REVIEW ARTICLE
SILVA, Natália Matos da [1]
SILVA, Natália Matos da. The mental health of health professionals related to the Covid-19 pandemic. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year. 07, Ed. 05, Vol. 02, pp. 173-189. May 2022. ISSN: 2448-0959, Access link: https://www.nucleodoconhecimento.com.br/health/health-professionals
ABSTRACT
A variety of symptoms related to mental health disorders, such as: stress, anxiety, psychological distress, depressive symptoms, insomnia and burnout, have been reported by health professionals as a result of the Covid-19 pandemic. In this context, this article was guided by the question: is the scenario of the Covid-19 pandemic conducive to the development of mental disorders in health professionals? Therefore, the objective is to investigate, in the already published literature, whether the pandemic is a factor that can trigger mental disorders in health professionals, as well as to identify scales, methodologies or protocols used to identify them. For this, the chosen method was the literature review. As a result, it was observed that the most used psychometric scales were: The Generalized Anxiety Disorder 7-item (GAD-7), Anxiety and Stress Scale. As a methodology or protocol, the literature pointed out: ESAE Scale (Examination of Subjective Anomalies of Experience) and Revised Impact of Events Scale (IES-R), Patient Health Questionnaire, World Mental Health-International College Student-WMHICS, PTSD checklist for DSM -5 (PCL-5), CAGE-AID, Composite International Diagnostic Interview (CIDI), Self-designed Demographic Questionnaire and Symptom Checklist 90 (SCL-90), Standard Questionnaire and Event Impact Scale – Revised ( IES-R-22), Center for Epidemiological Studies Depression Scale (CES-D), Covid-19 Peritraumatic Distress Index (CPDI) Questionnaire, Maslach Burnout Inventory (MBI); The 4-item Perceived Stress Scale (PSS-4), as being the most used. Furthermore, it was found that having a history of depression or anxiety disorder was a risk factor for the occurrence of depressive symptoms of moderate to severe intensity; the nursing profession was the factor most associated with psychological disorders and the medical profession was also a risk factor for the development of depressive symptoms and severe and moderate to severe anxiety symptoms. Finally, it was concluded that the mental health of all professionals working on the front line in the fight against Covid-19 deserves special attention for the early detection of psychiatric disorders, as the literature proves that this scenario is conducive to the development of severe and moderate to severe mental disorders in health professionals.
Keywords: Health professionals, Covid-19, Mental Health.
1. INTRODUCTION
The coronavirus (Covid-19) pandemic represented, and still represents, a problematic factor in global health. In this context, Ornell et al. (2020), states that it caused the confinement of entire populations, as well as an increase in the number of severely affected patients and in general mortality, causing psychological distress to the population.
However, it appears that the general population was not the only one vulnerable to psychological distress. After the confinement and the sudden increase in morbidity and mortality, the health system noted an increase in the prevalence of psychiatric disorders in health professionals who worked or work in the frontline team in the fight against the pandemic (KRISHNAMOORTHY et al., 2020; KOLA et al., 2021).
Through this, it was noticed that: the risk of contamination, the work overload, the physical exhaustion, the reorganization of spaces, the adaptation to rigid work protocols, the lack of protection materials, the high mortality of patients and the feeling of loss of control, associated with Covid-19, are sources of anxiety and depression in health professionals (KHANAL et al., 2020; SPOORTHY; PRATAPA; MAHANT, 2020).
However, it appears that in previous epidemics, such as H1N1 in 2009, health professionals have already revealed feelings of extreme vulnerability, somatic and cognitive symptoms, as well as high levels of anxiety, depression and long-term psychological distress (CORLEY; HAMMOND ; FRASER, 2010; GOULIA et al., 2010; IMAI et al., 2010; MATSUISHI et al., 2012). Feelings of loneliness, anxiety, fear, fatigue and sleep disturbances were also reported (CORLEY; HAMMOND; GOULIA et al., 2010; MATSUISHI et al., 2012).
In this context, this article was guided by the question: is the scenario of the Covid-19 pandemic conducive to the development of mental disorders in health professionals? Therefore, the objective is to investigate, in the already published literature, whether the pandemic is a factor that can trigger mental disorders in health professionals, as well as to identify scales, methodologies or protocols used to identify them. For this, the chosen method was the literature review.
2. MATERIALS AND METHODS
A bibliographic search was carried out between February 19, 2022 and March 17, 2022, for articles published in the Medline database (Medical Literature Analysis and Retrieval System Online) indexed in PubMed. For this, the recommendations of the PRISMA Checklist (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) were followed, which, according to Moher et al. (2015), in the context of systematic reviews and meta-analyses, have the function of detailing the reasoning, directing to an a priori methodological and analytical approach of the review.
First, the keywords were selected according to the descriptors in health sciences (MeSH): mental health; Health Personnel – or alternative term – health professionals; Covid-19 – and, alternate term, – Covid-19 Pandemic. Therefore, the terms with Boolean operators were: (health personnel) OR (health professionals) AND (mental health) AND (Covid-19) OR (Covid-19 pandemic), as shown in the table below:
Table 1 – Search terms using auxiliary terms and connectors
| Search: health personnel OR health professionals OR health workers AND mental health AND COVID-19 OR COVID-19 pandemic. Filters: Free full text, Associated data, Multicenter Study, Observational Study, Humans, English, MEDLINE. |
| (((“health personnel”[MeSH Terms] OR (“health”[All Fields] AND “personnel”[All Fields]) OR “health personnel”[All Fields] OR (“health personnel”[MeSH Terms] OR (“health”[All Fields] AND “personnel”[All Fields]) OR “health personnel”[All Fields] OR (“health”[All Fields] AND “professionals”[All Fields]) OR “health professionals”[All Fields]) OR ((“health”[MeSH Terms] OR “health”[All Fields] OR “health s”[All Fields] OR “healthful”[All Fields] OR “healthfulness”[All Fields] OR “healths”[All Fields]) AND (“occupational groups”[MeSH Terms] OR (“occupational”[All Fields] AND “groups”[All Fields]) OR “occupational groups”[All Fields] OR “worker”[All Fields] OR “workers”[All Fields] OR “worker s”[All Fields]))) AND (“mental health”[MeSH Terms] OR (“mental”[All Fields] AND “health”[All Fields]) OR “mental health”[All Fields]) AND (“covid 19″[All Fields] OR “covid 19″[MeSH Terms] OR “severe acute respiratory syndrome coronavirus 2″[All Fields] OR “2019 ncov”[All Fields] OR ((“coronavirus”[MeSH Terms] OR “coronavirus”[All Fields] OR “cov”[All Fields]) OR “covid 19 pandemic”[All Fields]). |
Source: Author (2022).
In the selection stage, the title and abstract of each article were analyzed. If there was consensus that an article was not suitable for inclusion, it was excluded. Full articles were independently selected and included according to the criteria mentioned below.
Studies published between 2020 and 2022 that were available in full for reading and written in English were included. Observational and cross-sectional studies, whether multicenter or not, on the mental health of health professionals during the Covid-19 pandemic were also selected.
For the search, mental health disorders were considered: burnout, Post-traumatic Stress Disorder (PTSD), anxiety disorders, phobias, depression, suicidal desire, psychotic disorders, and also psychosexual disorders.
Editorials, comments, letters to the editor, reviews and any other type of study that did not have the inclusion characteristics were excluded.
The figure below depicts the entire process described above.
Figure 1 – Article search flowchart and inclusion criteria, prepared according to PRISMA recommendations
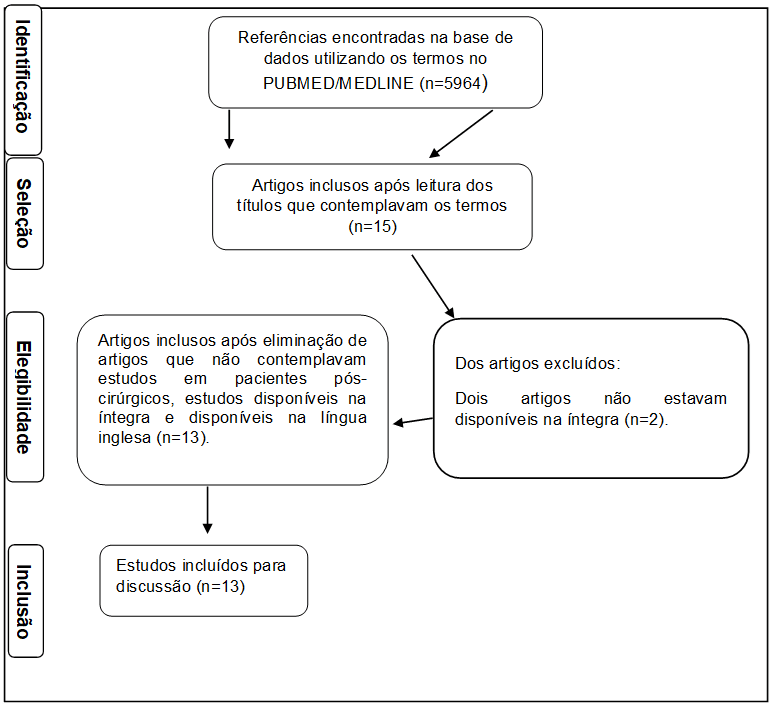
The literature search carried out identified 5,964 articles, which were screened in the first search in the PUBMED index, with filters according to the inclusion and exclusion criteria listed above. Therefore, 15 articles were included for full reading. After reading the texts, thirteen articles were selected to compose the final sample, as shown in Figure 1.
3. RESULTS
After carrying out the process described above, the information was extracted and organized into: author/date, research country, type of study, sample, main findings and reported conclusions. For this, Excel Software (Microsoft®) was used.
Chart 2 – Information extracted from the included studies
| Author/date | Country | Type of study and protocol | Sample | Main discoveries | Conclusions |
| Mira et al. (2020). | Spain | Cross-sectional study. Escala EASE (Exame das Anomalias Subjetivas da Experiência). |
685 health professionals. | Level of acute stress experienced is greater as the damage from Covid-19 increases in patients, and higher occurrence in territories where the pandemic has had the greatest impact in terms of incidence of cases and deaths from Covid-19. | – Acute stress affects most health professionals; – This type of stress reduces resilience to new waves of illness. |
| Ali et al. (2020). | Ireland | Observational multicenter cohort study Escala de Ansiedade e Estresse (DASS-21) e Escala de Impacto de Eventos Revisada (IES-R). |
472 health professionals. | The primary outcome showed prevalence of depression, anxiety, stress, and post-traumatic stress disorder (PTSD) among all health care workers. |
Psychological distress was prevalent among health professionals in critical hospital settings. |
| Alonso et al. (2020). | Spain | Cross-sectional research – Patient Health Questionnaire (PHQ-8); – seven-item Generalized Anxiety Disorder scale (GAD-7); – World Mental Health-International College Student-WMHICS. · PTSD checklist for DSM-5 (PCL-5); CAGEAID · Questionnaire; adapted version of Sheehan Disability Scale; Composite International · Diagnostic Interview (CIDI). |
9138 health professionals. | Prevalence: · female gender (77.3%), · age group was 30 to 49 years old (45.8%); · married (53.0%); · lived with children (41.4%) and, · 57.2% live in an apartment. · 26.4% were physicians; · 30.6% were nurses, · worked in a hospital (54.1%). · 80% directly involved in patient care, · 43.6% directly exposed to patients with Covid-19 all or most of the time. · 17.4% had Covid-19, · 13.8% had their spouse/partner, children or parents infected with Covid-19; · 25.5% were isolated or quarantined. · 41.6% reported pre-pandemic mental disorder(s) throughout their lifetime. |
High prevalence of probable mental disorders among healthcare workers during the first wave of the Covid-19 pandemic, with 1 in 7 experiencing a disabling mental disorder. |
| Bhargava; Sarkar and Kroumpouzos, (2020). | United States of America (USA) | Web-based cross-search. Questionário elaborado a partir de revisão minuciosa da literatura e testado piloto para garantir o fluxo adequado, saliência e aceitabilidade das perguntas. |
733 dermatologist doctors | · Mental suffering reported by 77.2% of respondents; · stress 73.9%; · Irritation 33.7%; · insomnia 30%; · depression 27.6% and, · 78.6% were overwhelmed by the amount of information about the pandemic they were receiving. |
– Mental distress was common among dermatologists during this pandemic. |
| Zhang et al. (2020). | China | Cross-sectional research Questionário de dados demográficos autoprojetado e Lista de Verificação de Sintomas 90 (SCL-90). |
450 health professionals. | · 178 participants were physicians; · physicians scored highest on most SCL-90 factors except for obsessive compulsiveness, hostility, phobic anxiety, and psychoticism (P < 0.05). The top 3 positive items for physicians were obsessive-compulsivity, other, and somatization. Among nurses were obsessive-compulsivity, others and hostility. -Gender, type of workers and risk of occupational exposure to Covid-19 were independent risk factors for the mental health status of community health workers |
Health workers suffered psychological problems during the Covid-19 outbreak in Sichuan Province, China. |
| Asnakew et al. (2021). | Ethiopia | Multicenter cross-sectional study. Questionário padrão e Escala de Impacto do Evento -Revisado (IES-R-22). |
396 health professionals. | Prevalence of: · post-traumatic stress disorder 55.1%; · age >40 years. |
More than 1/4 of the participants experienced severe post-traumatic stress disorder. |
| Ayalew et al. (2021). | Ethiopia | Multicenter cross-sectional study. Questionário padrão e A Escala de Depressão, Ansiedade e Estresse de 21 itens (DASS-21). |
387 health professionals. | Prevalence of: · 58.7% male, · 60.2% aged between 26 and 35 years old, · 49.4% married, · 77% were bachelors; · 59.4% had ≤5 years of experience, · 57.9% lived with their family, · 50.9% were nurses by profession and, · 35.7% worked in the emergency room. |
Symptoms of depression, anxiety and stress were the highly prevalent mental disorders experienced by health professionals. Being female, married, living alone, a nurse and working in hospitals were significantly associated with depressive symptoms. Older age groups, females, married couples and nurses were more likely to develop anxiety symptoms. Stress was significantly higher in females, married, living alone, nurses and working in non-emergency units. |
| Ibar et al. (2021). | Argentina | Cross-sectional observational study standard questionnaire and: · estresse percebido (Cohen et al., 1988), · suporte social (Timmerman et al., 2000), · escala de burnout (Maslach et al., 1997) e, · escala de eventos de vida de Homes-Rahe. Exames de níveis de cortisol no cabelo. |
234 health professionals. | · 40% had capillary cortisol values outside the healthy reference range. · 12% had burnout with the following distribution: 52% physicians and residents, 19% nurses, 19% administrative and the remaining technicians and maintenance. |
Health professionals have higher levels of stress and burnout. Given the current pandemic context, personnel in direct contact with patients face an increased risk of exposure to the disease, increased workload, moral dilemmas during care and fears about their own personal health. Capillary cortisol assessed by an automated method fulfills the requirement to assess stress status in this population. |
| Katsuta et al. (2021). | Japan | Observational cohort study Escala de Depressão do Centro de Estudos Epidemiológicos (CES-D). |
4239 health professionals. | The proportion of personnel with depression was 31.3% in 2020 with 27.5% pre-pandemic in 2019. The proportion of depression for 2020 was significantly higher in new hires than in employees with more than 2 years of experience (47.0% versus 29.9%; By occupation they present depression: · Nurses (43.2%), · paramedics (35.1%) · residents (22.9%), · doctors (20.4%), · teachers (18.0%) and, · part-time employees (15.3%), A positive CES-D score correlated significantly with age. |
Younger and younger employees demonstrated the highest rates of depression regardless of occupation. |
| Kafle et al. (2021). | Nepal | Web-based national cross-sectional study. Covid-19 peritraumatic Distress Index (CPDI) Questionnaire. |
254 health professionals. | · 85.4% < 30 years and the mean age of participants was 26.01(±4.46) years. · 50.04% male participants. · Hindu by religion (90.2%), · doctor by profession (42.5%), · Completed bachelor’s or master’s degree (89.8%) and working in non-governmental hospitals (72%). · works more than 4 days a week (71.1%) and, · more or equal to 40 hours a week (83.5%). |
More than half of healthcare workers were categorized as having “mild to severe distress” due to the Covid-19 pandemic. Female participants and physicians were suffering significantly more. |
| Kapetanos et al. (2021). | Greece, island of Cyprus | Multicenter cross-sectional epidemiological study. -The depression, anxiety and stress scale (DASS-21); -the Maslach Burnout Inventory (MBI). |
381 health professionals. | · 15.0% Depression, · 28.6% positive for Anxiety and, · 18.11% positive for stress. · the pandemic differentially affected the mental health of different health professionals. · prevalence of burnout was estimated at 12.3%; · strong negative association between the feeling of security with the protective measures adopted by the hospital, with the experience of burnout. There was no association between burnout and age or sex. |
The mental health of a significant portion of the workforce is compromised and therefore highlights the need for urgent intervention. The identified risk factors should provide guidance to employers with a view to protecting their frontline healthcare workers from the negative effects of the Covid-19 pandemic. |
| Mattila et al. (2021). | Finland | Multidimensional and cross-sectional research. The Generalized Anxiety Disorder 7-item (GAD-7). |
1995 health professionals. | The GAD-7 score was 4.88, indicating normal levels of anxiety. Main risk factors: · young age, · working at a teaching hospital, · cooperation problems between co-workers, · difficulty concentrating at work, · physical and psychological workload with health risk and, · Fear of being infected at work. |
Anxiety does not depend on whether the worker is directly involved in care or comes into contact with patients with Covid-19. |
| Teo et al. (2021) | Singapore | Prospective study with convenience sampling method. The 4-item Perceived Stress Scale (PSS-4); The Generalized Anxiety Disorder 7-item (GAD-7). |
2744 health professionals. | · nurses (60%), · female (81%), · lived with other people considered vulnerable (children, elderly or immunocompromised; 57%). |
Elevated perceived stress, anxiety and burnout at work were reported by 33%, 13% and 24% respectively; nurses reported the highest rates across all study outcomes. |
Source: Author (2022).
4. RESULTS AND DISCUSSION
Among the selected articles, it was found that the most used psychometric scales were: The Generalized Anxiety Disorder 7-item (GAD-7) (ALONSO et al., 2021; BHARGAVA; SARKAR; KROUMPOUZOS, 2020; MATTILA et al., 2021 ; TEO et al., 2021) and Anxiety and Stress Scale (DASS-21) (ALI et al., 2020; AYALEW et al., 2021; KAPETANOS et al., 2021).
The following methodology and/or protocol were also used: ESAE Scale (Examination of Subjective Anomalies of Experience) and Revised Impact of Events Scale (IES-R) (ALI et al., 2020); Patient Health Questionnaire (PHQ-8) (ALONSO et al., 2021); World Mental Health-International College Student-WMHICS (ALONSO et al., 2021); PTSD checklist for DSM-5 (PCL-5) (ALONSO et al., 2021); CAGEAID (ALONSO et al., 2021); Composite International Diagnostic Interview (CIDI) (ALONSO et al., 2021); Self-designed Demographic Questionnaire and Symptom Checklist 90 (SCL-90) (ZHANG et al., 2020); Standard Questionnaire and Event Impact Scale – Revised (IES-R-22) (ASNAKEW et al., 2021); Center for Epidemiological Studies Depression Scale (CES-D) (KATSUTA et al., 2021); Covid-19 Peritraumatic Distress Index (CPDI) Questionnaire (KAFLE et al., 2021); Maslach Burnout Inventory (MBI) (MATTILA et al., 2021); The 4-item Perceived Stress Scale (PSS-4) (TEO et al., 2021).
Health professionals with a psychiatric history of depression (ALI et al., 2020; BHARGAVA; SARKAR; KROUMPOUZOS, 2020; AYALEW et al., 2021; KATSUTA et al., 2021) or anxiety disorder (ALONSO et al., 2021 ; AYALEW et al., 2021; KAPETANOS et al., 2021; MATTILA et al., 2021; TEO et al., 2021) had significantly higher scores on psychometric screening scales for symptoms of anxiety and depression.
For Ali et al. (2020), anxiety is independent of whether the subject is directly involved in care or comes into contact with patients infected with Covid-19, as having a history of depression or anxiety disorder was a risk factor for the occurrence of moderate-intensity depressive symptoms severe, with psychological distress prevalent among health professionals who work in critical hospital environments.
The development of Post Traumatic Stress Disorder (PTSD) in healthcare professionals exposed to Covid-19 prevalence scenarios has been cited as an outcome in two studies (ALONSO et al., 2021; ASNAKEW et al., 2021). In the study carried out by Asnakew et al. (2021), the prevalence of post-traumatic stress disorder was found in 55.1% of the 396 health professionals interviewed.
In addition, it was found that nurses had higher scores on the psychometric scales used, which is the profession most associated with the development of psychic disorders through Covid-19, reporting that it is a risk factor for the appearance of moderate depressive symptoms to severe, moderate to severe anxiety symptoms and burnout (ALONSO et al., 2021; ZHANG et al., 2020; AYALEW et al., 2021; KATSUTA et al., 2021; TEO et al., 2021).
This stems from the fact that nurses have greater contact with patients infected by Covid-19 and work longer hours in environments where there is a risk of contamination. The medical profession was also a risk factor for the development of severe and moderate to severe depressive symptoms and anxiety symptoms (ZHANG et al., 2020; ALONSO et al., 2021; AYALEW et al., 2021; AYALEW et al., 2021; KATSUTA et al., 2021; TEO et al., 2021).
The study carried out by Ibar et al. (2021), used cortisol reference values to measure stress levels, noting that among the 12% of professionals who had burnout, 52% are doctors and residents, 19% are nurses and 19% correspond to professionals who work in the administrative sectors , technicians and maintenance.
Among the prodromal effects of depression mentioned in the analyzed studies, there was a higher occurrence of: insomnia, anxiety (ALONSO et al., 2021; KAPETANOS et al., 2021; MATTILA et al., 2021; TEO et al., 2021 ) and stress states (ALI et al., 2020; BHARGAVA; SARKAR; KROUMPOUZOS, 2020; MIRA et al., 2020; ASNAKEW et al., 2021; AYALEW et al., 2021; IBAR et al., 2021; TEO et al., 2021).
In view of the above, it is understood that Covid-19 was a risk factor for the development of moderate to severe diseases in health professionals, and it was found that working in departments related to the fight against Covid-19 was not just a risk factor for the development of generalized anxiety, but also for depression, insomnia and burnout.
5. FINAL CONSIDERATIONS
The Covid-19 pandemic, answering the guiding question, had, and still has, a negative impact on the mental health of doctors, nurses and other health professionals. Being evidenced, through the analyzed literature, greater risk of developing mental disorders in those who have a history of anxiety disorders or depression and who work in departments that act on the front line of the fight against the virus.
Thus, the early detection of psychiatric disorders and the implementation of specific strategies to ensure better mental health of health professionals are priorities in order to guarantee better patient care and quality of life for these professionals.
Therefore, it is concluded that the mental health of all professionals working on the front line in Covid-19 departments deserves special attention for the early detection of psychiatric disorders, as these present greater susceptibility and risk.
REFERENCES
ALI, Saied. et al. Psychological impact of the COVID-19 pandemic on healthcare workers at acute hospital settings in the South-East of Ireland: an observational cohort multicentre study. Bmj Open, v. 10, n. 12, p. e042930, 2020. Disponível em: https://bmjopen.bmj.com/content/bmjopen/10/12/e042930.full.pdf. Acesso em 20 fev. 2022.
ALONSO, Jordi. et al. Mental health impact of the first wave of COVID-19 pandemic on Spanish healthcare workers: A large cross-sectional survey. Revista de psiquiatria y salud mental, v. 14, n. 2, p. 90-105, 2021. Disponível: https://www.sciencedirect.com/science/article/pii/S1888989120301282. Acesso em: 20 fev. 2022.
ASNAKEW, Sintayehu. et al. Prevalence of post-traumatic stress disorder on health professionals in the era of COVID-19 pandemic, Northwest Ethiopia, 2020: a multi-centered cross-sectional study. PloS one, v. 16, n. 9, p. e0255340, 2021. Disponível em: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0255340. Acesso em: 20 fev. 2022.
AYALEW, Mohammed. et al. Prevalence and determinant factors of mental health problems among healthcare professionals during COVID-19 pandemic in southern Ethiopia: multicentre cross-sectional study. BMJ open, v. 11, n. 12, p. e057708, 2021. Disponível em: https://bmjopen.bmj.com/content/bmjopen/11/12/e057708.full.pdf. Acesso em: 18 fev. 2022.
BHARGAVA, Shashank; SARKAR, Rashmi; KROUMPOUZOS, George. Mental distress in dermatologists during COVID‐19 pandemic: Assessment and risk factors in a global, cross‐sectional study. Dermatologic Therapy, v. 33, n. 6, p. e14161, 2020. Disponível em: https://onlinelibrary.wiley.com/doi/full/10.1111/dth.14161. Acesso em: 20 fev. 2022.
CORLEY, Amanda; HAMMOND, Naomi E.; FRASER, John F. The experiences of health care workers employed in an Australian intensive care unit during the H1N1 Influenza pandemic of 2009: a phenomenological study. International journal of nursing studies, v. 47, n. 5, p. 577-585, 2010. Disponível em: https://www.sciencedirect.com/science/article/pii/S002074890900371X. Acesso em: 12 mar. 2022.
GOULIA, Panagiota. et al. General hospital staff worries, perceived sufficiency of information and associated psychological distress during the A/H1N1 influenza pandemic. BMC infectious diseases, v. 10, n. 1, p. 1-11, 2010. Disponível em: https://bmcinfectdis.biomedcentral.com/articles/10.1186/1471-2334-10-322. Acesso em: 12 mar. 2022.
IBAR, Carolina. et al. Evaluation of stress, burnout and hair cortisol levels in health workers at a University Hospital during COVID-19 pandemic. Psychoneuroendocrinology, v. 128, p. 105213, 2021. Dsiponível em: https://www.sciencedirect.com/science/article/pii/S0306453021000871. Acesso em: 21 fev. 2022.
IMAI, Hissei. et al. Factors associated with motivation and hesitation to work among health professionals during a public crisis: a cross sectional study of hospital workers in Japan during the pandemic (H1N1) 2009. BMC public health, v. 10, n. 1, p. 1-8, 2010. Disponível em: https://link.springer.com/article/10.1186/1471-2458-10-672. Acesso em: 12 mar. 2022.
KAFLE, Khagendra. et al. Psychological distress among health service providers during COVID-19 pandemic in Nepal. PLoS One, v. 16, n. 2, p. e0246784, 2021. Disponível em: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0246784. Acesso em: 23 fev. 2022.
KAPETANOS, Konstantinos. et al. Exploring the factors associated with the mental health of frontline healthcare workers during the COVID-19 pandemic in Cyprus. PloS one, v. 16, n. 10, p. e0258475, 2021. Disponível em: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0258475. Acesso em: 18 fev. 2022.
KATSUTA, Narimasa. et al. Elevated depressive symptoms among newer and younger healthcare workers in Japan during the COVID‐19 pandemic. Neuropsychopharmacology Reports, 2021. Disponível em: https://onlinelibrary.wiley.com/doi/full/10.1002/npr2.12217. Acesso em: 18 fev. 2022.
KHANAL, Pratik. et al. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Globalization and health, v. 16, n. 1, p. 1-12, 2020. Disponível em: https://psycnet.apa.org/record/2021-51602-023. Acesso em: 12 mar. 2022.
KOLA, Lola. et al. COVID-19 mental health impact and responses in low-income and middle-income countries: reimagining global mental health. The Lancet Psychiatry, v. 8, n. 6, p. 535-550, 2021. Disponível em: https://psycnet.apa.org/record/2021-51602-023. Acesso em: 12 mar. 2022.
KRISHNAMOORTHY, Yuvaraj. et al. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry research, v. 293, p. 113382, 2020. Disponível em: https://psycnet.apa.org/record/2021-51602-023. Acesso em: 12 mar. 2022.
MATTILA, Elina. et al. COVID-19: anxiety among hospital staff and associated factors. Annals of medicine, v. 53, n. 1, p. 237-246, 2021. Disponível em: https://www.tandfonline.com/doi/full/10.1080/07853890.2020.1862905. Acesso em: 25 fev. 2022.
MATSUISHI, Kunitaka. et al. Psychological impact of the pandemic (H1N1) 2009 on general hospital workers in Kobe. Psychiatry and clinical neurosciences, v. 66, n. 4, p. 353-360, 2012. Disponível em: https://onlinelibrary.wiley.com/doi/pdfdirect/10.1111/j.1440-1819.2012.02336.x. Acesso em: 12 mar. 2022.
MIRA, José Joaquín. et al. Acute stress of the healthcare workforce during the COVID-19 pandemic evolution: a cross-sectional study in Spain. BMJ open, v. 10, n. 11, p. e042555, 2020. Disponível em: https://bmjopen.bmj.com/content/bmjopen/10/11/e042555.full.pdf. Acesso em: 20 fev. 2022.
MOHER, David. et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic reviews, v. 4, n. 1, p. 1-9, 2015. Disponível em: https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/2046-4053-4-1/. Acesso em: 20 fev. 2022.
ORNELL, Felipe. et al. “Pandemic fear” and COVID-19: mental health burden and strategies. Brazilian Journal of Psychiatry, v. 42, p. 232-235, 2020. Disponível em: https://doi.org/10.1590/1516-4446-2020-0008. Acesso em: 12 mar. 2022.
SPOORTHY, Mamidipalli Sai; PRATAPA, Sree Karthik; MAHANT, Supriya. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian journal of psychiatry, v. 51, p. 102119, 2020. Disponível em: https://www.sciencedirect.com/science/article/pii/S1876201820302306. Acesso em: 12 mar. 2022.
TEO, Irene. et al. Healthcare worker stress, anxiety and burnout during the COVID-19 pandemic in Singapore: A 6-month multi-centre prospective study. PloS one, v. 16, n. 10, p. e0258866, 2021. Disponível em:
ZHANG, Wen-rui. et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychotherapy and psychosomatics, v. 89, n. 4, p. 242-250, 2020. Disponível em: https://www.karger.com/Article/PDF/507639. Acesso em: 12 mar. 2022.
[1] Post-graduated in Psychiatry, by IPEMED, city of São Paulo/SP. Graduated from the Faculty of Medicine of Vale do Aço – UNIVAÇO, Ipatinga – Minas Gerais. ORCID: 0000-0001-7660-7077.
Sent: April, 2022.
Approved: May, 2022.















