. 75, n. 897, p. 767 – 771, sep. 2002.
COSTENARO, R. G. S. Cuidando em Enfermagem: pesquisa e reflexões. Santa Maria: Universidade Franciscano, 2001. p. 133 – 134.
CLAESSON, G. OK – 432 therapy for lymphantic malformation in 32 patients (28 children). Journal Otorhinolaryngol, Irlanda, v. 65, n. 1, p. 1 – 6, aug. 2002.
DATZ, C. et al. Massive progression of diffuse hepatic lymphangiomatosis after liver resection and rapid deterioration after liver transplantation. American Journal of Gastroenteroloy, Estados Unidos, v. 96, n. 4, p. 1278 – 1281, apr. 2001.
FRANK, A. F. When bodies need voices. In: ______. The woundel storyteller: body, illness, and ethics. Chicago: University of Press, 1995. cap. 1, p. 1 – 25.
GUIGUÈRE, C. M. et al. Treatment of lymphangiomas with OK-432 (Picibani) sclerotherapy: a prospective multi-institucional trial. Arch Otolaryngol Head Neck Surgery, Estados Unidos, v. 128, n. 10, p. 1137 – 1144, oct. 2002.
GUIMARÃES, E. M. P. Sistema de Informação: subsídios para organização e utilização na coordenação da assistência de enfermagem. Belo Horizonte: Universidade Federal de Minas Gerais, 1995.
HALL, N. et al. Is intralesional injection of OK-432 effective in the treatment of lymphangioma in children. Surgery. Estados Unidos, v. 133, n. 3, p. 238 – 242, mac. 2003.
HARASHIMA, T. et al. Treatment of lymphangioma with Nd: YAG laser irradiation: a case report. Journal Clinical Laser Medical Sugery, Estados Unidos, v. 4, n 19, p. 189 – 191, aug. 2001.
KALISA, P. et al. Orbital lymphangioma: clinical features and management. Bull Society Belge Ophtalmoloy, Bélgica, n. 282, p. 59 – 68, 2001.
KEARNEY, C. E. et al. Ovarian lymphangioma: MRI appearances. Clinics Radiology, Inglaterra, v.56, n. 8, p. 685 – 687, aug. 2001.
KIM, H. S. et al. Gastric lymphangioma. Journal Korean Medical Science, Coréia do Sul, v. 16, n. 2, p. 229 – 232, apr. 2001.
KOÇER, U. et al. Late-onset superficial lymphatic malformation: report of a case and review of the literature. Dermatologic Surgery, Estados Unidos, v. 29, n. 3, p. 291 – 293, mar. 2003.
KWON, A. H. et al. Laparoscopic splenectomy for a lymphangioma of the spleen: report of a case. Surgery Today, Japão, v. 31, n. 3, p. 258 – 261, 2001.
LAI, C. H.; HANSON, S. G.; MALLORY, S. B. Lymphangioma circumscriptum treated with pulsed dye laser. Pediatric Dermatologic, Estados Unidos, v. 18, n. 6, p. 509 – 510, nov./dec. 2001.
MAGALON,G.; PATY, E. Linfangiomas e hemolinfangiomas. In: JUAREZ, M. A. Cirurgia Plástica na Infância. São Paulo: Hipócrates, 1989. v. 2, p. 595 – 597.
MEIHY, J. C. Manual de História Oral, 2. ed. São Paulo: Loyola, 1998.
MEIHY, J. C. Manual de História Oral, 4. ed. São Paulo: Loyola, 2002.
MELLO, J. F. et al. Psicossomática Hoje. Porto Alegre: Artes Médicas, 1992. p. 363.
MEZOMO, J. C. Gestão da Qualidade na Saúde: princípios básicos. São Paulo: Terra, 1995. p. 276 – 279.
OLIVEIRA, A. G. C. Convivendo com a Doença Crônica da Criança: a experiência da família. São Paulo, 1994. p. 141.
OSHIKIRI, T. et al. Five cases of the lymphangioma of the mediastinun in adult. Ann Thoracic Cardiovascular Surgery, Japão, v. 7, n. 2, p. 103 – 105, apr. 2001.
QUAYLE, J.; LUCIA, M.C.S. Adoecer: as interações do doente com sua doença. São Paulo: Atheneu, 2003. p. 149.
SILVA, M. J. P. O Amor é o Caminho: maneiras de cuidar. São Paulo: Gente, 2000. p. 99.
SILVA, M. J. P. Comunicação tem Remédio: A comunicação nas relações interpessoais em saúde. São Paulo: Gente, 1996. p.19.
UCHIDA, K. et al. Huge scrotal flank and retropeirtoneal lynphnagioma successfully treated by OK-432 sclerotherapy. Urology, Estados Unidos, v. 60, n. 6, p. 1112, dec. 2002.
WATKINS, R. G. et al. Lymphangiomatosis of the spine: two cases requiring surgical intervention. Spine, Estados Unidos, v. 28, n. 3, p. 45 – 50, feb. 2003.
WILSON, C.; ASKIN, F. B.; HEITMILLER, R. F. Solitary pulmonary lymphangioma. Ann Thoracic Surgery, Estados Unidos, v. 71, n. 4, p. 1337 – 1338, apr. 2001.
[1] Postgraduate in Nursing from the Northern University of Paraná (UNOPAR).















