FREITAS, Katherine Valença [1], MATTOS JUNIOR, Márden Estevão [2]
FREITAS, Katherine Valença; MATTOS JUNIOR, Márden Estevão. Laboratory evaluation of Patients with Meningitis: differential diagnosis between Bacterial and Viral Meningitis. Multidisciplinary Core scientific journal of knowledge. 03 year, Ed. 06, vol. 06, pp. 147-168, June 2018. ISSN:2448-0959
Summary
The meningitis is inflammation of the meninges (pia mater, dura mater and arachnoid), several factors may lead an individual to develop meningitis, such as infectious agents (bacteria, viruses and fungi) and non-infectious agents, such as a trauma; individuals with greater susceptibility are children, immunocompromised patients and immunocompromised. This survey provides information of importance in the diagnosis of meningitis, being made a parallel between the bacterial and viral meningitis, which are of higher incidence. The main objective was defined what is meningitis, its peculiarities and identifies her laboratory, describing the clinical differences and clarifying the differential diagnosis between bacterial and viral meningitis. This study was conducted following the concept of bibliographical research, using material already prepared, formed of scientific articles, theses and books. The inclusion criteria used for selection of material was to select the data that had focused on the laboratory diagnosis and clinical/laboratory aspects of bacterial and viral meningitis. The laboratory parameters for the differentiation of bacterial meningitis of the viral examination of utmost importance is the analysis of cerebrospinal fluid showing change from macroscopic examination the more sophisticated tests. The analysis of cerebrospinal fluid after a bacterial meningitis if exudative and features facilitates the clinical differential diagnosis, unlike the analysis of samples after viral and fungal infections, which show less changes with transudate characteristics depending on clinical associations and more specific analyses as the microbiological and dosage of lactate to aid in the differential diagnosis.
Keywords: Meningitis, cerebrospinal fluid, cerebrospinal fluid, bacterial meningitis and Viral meningitis.
Introduction
The meningitis affect much of the world's population, being your main target children, including bacterial and viral. (1)
The problems presented in this work addressed the differentiation of bacterial and viral meningitis laboratory level.
Seeing that this disease affects the central nervous system (CNS) there is great importance in studying it and deepen the knowledge about it and its variations, as well as the different ways to diagnose them accurately. (2, 3)
Bacteria and viruses are the main etiological agents cause of meningitis, so they must be differentiated by the fact that the prognosis and treatment of the patient depends on the causative agent (pathogen); that must be identified by the clinical/laboratory relationship, besides a good anamnesis of the patient. (4, 5, 6)
The present research becomes important to aid in the diagnosis of meningitis with emphasis on differentiation of bacterial and viral, in conjunction with the clinical and physical examination of the patient to be observed. (7, 8)
This work aimed to define what is meningitis, how to make an identification laboratory and its peculiarities, clarifying the differential laboratory diagnosis between bacterial and viral meningitis and describing the differences clinics between viral and bacterial meningitis.
This work was done following the concept of a bibliographical research exploratory, which "is developed from material already prepared, consisting of books and scientific articles, among other types of available electronic holdings. (9)
We used scientific articles, these articles can be accessed in the databases of the Scielo public health magazine, São Paulo, Arq of Neurosiquiatr, Journal of Pediatrics and Journal of Human Growth and Development; also been used dissertations, of which many are available in the virtual library of the University of São Paulo (USP) and the National School of public health – FIOCRUZ and clinical/laboratory interest books in addition to official sites, as well as Ministry of health, FUNASA, Secretaria de Estado da Saúde de São Paulo State Secretariat of health (SESAB) which discuss the topic in question, in the period from 1993 to 2015. Inclusion criteria were followed the materials that had focused on the laboratory diagnosis and clinical/laboratory aspects of meningitis, especially viral and bacterial, and to submit in your contents keywords, such as: meningitis, cerebrospinal fluid, cerebrospinal fluid, bacterial meningitis and viral meningitis.
Meningitis
The meningitis are classified as an inflammatory process of the meninges (pia mater, dura mater and arachnoid), being these membranes that surround the spinal cord and the brain. (19, 10) The paquimeninge are called meningitis when they reach the dura and leptomeninge, when they reach the arachnoid and pia mater. (5)
Several factors may lead an individual to develop meningitis, such as infectious agents (bacteria, viruses and fungi) and non-infectious agents, such as a trauma. The meningitis of infectious origin are of most interest for your great clinical occurrence and ability to unleash outbreaks; in focus that are caused by viruses and bacteria. (18)
For the development of meningitis, the pathogen crosses the blood-brain barrier and the blood-cerebrospinal fluid barrier of the human organism. With trauma injuries can also contribute to contamination of the CSF; In addition to congenital malformation and surgical procedures. (17)
As clinical feature, we must consider some classic symptoms, such as fever, myalgia, vomiting, headache, lethargy, irritability and signs of meningeal irritation, as the signs of Kening, Brudzinski and Lasègue's maneuver. (7)
Along the disease the patient may present pictures of delirium and coma. Taking into account the degree to which the brain was affected may arise seizures, paralysis, pupil disorders, tremors, among others. (18)
These patients present a clinical picture compatible to an infectious syndrome with signs of radicular syndrome and intracranial hypertension, being taken into account the changes of the quimiocitológico examination, characterized by increased cellularity (value of Variant as reference age group) and biochemical changes. (2)
Bacterial meningitis
It is characterized as a meningitis inflammation of the spinal region, arachnoid and pia mater, which are the membranes lining the brain and spinal cord. (3, 16, 20)
In susceptible individuals, any bacterium has the ability to produce meningitis. In approximately 95% of cases, the bacterial meningitis are caused by the bacteria Haemophilus influenzae type b, Streptococcus penumoniae (Pneumococcus) and Neisseria meningitidis (meningococcus). In some cases, meningitis can be caused by a bacterial invasion indirectly, for example, a sinusitis, mastoiditis and on rare occasions by an otitis media. (3, 19)
Still did not know the form of invasion of bacteria in the subarachnoid space and the exact location where they enter the central nervous system. Studies suggest that they can go through the choroid Plexus, where their cells along with the brain capillaries may have receivers that offer adherence to bacteria, so the carriage of the bacteria to the subarachnoid space, where they will find conditions for your breeding, since this space does not have a defense mechanism that can control the infection. (3)
The evolution of bacterial meningitis may present in different ways, the most lenient, even excessively severe. Their degree of importance is linked to the age of the patient, as well as, the pathogen involved. Patients aged over 60 years and under the age of 1 year, have greater tendency to later complications such as neurological sequelae and even death. (6)
Is of paramount importance to identify the etiological agent that causes meningitis, for it must rely on accurate diagnosis techniques, agile and reliable. (5)
The late diagnosis contributes to the high rate of mortality and morbidity, especially in children, even with antibióticoterapia as well as provide complications with worsening of prognosis, therefore one of the most important points of the diagnosis of bacterial meningitis is the clinical suspicion, in conjunction with the laboratory data. (1, 14)
One of the consequences of bacterial meningitis is the production of a Vasculitis, thrombus formation, which may evolve into a stroke or a cerebral infarction, due to the action carried in the blood vessels by bacteria, in addition to neurological problems and possible death. (11, 15)
The bacterial meningitis can lead to vascular complications as arthritis and thrombophlebitis, vascular complications of which the most common are the thrombophlebitis. The pathophysiological course involved in vascular changes leads to actions of the bacteria, which release Inflammatory Cytokines, such as tumor necrosis factor (TFN) and Interleukin-1 (IL). (11)
Etioepidemiologia-bacterial meningitis
Many bacteria can promote meningitis, in Brazil we can highlight three, as the most common and the main etiological agents, responsible for up to 95% of cases of bacterial meningitis, being them, Neisseria meningitidis, Streptococcus pneumoniae and Haemophilus influenzae. (4, 13, 14, 17, 18)
In infants up to 3 months and in neonatal period, the etiological agents involved in the pathology in question are the Streptococcus agalactiae (Group B), Listeria monocytogeneses, Enterobacter spp., Klebsiella pneumoniae, Salmonella enteritidis and Escherichia coli. Infection by these bacteria may be arising out of childbirth, due to vaginal mucosa, because they are pathogens that colonize the region. (3.19)
In the period of three months of age, called the transition period can be found both agents of the neonatal period, as those that affect children after this age, the most common until the age of eighteen are Neisseria meningitidis, Streptococcus pneumoniae and Haemophilus influenzae type b. In adulthood the gram-negative enteric bacilli, Listeria and Haemophilus influenzae type b are pathogens of greatest incidence. (3.19)
Meningitis caused by Streptococcus pneumoniae, Gram-positive bacteria, being alfahemolítica and not groups, with spherical, feature reporting in pairs, with wide variety of capsular Xenobiotics, is considered more serious, due to after-effects left by Pneumococcus. Some factors predispose to infection by this bacterium, being the most significant pneumonia, in addition to acute or chronic otitis media, alcoholism, diabetes, chronic obstructive pulmonary disease, renal failure, among others. (19, 3, 18)
The Neisseria meningitidis is a gram-negative diplococcus shaped, contains many Xenobiotics, serogroup A is what is more associated with epidemics, but those responsible for much of the meningococcal disease are the B and C, in your most of Group b. (4 , 12, 18.19) more common in children under the age of five years, meningococcal disease can occur at any age, and in individuals who exhibit deficiency of complement system, anatomical or functional asplemia and properdina are more susceptible to disease caused by meningococcus (3.19)
Meningococcal disease can be considered cosmopolitan and seasonal, and represents about 20% of cases of bacterial meningitis. (12, 14) The possibility of deaths by meningococcal disease is on average 5% to 15%, and in a few cases sequels when cured. (19)
The Haemophilus influenzae is a gram-negative, small, or not, capsular capsular pleomorphous and presents six groups (a to f). The most invasive form of the disease, is usually determined by the type b, because their capsular strains. The strains devoid of capsules are found usually in airway, involved in infections in adults as in children, infections such as sinusitis, bronchitis and otitis media. (3.18)
In general the meningitis caused by Haemophilus influenzae presents endemic character and your target audience ranges in age from 3 months to 18 years. Although she usually leaves low lethality demonstrate sequelae with higher frequency, such as deafness. With vaccination anti-Haemophilus influenzae type b (Hib) meningitis caused by Haemophilus influenzae, ceased to be the main agent of bacterial meningitis caused. (6, 19)
In patients with change in cellular immunity and the elderly the most common etiological agent is Listeria monocytogeneses, a gram positive Bacillus, staying in second place as a cause of meningitis in elderly, being surpassed only by penumococo. This bacterium affects especially transplant patients and with lymphoma. (19)
Staphylococcus epidermidis and Staphylococcus aureus are the main bodies involved in the meningitis after illnesses, especially Staphylococcus aureus, bacteria that is also involved in meningitis after lumbar puncture, so such as Pseudomonas aeruginosa. (6, 18.19)
Tuberculous meningitis is caused by Mycobacterium tuberculosis, which is a Bacillus, rod-shaped, without flagella, no producer of toxins and does not form spores, when stained by Ziehl-Neelsen method, not bleach after passage by alcohols. Meningitis caused by this bacterium is more common in recém-nacidos and children who inhabit the region with high rate of tuberculosis, showing slowly advancing. (17, 18)
In General gram-negative rods are the cause of meningitis in diabetic patients, chronic drinking, suffering from urinary tract infections to chronic character, in a patient with disseminated strongyloidiasis and also after procedures neurosurgical; patients in this condition are more susceptible to disease. (17, 18)
Viral meningitis
Viral meningitis presents a patient with a clinical neurological change, which usually evolves more lenient, compared to the meningitis caused by other agents, such as bacteria, not showing involvement of spinal cord and/or brain parenchyma. (4, 6)
The most affected by this pathology are children, generally under the age of five, however, this does not exclude the possibility that individuals from other age groups are susceptible to disease. On average 85% of cases of viral meningitis are caused by the Enterovirus, emphasizing the Poliovirús, Echovirús and Coxsockievírus of the groups A and B 1.2. (4)
The meningitis caused by enterovirus present specific clinical signs, such as gastrointestinal changes, breathing, skin rash, in addition to the classic signs seen on meningitis. (7)
Sometimes, however, can present more serious paintings with dire prediction, being in their clinical manifestations, both related to the age of the patient, as the etiological agent involved, or to the State of immune competence of the patient, and may some remain with sequels, such as memory loss, anosmia, dysphagia, personality changes, hemiparesis, ataxia, seizures and coriorretinites, among others; In addition to psychosis, characterized by memory loss and personality changes. (6)
Climatic, geographical conditions, exposure to animals, among other factors, predisposes a particular population, the prevalence of some of these viruses. (6)
Etioepidemiologia-viral meningitis
Viral meningitis can be considered seasonal, cosmopolitan and also your highest rate is in temperate, with prevalence in early spring and summer, but must be taken into consideration the health infrastructure, population clusters and virulence of pathogens, that interfere directly in the expression. (6, 7)
In 2015 7194 cases were reported of meningitis viral etiology, featuring a number of 120 deaths, being that your ID has only been possible due to outbreaks. (4, 28)
Usually the viral meningitis are more frequent in children due to fecal-oral transmission, but may affect any age, being epidemic or sporadic form. (6, 25)
Many viruses can cause meningitis, especially the enterovirus, which account for an average of 85% to 90% of cases of meningitis, the enteroviruses can be found anywhere in the world, and your single reservoir is the man. (6) one of the enterovirus, included the poliovirus (3 strains), coxsackie virus B (6 strains), echovírus (28 strains), coxsackieviruses A (23 strains), and 5 strains of other enteroviruses. (17.18)
In addition to enterovirus can also highlight the mumps virus, arbovirus, the herpes virus, the measles virus, the varicella virus, rubella virus and adenovirus, in addition to these other viruses also have great potential to cause meningitis, as the Epstein-Barr virus, AIDS, Cytomegalovírus and Lymphocytic Cryomeningitidis virus. (6)
The Herpes simplex virus (HSV 1 and 2) have high prevalence and are found throughout the world, and the meningitis caused by these viruses are considered a medical emergency, considered as the second largest cause of viral meningitis in adults and teenagers. (6, 26) It is estimated that 60% to 80% of the world's population are HIV positive for HSV1 and HSV2 for ranging from 20% to 10%, noting that infections take place by direct contact with secretions containing the virus, as well as by contact with infected injuries. (6)
The mumps virus has been the most frequent between the viral meningitis, but after vaccination (developed at the 60), has been virtually eradicated. Edema in the Parotid gland, even without parotitis, can generate a meningitis. In some countries, this virus has seasonal behaviour, with prevalence in winter and spring, being more frequent in people over 15 years. (6, 26)
Pathophysiology
Generally pathogenic germs can colonize the upper airways, being considered the initial event of a bacterial meningitis, usually by encapsulated organisms, like pneumococcus, meningococcus and hemófilo type b. (19)
The virulence factor of the micro-organism, as well as the defense of the host State, may favor an invasion of epithelium by pathogen, spreading through the bloodstream. (19)
The bacteria release specific enzymes in the process of mucosal invasion, such as IgA proteases by clicking them and inactivating the enzyme local specific, subsequently attacking the epithelium of the respiratory tract, causing loss of ciliary activity of the epithelium, binds selectively to the non ciliated epithelium through their fimbrias and the host receptor. (3)
The intense inflammation of the meninges is induced by bacterial Lysis and the subsequent release of the elements of your cell walls, once released these substances, they will stimulate the release of microglia cells and astrocytes, in addition to the production of cytokines, as the tumor necrosis factor and Interleukin-1, which are considered triggers of meningeal inflammatory response. (3.19)
The cytokines produced induce an increased permeability of the blood-brain barrier, this event promotes the emergence of cerebral edema of vasogenic type and allows the passage of leukocytes and proteins to the CSF, elements that make the formation of a thick exudate. CSF reabsorption can be blocked by the throat, through the aracnoideas grits, as noted in Figure 1. (19)
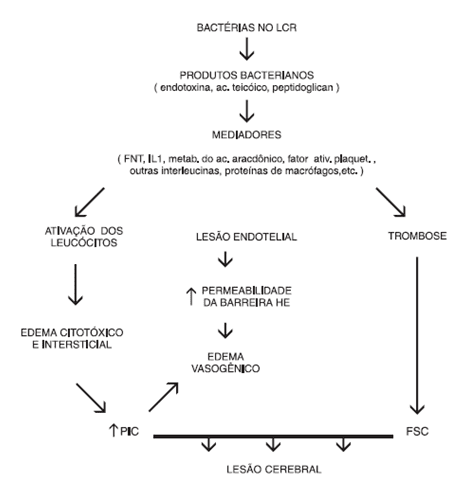
With the advance of infection there is loss of self-regulation central nervous system vascular, causing the blood flow to the brain is dependent on the systemic blood pressure directly. (3.8)
The inflammatory process that affects the subarachnoid space ends up affecting the blood vessels by contiguity, as a Vasculitis, causing a thrombosis and ischemic cerebral infarction and may also encourage the spread of infection to the brain, causing the appearance of brain abscesses. (19)
Diagnosis
The early diagnosis of meningitis is very important for the treatment to be effective, and that mortality and morbidity rates are reduced. (3)
Clinical diagnosis
The most characteristic clinical signs of meningitis are fever, nausea, vomiting, headache, myalgia, reigidez on the back of the head, mental confusion, signs of meningeal irritation (sign of Kerning, Lasègue's maneuver and Brudzinski), besides the changes in cerebrospinal fluid (CSF). (7, 18)
Sign of Kerning: there is a difficulty in extending the legs, when it flexes the trunk. (7, 18.19)
Lasègue's sign: lower limb elevation towards the hip. (7.18)
Brudzinski's sign: to Flex slightly to head toward the chest, the legs also declined. (7, 18.19)
Laboratory Diagnosis
To diagnose meningitis can be made an analysis of the cerebrospinal fluid, blood and scraped of the lesions, as well as analysis of urine and feces, for viral meningitis. (18)
The laboratory analysis of the cerebrospinal fluid provides extremely relevant information for future diagnosis of the patient. (19)
When there is suspicion of meningitis the main tests requested for research are: cytological examination of CSF, Gram stain, culture, contra-imunoeletroforese and agglutination by LaTeX. (18)
Laboratory analysis of the material collected
For the diagnosis of meningitis it is necessary that we collect cerebrospinal fluid (CSF), if the patient presents a low level of consciousness it is recommended to be taken, such as CT and MRI, before the puncture. The CSF leak puncture should be performed on the spine, which includes L1 to S1, indicated the locations of the L3-L4, L4-L5 and L5-S1. This collection must be made by a clinical pathologist and the material forwarded to the laboratory of clinical analyses. (16, 19, 20)
Can be collected an amount of up to 20 ml of the material, you must simultaneously also spoon venous blood sample for comparisons between plasma glucose and liquorica and chlorine. It is important to stress that the bottles used for the harvest of the material must be sterile (sealed and autoclaved and should not be used after your due date. (16, 20, 22).
In all three tubes are collected, which will be sent to the sectors of Microbiology, biochemistry and Immunology and haematology. In case of suspicion of malignancy can be included a fourth pipe, which will be forwarded for cytology, clarification of suspicion. (16, 20)
At the end of the harvest material should be forwarded to the laboratory and analyzed as soon as possible, to reduce the degradation of the same, beginning on average 1 hour after collection, considering that this easy material deterioration. (16, 20)
The CSF in normal individuals appears colorless and clear, with the "water of rock". (5, 16, 19, 20)
The increased cellularity in the CSF may cause cloudiness of the same, depending on the amount and type of cells can be a variation of your coloring. (19)
The CRL if left in standby mode should not introduce changes, such as blood clots and precipitations. In abnormal conditions can introduce some changes. (16, 19, 20)
The fibrinous exudation: the material is presented clearer looking, but when at rest it is formed a lattice, similar to a network, waving to the slightest movement. (20)
Turbid liquid: may indicate meningitis in the acute phase. (19, 20)
Purulent liquid: indication of meningitis in the chronic phase. (20)
Hemorrhagic fluid: initially one should search if the aspect of hemorrhagic cerebral spinal fluid is associated with a puncture accident, which can be seen throughout the collection, in other words, if the hemorrhagic aspect is stronger in the first tube collected and lighter in the other, suggests that really there has been an accident in the Act of collecting, however if the material present hemorrhagic aspect uniform indicates that very blood comes from the subarachnoid space. (20)
Liquid xanthochromic: pós-hemorragia meningoencefálica or meningeal observed in adult and meningeal reaction in infants with jaundice. (16, 19, 20)
Biochemical tests used for the dosage of proteins, glucose, urea, chlorides, among others. CSF glucose corresponds to a large part (2/3) of circulating glucose in the body. The best way to measure a patient's glucose is making a relationship of glucose present in the CSF and serum glucose; already the amount of proteins depends on the age factor and location of the harvest of the material. (19)
The concentration of proteins is directly related to the degree of the infectious process, thus also changing the concentration of the CSF. (5)
Most of the proteins contained in the CSF is derived from plasma (about 80%). The increase of proteins is not very specific, but is of great value to the diagnosis. (16)
The high level of total protein, usually is equivalent to the degree of pleocytosis. (20)
The existing glucose in CSF depends on the glucose in the blood. (16, 20)
The high rate of glucose in CSF cannot be taken into account and/or has no clinical significance, and until 2 hours after the completion of the LP the glucose can be changed. The trauma caused by the punch can lead to increased apocryphal. (16)
Chloride levels in the CSF are related to the osmotic pressure exerted by the acid-base balance and the intracellular medium. (5)
Amendment globulínica in the CSF is expressed by the reactions of Pandy, Ross-Jones and Nonne-Apelt based on flocculation of protein. (20)
The increase of proteins present in the CSF positive reactions of the globulins. To the diagnosis must take into account the high levels of protein. (5)
The cytological examination if counts of cells and red blood cells, which is a quantitative examination and morphological quote. (5)
The LCR in your composition offers poor cellularity in, being in your majority composed of lymphocytes and monocytes. When there is an increase in the number of cells in the material called pleocytosis, and may be classified as moderate to severe. (16, 19, 20)
CSF cell count, the same cannot be diluted, and your count be made on manual camera. This count in camera may not be very accurate. For best accuracy using automated methods, not being dispensable to count. (16)
Must be done a smear coloured for the total count (global) and the differential (count) of cells found in the material. (19)
Only the differential does not determine the etiology of meningitis, but your absence classifies meningitis as not determined. (2)
The culture method used for confirmation of Gram stain, which may present erroneous results. This method allows already made a sensitivity test of the sample. The biggest problem presented in culture is the delay in obtaining results, and can be between 3 to 4 weeks. (20)
For an accurate diagnosis is necessary for the cultivation of the microorganism is made in good condition, both physical as nourishing of the culture medium chosen. Conservation, care with transport, storage and material culture medium chosen is of great importance for a proper diagnosis. (5)
The Gram stain aims to search the pathogen present in the cerebrospinal fluid, and the results depend on several factors, such as time of specimen collection (via spinal tap), growing media and appropriate culture, sample storage and antibióticoterapia prior to specimen collection. (5)
This method allows the classification with a low degree of specificity, grouping tintorialmente and morphologically the agents. (2)
Although not a very reliable, the Gram stain method can provide useful data to research, how to detect the most common pathogens of bacterial meningitis, about 80% to 85% of cases are confirmed by the Gram. (19, 20)
The contra-imuneletroforese is an effective test for detecting bacterial meningitis, when you have negative results on culture and Gram stain. (20)
The production of immunoprecipitation consists of applying an electric current, in order to accelerate Immunodiffusion in agar or cellulose acetate of the Antigen, so that he directs to the antibody. (5)
In relation to bacteriological examinations by Latex Agglutination test routine is the most feasible, due to your power to allow indirect detection of the pathogen, rather used for Diagnostics, on the basis of urgency may be used blood samples or CSF. (5.17)
"This method utilizes latex particles sensitised with specific antibodies absorbed in your surface for detection of Antigen directly in clinical specimens. In the presence of homologous Antigen visible agglutination occurs. " (5)
Laboratory profile comparison between the bacterial and viral meningitis
To set up a laboratory profile that characterizes and differentiates the bacterial and viral meningitis, need mostly a sample of cerebrospinal fluid of the individual suspected of the disease, but the blood sample is not expendable. The examination of blood count is possible to observe a significant Leukocytosis, mainly in the bacterial, and viral in being watched increase in acute phase, in some cases, noting that the definitive diagnosis is made with the analysis of the cerebrospinal fluid. (24, 26)
Macroscopic examination
In general the LCR coloring on bacterial meningitis will of milky-white to slightly xanthochromic, increased cellularity can leave the cerebrospinal fluid cloudy and your intensity varies the amount present in the same cells, neutrophils Let your cloudy lysates and purulent. (16, 18.19)
Usually the meningitis viral in origin have the CRL of limpid and colourless, with low numbers of cells, however, in meningitis in the acute phase can present slight cloudiness. (14, 19, 27)
Cytological examination of cerebrospinal fluid
Normally the spinal fluid shows 4 cells/mm ³, being composed of monocytes and lymphocytes. (19)
The growth of leucocitárias cells comes from the inflammatory/infectious process. (16)
The cytokines are produced after the release of endotoxin by bacteria, favoring the emergence of selectins, which in your time are receptors for leukocytes, found in endothelial cells, this event helps the migration of these cells for the CSF, leaving it more cloudy, as the intensity of infection. (19)
Usually in bacterial meningitis is seen an important pleocytosis with cellularity above 1,000 cells/mm ³, even without cellular differentiation, your prevalence tends to be polymorphonuclear (PMN) cells, however in acute phase features dominance of monocytes (mononuclear). (14, 16, 27)
Viral meningitis presents cellularity less than 1,000 cells/mm ³, being predominant mononuclear (MN), however in the acute phase can come to present polymorphonuclear (PMN) rate higher, so how can suffer in this context, changes in cases of infections with Herpes simplex virus (HSV), for example, where there may be variation of cellularity ranging from 0 to 2,500 cells/mm ³, being that your predominance should be 50 to 800 cells/mm ³. (14, 27)
Biochemical examination
Usually the viral meningitis there is no change in the levels of glucose and proteins can vary from normal to slightly increased, by contrast, the bacterial meningitis, the biochemical examination demonstrates a decreased glucose concentration (< 40 mg/dL), unlike proteins, which is high (usually > 100 mg/dL). (14.4 .13, 27)
The low level of glucose is characteristic of bacterial meningitis, when there is increased consumption via anaerobic Glycolysis by brain tissue and by white blood cells. (16)
The increased permeability of the blood-brain barrier, can generate an increase in the number of proteins, which can be caused by inflammation, as well as an obstruction (blockage) of CSF flow and decreased reabsorption in the villi aracnóideos. (16)
With the increased permeability of the hematoecefalica barrier, by changing its properties, there is the favouring of a cerebral edema (vasogenic type), allowing to have a leukocyte extravasation and proteins to the CSF, elements that lead to formation of a thick exudate, which blocks the CSF reabsorption. (19)
The reaction of Pandy show positive in bacterial meningitis, because of the increase of proteins, thus changing the globulins, because the high concentration of proteins tend to eventually turn positive reactions of the globulins, in General showing no change in case of viral meningitis. (5, 26)
High concentration of C-reactive protein (CRP) in the acute phase, has been used in differentiation of viral and bacterial meningitis. A supposed a negative result with low value, can drop by up to 97% of the meningitis research be of bacterial origin. (16)
The concentration of chlorides in bacterial meningitis decreased because of the presents acído-basic imbalance and the changes of the intracellular medium osmolarity which the body is going through. (5, 18)
Lactate is used as a differential test for bacterial and viral meningitis. High concentrations of lactate in CSF demonstrate anaerobic metabolism in the central nervous system, due to hypoxemia. (3.16)
High concentrations of lactate are more present in bacterial meningitis, showing rates above 35 mg/dL, unlike viral meningitis in which lactate, almost always less than 35 mg/dL, and usually offers less than 25 mg/dL. Persistently elevated concentrations are associated with a poor prognosis for patients with head trauma. (16)
Gram stain
An examination of extreme importance is the bacteriological, which aims to identify the pathogen in cerebrospinal fluid. Considered as "gold standard", the culture, even if little late, can set the proper diagnosis. As the bacteria that cause meningitis are sensitive to humidity and temperature should know the appropriate way to make the culture. The cultivation in Middle chocolate agar with growth already suggests that the Etiologic Agent is bacterial, and can also be grown in middle of-Lowenstein-Jansen is suspected case of tuberculous meningitis. (5, 6, 18)
The Gram is a presumptive method, microscopy could prove positive for gram negative diplococcus, Gram-negative bacilli, coconuts Gram-positive and Gram-positive bacilli. (14, 18)
Against-imuneletroforese and LaTeX agglutinins
The contra-imunoeletroforese is an important method for the diagnosis of bacterial meningitis, as well as being fast, if shows reagent for Streptococcus pneumoniae, Haemophilus influenzae and Neisseria meningitidis. By Latex Agglutination, as well as the controimuneletroforese, when in contact with the Antigen specific, visible agglutination occurs, in research to detect viral meningitis these tests will be negative, not being reagents. (13, 18)
You can also use the imunoenzimáticos tests for the identification of bacterial antigens, usually a solid support, where specific antibodies bind. We still have the molecular method and the polymerase chain reaction (PCR), which are used as more specific tests. (6)
Final considerations
The laboratory parameters for the differentiation of bacterial meningitis of the viral examination of utmost importance is the analysis of the cerebrospinal fluid, showing changes since the macroscopic examination the more sophisticated tests, in which all tests are important in phase of early diagnosis, to treatment be carried out as soon as possible. The analysis of cerebrospinal fluid after a bacterial meningitis exudative features and makes the differential diagnosis, as opposed to the analysis of samples after viral infections, demonstrating less changes with features of transudate, Depending on, of more specific analyses and clinical associations such as microbiological and dosage of lactate to aid in the differential diagnosis.
It is observed that in bacterial meningitis the CSF, usually blurred, because of the high protein and your high cellularity, mainly polymorphonuclear, causing your colour varies from white to Milky xanthochromic, in contrast in the CSF viral meningitis is colorless and with predominance of mononuclear cells, however in the acute phase of the disease may present slight turbidity and increased polymorphonuclear. If dealing with biochemical analysis, is observed in bacterial meningitis there is an increase of proteins, as well as in the acute phase of viral meningitis, which may vary from normal to slightly increased; the low level of glucose is characteristic of bacterial meningitis, showing no change in viral. Main differential test, has been used the determination of lactate, which brings high concentrations in bacterinas meningitis, showing no significant changes in viral. The Gram stain and culture tests are used for confirmation and identification of the etiological agents of bacterial meningitis, later being made contra-imunoeletroforese and agglutination tests for LaTeX, which show positive/ reagent, unlike viral meningitis, where no change in these tests.
Therefore, the laboratory analysis of the cerebrospinal fluid becomes important in clinical use as a means of differential diagnosis associated with disorders that affect the central nervous system, especially of infectious origin.
References
1. Lete R, Garcia J, Ferreira A, J, J, Goés Valli M, et al. Clinical and laboratory features of bacterial meningitis in children. Arq Neuropsiquiatr. 1996; 54 (54): 571-6.
2. Freitas CAP. Study of the occurrence of meningococcal meningitis not in the city of Ribeirão Preto-SP, in the period from 1998 to 20[dissertação]0[Internet]5. Ribeirão Preto: University of São Paulo – USP; 2007. [acesso em 2016 mar 08]. Available at: http://www.teses.usp.br/teses/disponiveis/17/17139/tde-17032008-142358/fr.php
3. Would SM, Farahat Ck. Bacterial meningitis: diagnosis and conduct. Journal of Pediatrics. 1995; 75 (1): 46-56.
4. State Secretariat of health of São Paulo. Viral Menintes. São Paulo. Rev. Public Health. 2006; 40 (4): 748-50.
5. Atobe JH. DNA amplification of Neisseria meningitides in cerebrospinal fluid sample employed a polymerase chain reaction-multiplex[dissertação]. São Paulo: University of São Paulo – USP; 1998. [acesso em 2016 mar 08]. Available at: http://www.teses.usp.br/teses/disponiveis/9/9136/tde-11082006-115017/pt-br.php
6. Trócoli MGC. Epidemiology of bacterial and viral acute meningitis occurred in the Instituto Estadual de Infectologia São Sebastião (IEISS)-Rio de Janeiro. Period: 11/11/96 to 10/06/9[dissertação]7[Internet]. Rio de Janeiro: National School of public health-FIOCRUZ; 1998. [acesso em 2016 mar 28]. Available at: http://www.arca.fiocruz.br/xmlui/handle/icict/4650
7. Nunes RAL. Application of molecular techniques in laboratory diagnosis complement the viral infections of the central nervous system at the University Hospital of the University of São Paul[dissertação]o. São Paulo: University of São Paulo – USP; 2013. [acesso em 2016 mar 08]. Available at: http://www.teses.usp.br/teses/disponiveis/42/42132/tde-19032014-160513/pt-br.php
8. Tauil MC. Epidemiological aspects of meningococcal disease in 2000 to 2011[dissertação]. São Paulo: University of São Paulo – USP; 2013. [acesso em 2016 mar 08]. Sisponível in: http://www.teses.usp.br/teses/disponiveis/6/6132/tde-14032013-131623/pt-br.php
9. Gil AC. Methods and techniques of social research. 6. Ed. São Paulo: Atlas S.a.; 2008. p. 49-59.
10. Escosteguy CC, Medronho RA, M. R, HG, Baron RC, Azevedo OP. Epidemiological surveillance and evaluation of assistance to meningitis. Rev. Public Health. 2004; 38 (5): 657-63.
11. Rajan VMLM, Rock CM, Fernandes WLM, Warrior MM. Acute bacterial meningitis. Vascular Complications. Arq Neuropsiquiatr. 1993; 51 (4): 507-10.
12. CMCN Oak, Oak OAM. Etiology of Bacterial Meningitis in a population sample of Salvador-Bahia. Arq Neuropsiquiatr. 1998; 56 (1): 83-7.
13. GC Boiler. Humoral immune response of patients with meningococcal disease front the specific lipooligossacaarídeos[dissertação]. São Paulo: University of São Paulo – USP; 2004. [acesso em 2016 mar 08]. Available at: http://www.teses.usp.br/teses/disponiveis/9/9136/tde-28012005-111217/pt-br.php
14. Costa GAM. Behavior of neonatal bacterial meningitis according to birth weight[dissertação]. São Paulo: University of São Paulo – USP; 2006. [acesso em 2016 mar 08]. Available at: http://www.teses.usp.br/teses/disponiveis/5/5141/tde-06022007-095913/pt-br.php
15. Miller. Lab for clinical. 8. Ed. São Paulo: Atheneu; 1999. p. 533-42.
16. Henry Jb. Clinical diagnosis and treatment by laboratory methods. 20 ed. São Paulo: Manole; 2008 p. 471-95
17. Santos Av. Meningitis[trabalho de conclusão de curso]. São Paulo: FMU; 2007. [acesso em 2016 abr 05]. Available at: http://arquivo.fmu.br/prodisc/pharmacy/avs.pdf
18. Ministry of health (Brazil). Guide to epidemiological surveillance. 7 ed. Brasília: Secretary of health surveillance/MS; 2009. P. 21-47
19. Marino M, MR, Nicolich M, Netto M, Messina B. Infectious Diseases. Medcurso. 2014; (3): pp. 45-50.
20. Miller. Lab for clinical. 8. Ed. São Paulo: Atheneu; 1999. p. 153-8
21. Ministry of health (Brazil), NHS Foundation, the National Center of epidemiology. Infectious and parasitic diseases: clinical aspects, epidemiological surveillance and control measures. Brasilia: FUNASA; 2000. p. 65-6
22. Central Laboratory Of The State Of Paraná. Handbook of biological samples collection and sending the LACEN/PR: 1.30.001 Manual. Curitiba: LACEN; 2012.
23. Vieira s. assessment of concentrations of antibodies to serotypes 4, 6B, 9V, 14, 18 c, 19F, and 23F of Streptococcus pneumoniae before and after implementation of the 7-Valent Conjugate Vaccine in children with chronic renal failure on conservative treatment and dialys[dissertação]i[Internet]s. São Paulo: Faculdade de Medicina da Universidade de São Paulo-USP; 2007. [acesso em 2016 mar 08]. Available at: http://www.teses.usp.br/teses/disponiveis/5/5141/tde-24102007-144034/pt-br.php
24. CAR Oak. Foundation of Tropical Medicine Doctor Hector Vasquez[homepage na Internet]. Meningitis[acesso em 2016 jul 30]. Available at http://www.fmt.am.gov.br/manual/meningite.htm
25. Adam FG, Wajnsztejn R, Adams CAE, moral TC, Fujimori M, Adami F, et al. Laboratory parameters of cerebrospinal fluid in patients with meningitis for enteroviruses. Journal of Human Growth and Development. 2015; 25 (2): 237-242.
26. Damiani D, Furlan MC, Damiani d. aseptic Meningitis. Rev Bras Clin Med. 2012; 10 (1): 46-50.
27. Government of the State of Bahi[homepage da internet]a. Laboratory diagnosis of meningitis líquores x results pathologies[acesso em 2016 ago 22]. Available at: http://www.suvisa.ba.gov.br/sites/default/files/vigilancia_epidemiologica/imunopreveniveis/arquivo/2012/08/09/DIAG%20LABORATORIAL%20L%C3%8DQUOR%20X%20PATOLOGIAS.pdf
28. Ministry of health (Brazil), the health Portal[homepage da internet]. Confirmed cases, deaths, incidence (per 100,000 inhabitants) and lethality (%) by type of meningitis. Brazil, 2010 to 2015 *. [acesso em 2016 nov 23]. Available at: http://portalsaude.saude.gov.br/images/pdf/2016/outubro/33/tabela-2000-2015_meningite.pdf
[1] Student college life sciences Patos de Minas-FPM forming in the year 2016
[2] Faculty of life sciences from the Faculty course Patos de Minas-FPM. Master's degree in Physiological Sciences from Universidade Federal do Triângulo Mineiro-UFTM















