CASE REPORT
SILVA, Alexandre Augusto Ferreira da [1], ROCHA, Roberto de Oliveira [2], MARIANO, Ronaldo Célio [3]
SILVA, Alexandre Augusto Ferreira da. ROCHA, Roberto de Oliveira. MARIANO, Ronaldo Célio. Bilateral tapia syndrome after maxillomandibular advancement surgery. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year. 06, Ed. 10, Vol. 08, pp. 49-59. October 2021. ISSN: 2448-0959, Access Link: https://www.nucleodoconhecimento.com.br/health/bilateral-tapia, DOI: 10.32749/nucleodoconhecimento.com.br/health/bilateral-tapia
ABSTRACT
Hypoglossal and recurrent laryngeal nerve lesions in their unilateral or bilateral extracranial pathways cause a motor deficit in the tongue with transient, partial or total loss of speech, which may be associated with mild or severe dysphagia, characterizing Tapia’s syndrome. This unusual condition is usually related to airway manipulation during the anesthetic-surgical procedure, and few cases in the literature are correlated with maxillofacial surgery, which explains, in part, the lack of knowledge of this complication by a significant number of professionals. We describe a case report of bilateral Tapia syndrome established after a procedure for maxillomandibular advancement. This is a 55-year-old male patient diagnosed with retrognathism and retromaxilism. The patient underwent maxillomandibular advancement with nasotracheal intubation. He evolved with bilateral Tapia syndrome, recovering from the signs and symptoms of this complication, being reoperated on to correct aesthetic results obtained in the first intervention, which were below acceptable, not evolving after this second surgery with the syndrome. We conclude that preventive measures must be taken, such as avoiding sudden movements in the head region and prolonged hyperextension of the neck during surgery, minimizing trauma to the tracheal tube on the tissues that cover the hypoglossal and recurrent laryngeal nerves.
Keywords: Syndrome, Recurrent Laryngeal nerve, Hypoglossal nerve, Swallowing disorders, Dysphonia.
INTRODUCTION
Tapia Syndrome is an extremely rare complication first reported in 1904 by Antonio Garcia Tapia, an otolaryngologist physician (VAREDI et al., 2003). It is usually associated with airway manipulation for general anesthesia, characterized by lesions in the extracranial pathways of the hypoglossal nerve (motor nerve of the tongue) and the recurrent laryngeal nerve (branch of the vagus nerve inneruning the vocal cord), causing neuropraxia of these nerves with greater unilateral frequency, but may also be bilateral, compromising tongue movement due to hypoglossal nerve injury and speech difficulty due to recurrent laryngeal nerve injury (VAREDI et al., 2003; FARHAD; SAEID; HAMIDREZA, 2019). Cinar et al. (2005) also add to signs and symptoms, mild or severe dysphagia depending on the extent of the lesion of the nerves involved and also on the fact that the involvement is uni or bilateral, and in unilateral involvement, speech difficulty associated with the projection of the tongue out of the mouth with deviation from its tip to the opposite side of the lesion are the most frequent characteristics, while bilateral involvement may occur complete absence of tongue protusion and total swallowing inability at a later stage of the syndrome.
The aim of this report is to describe a case that evolved with bilateral Tapia Syndrome after maxillomandibular advancement surgery. After the patient recovered from the signs and symptoms of the syndrome, he/she needed to be reoperated, not evolving after the second intervention with Tapia Syndrome.
CASE REPORT
A 55-year-old male patient, leucoderma, diagnosed with retrognathism with mandibular asymmetry and retromaxillism with vertical maxillary deficiency, associated with a clinical picture of obstructive sleep apnea in moderate degree. The reasons that led the patient to seek treatment were snoring, daytime sleepiness and impaired facial aesthetics. The patient underwent general anesthesia with nasotracheal intubation to perform a skeletal surge of 12 mm in the maxilla and mandible.
The patient, despite his maxillofacial skeletal deformity, was considered of probable easy intubation, but only during the second attempt of laryngoscopy was intubated. The cuff of the nasotracheal tube was inflated with pressure less than 20cm H2O. An oroaming buffer corresponding to the volume of three gauze sums of 7.5cm x 7.5cm in size was used to minimize the passage of fluids to the stomach. During the surgery that lasted 180 minutes there was a need to reinflate the cuff that had lost pressure, taking care not to exceed 20cm of H2O. Systolic hypotension was established at approximately 90 to 100 mmHg throughout the surgery. The patient remained in a semi-supine position with a head slightly higher than the trunk.
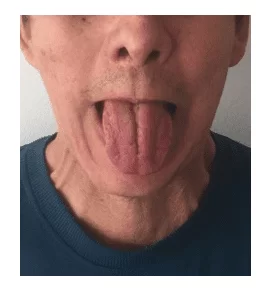
After the end of the surgery, the patient was extubated without any intercorence. Forty-eight hours after surgery, the patient still could not speak and we diagnosed that the tongue had almost no movement in the sense of protruding out of the mouth, lateralizing or rising to contact with the palate. On this occasion it was also verified that swallowing was very compromised and the patient could not swallow his own saliva. A nasofibroscopy was performed where bilateral vocal cord paralysis can be observed. Due to the difficulty of swallowing, the oral diet was suspended and a nasogastric tube was placed for the patient’s nutrition. Four days after surgery, the condition did not present any alterations. Computed tomography examination of the skull did not identify significant alterations and magnetic resonance imaging of the skull and neck found that the intracranial path of the hypoglossal nerve, as well as its canal and jugular forame were preserved. No changes in the topography of the hypoglossal nerve in its extracranial path were also identified. After any type of central nervous system involvement was ruled out, the diagnosis of Tapia Syndrome associated with severe dysphagia and dysphonia was established. The administration of corticosteroids (dmehasone – 4mg intravenously every 8 hours for 2 weeks) and B-complex vitamins was initiated for two months in order to accelerate the repair of injured nerves. As soon as postoperative edema began to regress, speech therapy for speech and swallowing began. The clinical picture of the patient remained unchanged in relation to Tapia Syndrome during the first postoperative week and, at the end of the postoperative period, pneumonia caused by aspiration of liquid foods was diagnosed during the first 48 hours postoperatively, when the oral liquid diet was still maintained. Over the subsequent weeks the patient fully recovered from pneumonia, and only three weeks postoperatively it was possible to observe that the right side of the tongue began to present a small protussion movement, with deviation from the tip of the tongue to the left, a fact that until then was not observed, but without any capacity to raise the tip of the tongue against the palate (Figure 1). On this occasion also the patient began to speak with great hoarseness and extreme difficulty. Each week the patient improved tongue movement and voice quality slightly, even having to feed by nasogastric tube and, only two months postoperatively, after several tests performed by the speech therapist to verify that the patient was able to swallow and not vacuuming pasty foods, the nasogastric tube was removed and oral nutrition was restored, without risk of a new aspiration with the development of a new aspiration pneumonia. The patient followed with speech therapy of oral motricity and to improve speech and swallowing, and progress was slow but constant, until four months postoperatively the patient could already make all the movements of the tongue (Figure 2), such as: protruding out of the mouth, making laterality and raising the tip of the tongue against the palate. The voice showed significant improvement in hoarseness, but it was still very different from the preoperative period. New nasofibroscopy has now evidenced only paralysis of the left vocal cord.
The patient continued to show significant improvement in the signs and symptoms of Tapia Syndrome with each passing month, however, the expected aesthetic result of maxillomandibular skeletal advancement surgery fell far short of what had been planned. Then, eighteen months postoperatively, with all tongue movements recovered and still with a small hoarseness in the voice, the patient was reoperated.
We establish precautions to reduce the chances of a recurrence of the signs and symptoms of this syndrome, such as: performing nasotracheal intubation with as little trauma as possible, controlling the pressure in the tube cuff, not using oropharyngeal packing, reducing surgical time as much as possible and avoiding excessive manipulation or hyperextension of the neck during surgery. This time we performed a surgery only in the maxilla associated with a mentoplasty, whose objective was to reduce the extension and duration of the surgery. The patient was then submitted again, after venous induction and deep healing, to nasotracheal intubation with minimal cervical extension and minimal manipulation of the glottis, with success in the first attempt. As in the first surgery, the patient was kept in a semi-supine position with the head slightly higher than the trunk and the oropharyngeal plug this time was not used in order to prevent compression on the hypoglossal and recurrent laryngeal nerves. The surgery lasted 120 minutes and at the end of the surgery the patient was extubated with minimal airway manipulation without the use of an oropharyngeal cannula. Immediately after the removal of the nasotracheal tube, the patient was already able to pronounce several words and, when asked to move the tongue in all directions, he did so. Absolute fasting was maintained for the first twelve hours after surgery. Twenty-one months after the first surgery and three months after the second surgery, a new nasofibroscopy exam still showed persistence of left vocal cord paralysis, and the patient still has a slight hoarseness in the voice, which was not aggravated for the second intervention and that does not interfere with their social life, remaining still in speech therapy to improve speech. The aesthetic results that motivated the indication for the second surgery were considered adequate by the team and the patient.
DISCUSSION
Tapia syndrome, although extremely rare, has as its most probable cause, airway manipulation in patients undergoing general anesthesia, either by naso or orotracheal intubation (CINAR et al.,2005; NALLADARU; WESSELS; DUPREEZ, 2012; CARIATI et al., 2016; MUMTAZ; HENRY; SINGH, 2018; FARHAD; SAEID; HAMIDREZA, 2019). Ota et al. (2013) described the etiology of Tapia Syndrome as a mechanical trauma, producing damage to the recurrent laryngeal nerve, branch of the vagus nerve, and on the hypoglossal nerve, which are close to the base of the tongue, and this place where the vagus and hypoglossal nerves cross can be compressed by the endotrachertube.
There are reports of Tapia Syndrome after surgeries in other locations outside the head and neck, such as after cardiac surgery (NALLADARU; WESSELS; DUPREEZ, 2012). There are reported cases whose proximity of the tracheal tube to the surgery site is very large, such as after repair of mandible fracture, rhinoplasty, surgery for fixation of zigoma fracture, orthognathic surgery and removal of the upper third molar retained under general anesthesia (KASHYAP et al., 2010; LYKOUDIS; SERETIS, 2012; VAREDI et al., 2013; OTA et al., 2013; MUMTAZ; HENRY; SINGH, 2018). In surgeries performed on the face it is common during the transoperative period for the surgeon to correct, one or more times, the positioning of the patient’s head, or even turn it over to one side or to the other depending on the region he will act on, and this may, in some circumstances, promote the displacement of the tracheal tube and this will traumatize the region superficially to the nerves involved in this syndrome (OTA et al., 2013). Therefore, preventive measures such as an intubation with less trauma possible, total control of air pressure in the cuff without ever exceeding 20cm H2O to avoid excessive compression of tissues superficially to nerves, proper positioning of the patient’s head without hyperextension of the neck for a long time, avoiding sudden movements of the head during surgery, may contribute to the prevention of this syndrome.
The bilateral incidence of Tapia Syndrome is exceptionally rare, and we found in the literature the case report of Cinar et al. (2005) who described a bilateral occurrence of this syndrome after a rhinoplasty, with resolution of symptoms completely in four weeks. In the present report, also with bilateral involvement, the patient only began to fully move the tongue and had the nasogastric tube removed two months after the first surgery, and with 18 months postoperatively the patient still presented paralysis of the left vocal cord and mild hoarseness in the voice that did not bother him, and then reoperated, not presenting in this second postoperative period, the signs and symptoms of Tapia Syndrome, showing that prevention care are fundamental strategies to avoid this condition.
Paralysis of the hypoglossal and recurrent laryngeal nerves unilaterally lead to the classic signs of Tapia Syndrome which are: motor deficit in the tongue with deviation from the tip to the opposite side of the injured hypoglossal nerve during the protusion movement of the same and dysphonia due to paralysis of the ipsilateral vocal cord (KASHYAP et al., 2010; LYKOUDIS; SERETIS, 2012). However, several authors add that dysphagia may be present in cases where trauma to the nerves involved has been greater, and may occur in unilateral and bilateral situations (CINAR et al.,2005; VAREDI et al., 2013; CARIATI et al., 2016). In bilateral cases there is almost complete absence of language movement in all directions, as in the case reported here. Ibrahim and Sarper (2010) classified Tapia Syndrome as mild, moderate or severe, however, they considered only unilateral involvement of the syndrome, and only in the severe type the patient presented difficulties in swallowing. In the present case, even because it was bilateral, the patient had total inability to swallow his own saliva during the first postoperative month of the first surgery.
For the treatment of this undesirable complication it is suggested to carry out corticosteroid therapy as soon as the diagnosis is made for a period that can vary around two weeks, as well as the administration of B-complex vitamins, aiming at an earlier repair of the function of the nerves involved, until significant improvement of symptoms occurs (CINAR et al., 2005; LYKOUDIS; SERETIS, 2012; CARIATI et al., 2016; MUMTAZ; HENRY; SINGH, 2018). There is a consensus that speech therapy to stimulate the improvement of diction, tongue movement and dysphagia, when present, is fundamental to assist in the reestablishment of the patient (VAREDI et al., 2013; MUMTAZ; HENRY; SINGH, 2018; FARHAD; SAEID; HAMIDREZA, 2019).
It is important to emphasize the need for an early diagnosis of Tapia Syndrome, even in the first hours of the postoperative period in which the patient has undergone general anesthesia, since in cases where dysphagia may be present, the release of the diet may lead to other complications, as occurred in the present case, where the patient remained on a liquid diet in the first 48 hours, aspiring content to the lungs with consequent development of pneumonia, which greatly complicated its recovery. As soon as the patient regains consciousness after general anesthesia and before introducing the diet it is essential to check the movement of the tongue in all directions, as well as whether the patient can pronounce a few words and swallow his own saliva. Due to its extremely unusual case, Tapia Syndrome is unknown to the vast majority of professionals, causing its diagnosis to be delayed until all the team that accompanies the patient can better understand the signs and symptoms presented by the patient, so that the diagnosis can be elaborated and consequently the treatment introduced.In the present case, the diagnosis was delayed and hindered by trying to find a relationship between signs and symptoms and surgery performed.
FINAL CONSIDERATIONS
Face surgeries have an extremely low relationship with the development of Tapia Syndrome, provided preventive measures are taken, such as avoiding sudden movements in the head region and hyperextension of the neck for long periods during surgery, minimizing tracheal tube trauma on tissues covering the hypoglossal and recurrent laryngeal nerves.
REFERENCES
CARIATI, Paolo; CABELLO Almudena; GALVEZ, Pablo P; LOPEZ, Dario Sanchez; MEDINA, Blas Garcia. Tapia’s syndrome: pathogenetic mechanisms, diagnostic management, and proper treatment: a case series. J Med Case Rep. v. 10, n. 23, jan. 2016. https://doi.org/10.1186/s13256-016-0802-1
CINAR SO, SEVEN H, CINAR U, TURGUT S. Isolated bilateral paralysis of the hypoglossal and recurrent laryngeal nerves (Bilateral Tapia’s syndrome) after transoral intubation for general anesthesia. Acta Anaesthesiol Scand. v. 49, n. 1, p. 98-99, jan. 2005. https://doi.org/10.1111/j.1399-6576.2004.00553.x
FARHAD, Ghorbani; SAEID Tavanafar; HAMIDREZA Eftekharian. Tapia’s syndrome after cosmetic malar augmentation: a case report. J Dent Shiraz Univ Med Sci. v. 20, n.1, p. 66-70, mar. 2019. doi: https://doi.org/10.30476/DENTJODS.2019.44566
IBRAHIM, Boga; SARPER Aktas. Treatment, classification, and review of Tapia syndrome. J Craniofac Surg. v. 21, n.1, p. 278-280, jan. 2010. https://doi.org/10.1097/SCS.0b013e3181c678f0
KASHYAP, Soumya A; PATTERSON, Alan R; LOUKOTA, Richard A; KELLY, Gerard. Tapia’s syndrome after a repair of a fractured mandible. Br J Oral Maxillofac Surg. v. 48, n. 1, p. 53-54, jan. 2010. https://doi.org/10.1016/j.bjoms.2009.01.021
LYKOUDIS, Efstathios G; SERETIS, Konstantinos. Tapia’s syndrome: An unexpected but real complication of rhinoplasty: case report and literature review. Aesthetic Plastic Surg. v. 36, n. 3, p. 557-559, jun. 2012. https://doi.org/10.1007/s00266-011-9849-y
MUMTAZ, Shadaab; HENRY, Alastair; SINGH, Mark. Tapia’s syndrome. Anesth Prog. v. 65, n. 2, p. 129-130, jun. 2018. https://doi.org/10.2344/anpr-65-04-06
NALLADARU, Zubin; WESSELS, Andre; DUPREEZ, Leon. Tapia’s syndrome – a rare complication following cardiac surgery. Interact Cardiovasc Thorac Surg. v. 14, n. 1, p. 131-132, jan. 2012. https://doi.org/10.1093/icvts/ivr056
OTA, Nobutaka; IZUMI, Kiwako; OKAMOTO, Yoshihiko; TOSHITANI, Koji; NAKAYAMA, Keisuke; FUKUZAWA, Hideaki; OZEKI, Satoru; IKEBE, Tetsuro. Tapia’s syndrome following the orthognatic surgery under general anaesthesia. J Oral Maxillofac Surg Med Pathol. v. 25, n. 1, p. 52-54, jan. 2013. https://doi.org/10.1016/j.ajoms.2012.02.001
VAREDI, Payam; SHIRANI, Gholamreza; KARIMi, Abbas; VAREDI, Peyman; KHIABANI, Kazem; BOHLULI, Behnam. Tapia syndrome after repairing a fractured zygomatic complex: a case report and review of the literature. J Oral Maxillofac Surg. v. 71, n. 10, p.1665-1669, oct. 2003. https://doi.org/10.1016/j.joms.2013.05.019
FIGURES AND LEGENDS
Figure 1: Three weeks postoperative of the first surgery where we began to observe a small projection of the tongue out of the mouth with deviation from the tip to the left.
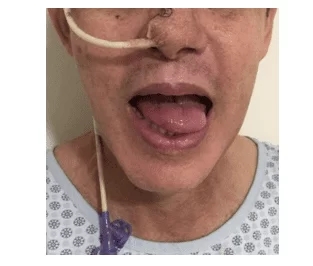
Figure 2: Postoperative 4 months after the first surgery when all tongue movements were recovered.
[1] Master’s degree from the Dental Sciences Program of the Federal University of Alfenas (UNIFAL-MG). Residency in Bucomaxillofacial Surgery and Traumatology at the Central Hospital of Santa Casa de São Paulo-SP. Specialist and Full Member of the Brazilian College of Surgery and Bucomaxillofacial Traumatology.
[2] Doctor of Medicine from the Neurology Discipline of the Hospital das Clínicas, Faculty of Medicine, University of São Paulo.
[3] Advisor. Full Professor, School of Dentistry, Federal University of Alfenas (UNIFAL-MG). PhD in Dentistry, Area of Surgery and Bucomaxillofacial Traumatology, School of Dentistry of Araçatuba, Unesp. Residency in Bucomaxilofacial Surgery and Traumatology, Ribeirão Preto School of Dentistry, USP.
Submitted: August, 2021.
Approved: October, 2021.















