ORIGINAL ARTICLE
SILVA, Ítalo Fernando Penha da [1], SERRUYA JÚNIOR, José Maria Henriques [2], GÓES, Tayonara Borges Gonçalves [3], NORONHA, Bruno Gomes de [4], DIAS, Cláudio Alberto Gellis de Mattos [5], DENDASCK, Carla Viana [6], OLIVEIRA, Euzébio de [7], FECURY, Amanda Alves [8]
SILVA, Ítalo Fernando Penha da. Et al. Antimicrobial Sensitivity Profile Of Uropathogens In A Macapá Laboratory, Amapá, Brazilian Amazon. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year 06, Ed. 02, Vol. 04, pp. 81-102. February 2020. ISSN: 2448-0959, Access link: https://www.nucleodoconhecimento.com.br/health/antimicrobial-sensitivity, DOI: 10.32749/nucleodoconhecimento.com.br/health/antimicrobial-sensitivity
SUMMARY
Urinary tract infections (UTI) represent a worldwide health problem. Microbial resistance, due to selective antibiotic pressure, has a direct influence on the evolution and impact of these infections. The objective of this work was to identify the antimicrobial susceptibility profile of uropathogens isolated in uroculture samples from a private laboratory in the city of Macapá/AP. It is a quantitative, retrospective and cross-sectional study, using a laboratory database. Data were collected from results of urocultures with antibiogram analyzed from January to December 2019. The present study evaluated 3,510 urocultures, carried out during the study period, of which 1,269 had bacterial growth, equivalent to 36.15%. Among the positive results, we found the bacteria Escherichia coli (66.59%), Staphylococcus aureus (32.62%), mixed colonies of E. coli and S. aureus (0.47%), Staphylococcus saprophyticus (0.24%) and Serratia marcescens (0.08%). The male gender was responsible for 16.35% (n = 574) of the urocultures analyzed, while the female population was 83.65% (n = 2936). When analyzing the distribution of bacteria isolated by gender, males were considered a protective factor with 42% less chance of presenting bacteria in urine. The bacteria E. coli was the predominant pathogen in these infections in both sexes and in all age groups.
Keywords: Uroculture, Sensitivity, Resistance, Antimicrobials, Antibiotics, Amazon.
INTRODUCTION
Urinary tract infection (UTI) means the inflammatory response in the urinary tract (urethra, bladder, kidney or prostate), determined by a microbial agent (bacteria and/or virus and/or fungus and/or parasite) with clinical manifestations ranging from asymptomatic bacteriuria to septic shock. The type of UTI Can be classified through its anatomical location: high or low, symptomatic or asymptomatic, complicated or uncomplicated, recurrent or sporadic (JÚNOR et al; 2010).
In the United States, they accounted for approximately 2% of consultations with emergency services in 2014, totaling 2.3 million people (WIJTING, 2019). In Brazil, ITUs are considered the most common of bacterial infections, responsible for 80 out of every 1,000 clinical consultations, and may have particularities between the sexes (OLIVEIRA; SANTOS, 2018). It is estimated that almost half of women will experience at least one episode of cystitis during their lifetime and a third of them before the age of 24 (EAU, 2018).
The most common etiological agent is Gram-negative bacteria, with Escherichia coli being the most frequent. Other bacteria involved are Proteus mirabilis, Klebsiella pneumoniae, Pseudomonas aeruginosa, Enterococcus spp., Enterobacter spp., Group B streptococcus and Staphylococcus saprophyticus (CUNHA et al, 2016).
The diagnosis of ITUs is made based on the clinical signs and symptoms presented by the patient and the analysis of the urine sample, confirming the presence of significant leukocyria and bacteria (MARTINS et al, 2016). The high incidence of these infections and the need to start treatment before the results of microbiological findings become available often lead to the adoption of empirical therapy (CUNHA et al, 2016).
Although the benefits of antibiotic use are clear, their misuse or overuse have contributed to the growing problem of resistance among uropathogenic bacteria, which is a serious threat to public health. In emergency services, 20-50% of the prescribed antibiotics proved unnecessary or inappropriate (EAU, 2018). Unlike other drugs, the unmanaged use of antimicrobials has a negative impact not only on the patient who receives them, but also on the ecosystem, when selecting multidrug-resistant pathogens (BRASIL, 2019).
The Global Monitoring Report on Antibiotic Resistance released by the World Health Organization showed that increased resistance of major bacteria to cephalosporins and fluoroquinolones is a serious health problem worldwide (KANG et al, 2018).
All this exposure increases the risk of adverse events, unwanted drug interactions, acquisition of concomitant infections by other multidrug-resistant pathogens, fungi and Clostridium difficile, in addition to the significant increase in care costs (direct and indirect) (BRASIL, 2019).
National and international studies have shown greater resistance to commonly used antimicrobials. In addition, knowledge of the resistance pattern of uropathogens is important to guide the ideal antimicrobial choice in the patient’s initial approach, because variations in the microbial spectrum and susceptibility patterns may occur in different regions, and the previous use of antimicrobials is an important predictor of resistance (CUNHA et al, 2016; OLIVEIRA et al., 2020).
However, national and international studies have demonstrated increasing resistance to commonly used antimicrobials, resulting from a change in the bacterial profile, directly reflecting on the quality of care provided. This resulted in global initiatives for prevention and control of microbial resistance in health services in order to direct strategies and actions to detect, prevent and control the spread of resistant microorganisms (BRASIL, 2019).
Among these measures, identifying the most common pathogens in the community, as well as their sensitivity profile to the use of antimicrobials, aims to ensure the maximum pharmacotherapeutic effect; reduce the occurrence of adverse events in patients; prevent the selection and spread of resistant microorganisms and reduce care costs.
GOAL
To identify the most frequent uropathogens in urocultures, as well as their antibiotic sensitivity profile in outpatients in Macapá, Amapá, Brazil, aiming at improving the effectiveness in the initial approach to the patient.
METHODOLOGY
This is a quantitative, retrospective and cross-sectional study. Data from patients who had uroculture analyzed from January 2019 to December 2019 were used at the Dr. Paulo J. Albuquerque Medical Laboratory, located at Avenida Leopoldo Machado, Centro, Macapá-AP, Brazil. Data were collected and organized in February and March 2020 and correspond to the production of tests with uroculture and antibiogram for diagnosis of UI. The information was obtained through consultation with the laboratory’s test records database, using the results of urocultures from the outpatient clinic, ward or community. Initially, the information was organized by using Microsoft Excel 2010 and was analyzed and processed by the BIOESTAT 5.0 tool. Data from patients of both sexes and all age groups who performed urocultures in this laboratory from January 2019 to December 2019 were included in the study.
This study was approved by the Research Ethics Committee (CEP/UNIFAP) under registration No. 4,203,509 and the collected data will be used only for the purposes of this study, preserving the anonymity of the sample population.
RESULTS
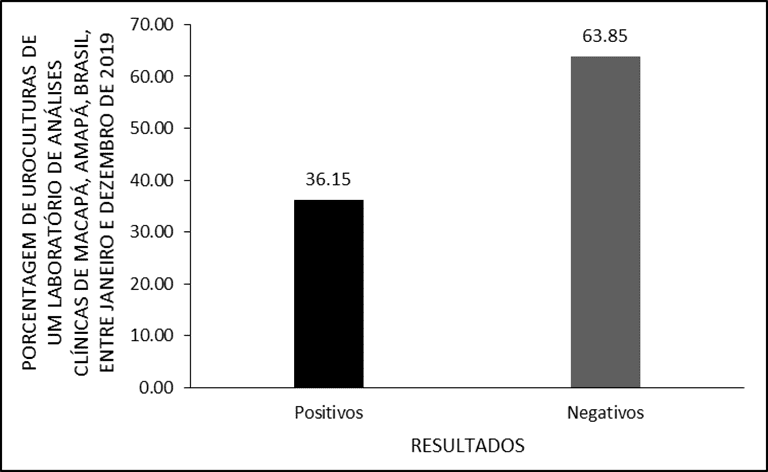
The present study evaluated 3,510 urocultures, carried out between January and December 2019 in a clinical analysis laboratory in the city of Macapá, Amapá, Brazil, of which 1,269 had bacterial growth, equivalent to 36.15% (Figure 1).
Figure1 Results of urocultures from a clinical analysis laboratory in the city of Macapá/AP, from January to December 2019.
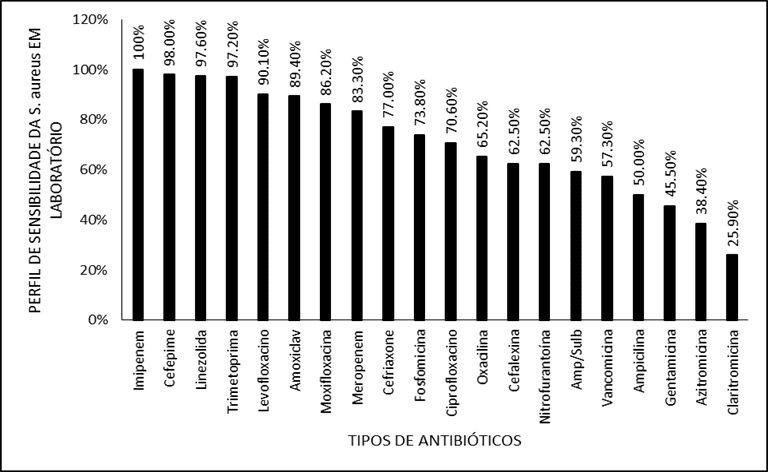
Among the positive results, we found the bacteria Escherichia coli (66.59%), Staphylococcus aureus (32.62%), mixed colonies of E. coli and S. aureus (0.47%), Staphylococcus saprophyticus (0.24%) and Serratia marcescens (0.08%) represented in Table 1.
Table 1. Bacteria isolated in urocultures from a clinical analysis laboratory in the city of Macapá/AP from January to December 2019
The male gender was responsible for 16.35% (n = 574) of the urocultures analyzed, while the female population was 83.65% (n = 2936). When analyzing the distribution of bacteria isolated by gender, males were considered a protective factor with 42% less chances of presenting bacteria in urine (Odds Ratio = 0.58[IC 0,480-0,716] p<0.05) and females were shown to be a risk factor with 1.7 times more chances of having positive results (p<0.05). However, there was no association when comparating the risk of infection specifically by E. coli or S. aureus in each genus (OR = 0.765[IC: 0,537-1,090] p = 0.137). The bacteria S. saprophyticus, S. marcescens and mixed colonies were excluded from these calculations, as they did not represent a significant sample.
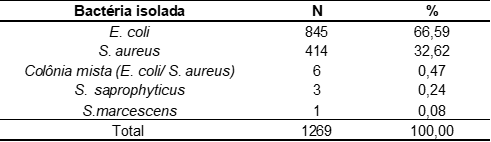
The age of the patients varied between 1 and 106 years, the mean age in the sample studied was 41 and the median was 39 years. Moreover, the population with positive results had a mean and median age higher than the population with negative result, 42 and 38 years, respectively. The distribution by age group of the studied population was described in Table 2.
Table 2. Age distribution of the studied population from an analysis laboratory in the city of Macapá/AP, from January to December 2019.
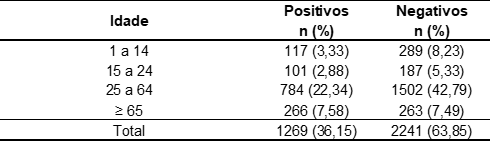
As shown in table 3, the age group between 25 and 64 years concentrated the majority of positive cases with 61.47% (n = 784) in the general population.
Table 3. Age distribution in patients according to bacteria isolated individually from an analysis laboratory in the city of Macapá/AP, from January to December 2019.
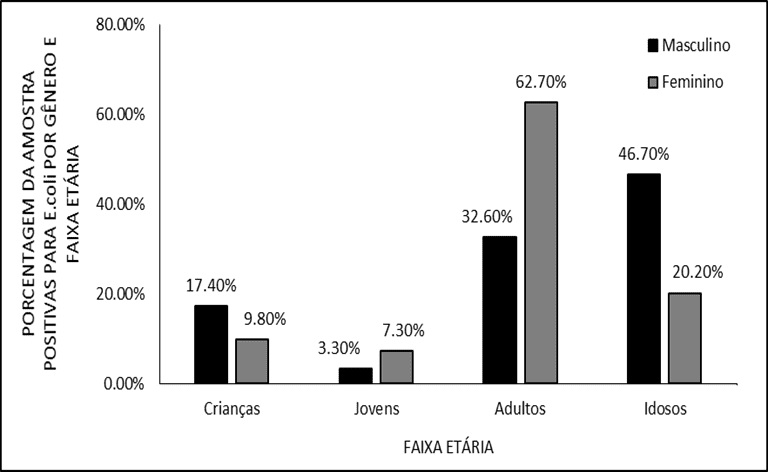
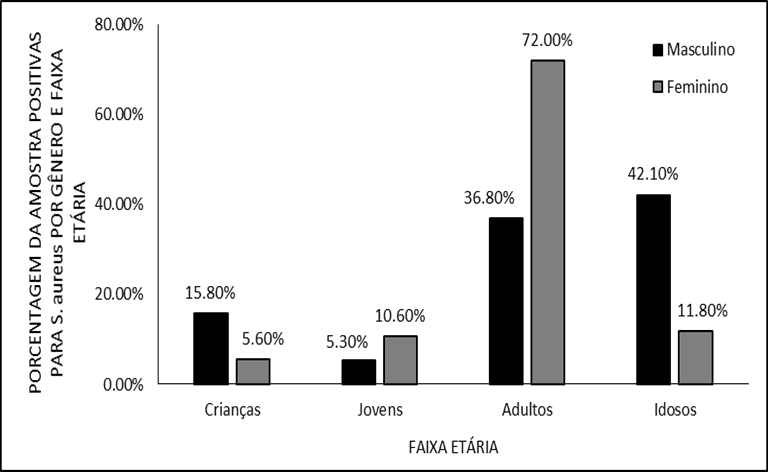
Observing each gender in isolation, women were more affected between 25 and 64 years (E. coli 62,7%; S. aureus 72,0%) while in males, elderly patients (> 64 years) had a higher number of cases (E. coli 46.7%; S. aureus 42.1%). These results had statistical significance (p<0.05) and are represented in figures 2 and 3.
Figure 2. Distribution of positive samples for E. coli by gender and age group.
Figure 3. Distribution of positive samples for S. aureus by gender and age group.
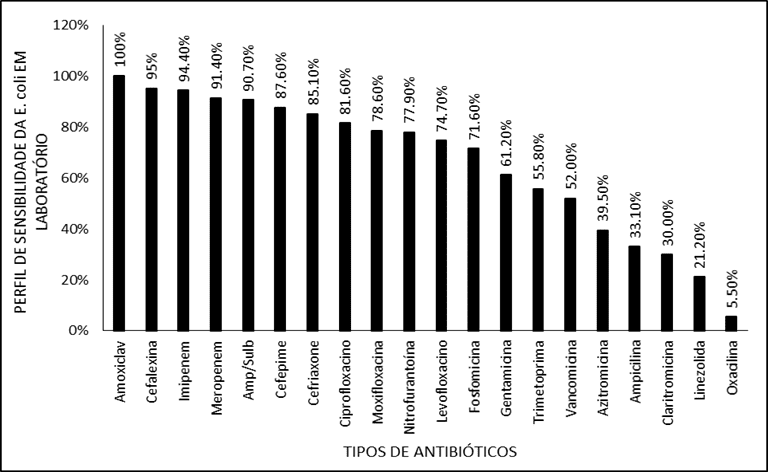
Among the positive results for E. coli, 20 antibiotics prevalent in clinical practice were tested, these are listed in Table 4.
Table 4. Antimicrobial sensitivity and resistance profile of E bacteria. coli (n = 845) in antibiograms from a clinical analysis laboratory in the city of Macapá/AP
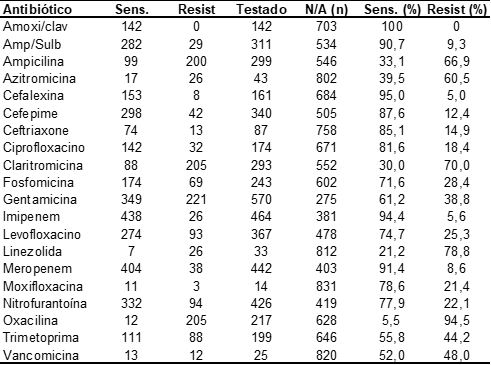
Antibiotics with the highest sensitivity rate against E. coli. were: Amoxicillin with clavulanate (100.0%), Cephalexin (95.0%), Imipenem (94.4%), Meropenem (91.4%), Ampicillin with Sulbactan (90.5%) and Cefepime (87.5%). The distribution in decreasing order of sensitivity was represented in Figure 4.
Figure 4. Shows the profile of E. coli sensitivity to different antibiotics in the laboratory.
Among the positive results for S. aureus, 20 antibiotics prevalent in clinical practice were tested, which are listed in Table 5.
Table 5. Antimicrobial sensitivity and resistance profile of s. aureus (n = 414) in antibiograms from a clinical analysis laboratory in the city of Macapá/AP
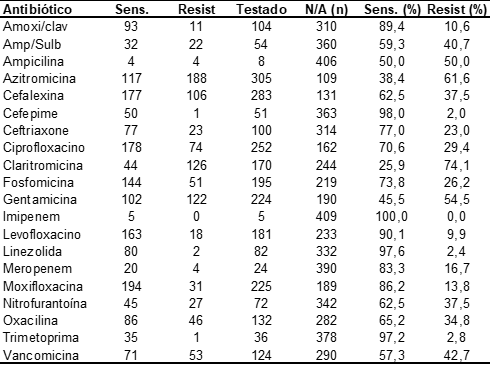
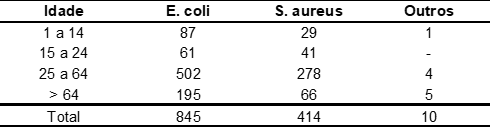
The antibiotics with the highest sensitivity index were: Imipenem (100.0%), Cefepime (98.0%), Linezolid (97.6%), Trimethoprima (97.2%), Amoxicilline with clavulanate (89.4%) and Levofloxacin (90.1%) The distribution in decreasing order of sensitivity was represented in Figure 5.
Figure 5 Shows the sensitivity profile of E. coli to different antibiotics in the laboratory.
DISCUSSION
The etiology and profile of bacterial resistance in urocultures of patients treated in a community according to age and gender are important in the decision of empirical antimicrobial therapy. The 36.15% positive results obtained in the research have similar reports in several authors.
Santos et al. (2017) found 25.7% positive results of culture test with antibiogram in a private laboratory in São Paulo. In 2019, at the Central Laboratory of Public Health of Macapá (LACEN), researchers analyzed 2,078 tests and found 13.9% positive urocultures (SANTOS; PORCY; MENEZES, 2019). Similarly, in a laboratory in Santa Catarina, 3,232 tests were analyzed, where 16% of patients obtained positive results for urinary infection (MACHADO et al, 2019). In Ceará, in a laboratory that attended the hospital and community population, a total of 835 samples were observed with 26.52% of the positive analyses (FIGUEREDO; CRUZ; PITA, 2020).
Researchers from a pediatric hospital in Pará analyzed 2,222 urocultures in children under 10 years of age with 9% positive (BRÍGIDO, 2020). Divergent result from that found by Marks et al. (2020) in a pediatric hospital in Santa Catarina, which obtained 46.2% of positive urocultures. Higher values were found in the Intensive Care Unit at the Municipal Hospital of Santarém/PA, with positive uroculture rates of 63.4%. In general, hospital units are expected to record a higher prevalence of positive urocultures when compared to laboratories where users come from the community (TIAGO et al, 2020).
About its population, the present study observed greater involvement in females (88% of the positive results), and the age group between 15 and 64 years was more affected. A result similar to those found in the studies by Machado et al (2019), Brambilla et al (2019), Santos et al (2017), Cunha et al (2016) and Araújo e Queiroz (2012) who reported 88.2%, 89.7%, 84%, 79%, 78% of involvement among women, respectively. However, a smaller proportion was observed in the works of Santos, Porcy and Menezes (2019) and Bail et al (2017) with 55% and 56% each. According to Nóbrega (2015), UTI is the most frequent urological disease among women and can manifest in any age group.
Behavioral factors predominate in menacme, such as the number of partners, frequency of sexual intercourse, use of diaphragm and spermicides. Genetics and pelvic anatomy also play an important role since maternal history of recurrent UTI, previous case of UTI before 15 years of age and a shorter distance between the urethra and the anus are reported as risk factors. In postmenopausal, other alterations are highlighted, such as estrogen deficiency, decreased vaginal lactobacilli, cystocele, urogenital surgery, elevated post-voiding residual volume and previous UTI (HADDAD; FERNANDES, 2018).
According to Marks et al (2020), the highest female prevalence in UTI occurs from the first year of life, because before that and especially in the first three months, it is more common in males. It is believed that it is due to the mucosa of the foreskin favoring bacterial adhesion and ureteral vesico reflux that may be present at this age in boys. However, in the case of infection in the hospital environment, men and women are affected in a variable way depending on the risk factors that are associated and also on the immunosuppressive state of each patient (JORGE; VIDAL, 2014).
In this study, males accounted for 12% of the positive samples, with the age group over 64 years being the most affected. According to Fernandes (2020), the higher prevalence in the elderly population is justified by the increase in prostate volume that results in the inability to completely empty the bladder. Other structural changes such as urethra stenosis, urinary tract tumors and benign prostatic hyperplasia, as well as the presence of urethal probes, eliminate the inherent defense mechanisms of the individual, such as urination and proper emptying of the bladder, facilitating the entry of intraluminal microorganisms into this closed system.
In the present study, E. coli was the most prevalent pathogen (66.59%) followed by S. aureus (32,62%). Meanwhile, mixed colonization, S. saprophyticus and S. marcescens accounted for < 1.0% each. This result is similar to a study conducted in the same laboratory in Macapá in the period of 2017 that reported the presence of E. coli (65.4%), S. aureus, (31.5%) and Staphylococcus sp, (3.1%) in their samples. In relation to the predominant bacterium, both studies have values similar to those found in the national and international literature (RODRIGUES et al., 2016; CASTILLO et al, 2019).
In Santa Catarina, Machado et al. (2019) observed E. coli (62.4%), followed by Proteus sp. (17,3%), Klebsiella sp. (10,4%), Estafilococos sp. (8,9%) e Pseudomonas sp. (1%). In a laboratory in Paraná, was found E. coli (60%), followed by Klebsiella pneumoniae (12%), Morganella morganii (4%), Enterococcus sp (4%), Aeromonas hydrophila (4%) and Citrobacter koseri (4%) (BRAMBILLA, 2019). A study, conducted at the Central Laboratory of Rio Grande do Norte, found E. coli responsible for 60.4%, Klebsiella spp. (14.2%), Staphylococcus spp. (7.2%), e Proteus spp. (4.8%) (CUNHA et al., 2016).
In a hospital setting, Bail et al. (2019) described E. coli accounting for 56.7% of cases, followed by Klebsiella spp. with 13.5%. Other enterobacteria detected were Proteus mirabilis (4.8%), Enterobacter spp (2.9%), Citrobacter spp (2.9%), Pantoea agglomerans (1%) and Serratia marcescens (1%). Figueredo et al. (2020) observed, in the hospital scope, E. coli (40,52%); Klebsiella sp. (15,26%); Enterobacter sp. (14,73%); Streptococcus agalactiae (10%) e Proteus sp. (9,47%).
Tiago et al (2020), in a pediatric population in Pará, observed E. coli with 53.8%, Proteus mirabilis with 13.5%, Klebsiella pneumoniae with 9.6%, Pseudomonas aeruginosa with 9.6% and Staphylococcus epidermidis with 5.8% of positive cases.
A multicenter study involving nine European countries and Brazil (ARESC Study) evaluated 3,018 cases of urinary infection in women; the highest prevalence was E. coli (76.7%), followed by Enterococcus faecalis (4%), Staphyloccocus saprophyticus (3.6%), Klebsiella pneumoniae (3.5%) and Proteus mirabilis (3.5%) (NABER, 2008).
In the Northern Dimension Antibiotic Resistance Study (NoDARS), Finland, Germany, Latvia, Poland, Russia, and Sweden collected urine samples from ambulatory women with symptoms of uncomplicated urinary infection and found E. responsible in 77.2% of cases (NY et al, 2019).
In the literature most of the isolated microorganisms belong to the Enterobacteriaceae family, human gut residents and considered important causes of UTI, blood infections, hospital, pneumonias and various intra-abdominal infections. E. coli is the pathogen most often associated with UIs for all syndromes and age groups where its transmission is made by direct contact person by person and fecal-oral route. Originating from the intestinal microbiota, it is adesed and colonized through the fibrias and adhesins, hindering its elimination through urinary flow (BAIL et al 2019).
The second most prevalent pathogen in this study, S. aureus (32.62%), is a gram-positive bacterium and has great adaptation to environmental conditions and can survive acidic, basic and dry sites. These microorganisms are facultative anaerobic bacteria and have a great impact on public health, being an important cause of infections in humans and other animals. It is often found in human narins and skin and its relationship with UT in general is related to health care (FRANÇA et al, 2020). The high proportion found in this study differs from much of the literature and may be a consequence of contamination of samples during the collection procedure performed by manual method (CASTILLO et al, 2019).
Polymicrobial urinary tract infections are infrequent. The presence of two or more bacteria in the culture raises doubts regarding the reliability of the test and generates the suspicion of possible contamination of the sample. Confirmation of the diagnosis should be performed with the acquisition of serial urine samples, observing the presence of the same pathogens in subsequent samples (FIGUEREDO; CRUZ; PITA, 2020).
Antibiotic resistance has become one of the most important public health problems worldwide. This increase, observed since the last years of the century, generated a global movement with the aim of limiting its potentially catastrophic effects. The consequences of antibiotic resistance are difficult to predict, but it is estimated that by 2050 it will be the cause of death of about ten million people and will assume a huge economic cost (ALFAYATE, MIGUELEZ; GARCIA-MARCOS, 2020).
The present study evaluated susceptibility to several common antibiotics in medical practice. The bacterium E. coli was sensitive to beta-lactams: amoxicillin with clavulanate (100.0%), cephalexin (95.0%), ampicillin and sulbactan (90.5%) – with low sensitivity to ampicillin alone (33%) – and 3rd and 4th generation cephalosporins had 85% and 87%. In addition, more than 90% of the cultures were sensitive to carbapenems. Sensitivity to fluoroquinolones was varied: Ciprofloxacin (81.4%), moxifloxacin (78%) and levofloxacin (74.7%). Drugs of choice in most guidelines, such as nitrofurantoin and phosphomycin, showed moderate sensitivity with 77.9% and 71.6%, respectively. Macrolides have been shown to be of low efficacy (<40%), even included in antibiograms, these drugs have no role in the treatment of UTIs.
Although this study showed a good action profile of beta-lactams, it is important to highlight that these drugs are losing their effectiveness due to extended spectrum beta-lactamases (ESBL) producing strains. Ny et al (2018), Kim et al (2015) and Zavala-Cerna et al (2020) found a prevalence of 8.7%, 25.6% and 24.6% in their studies. The mechanism of resistance is essentially due to plasmid-mediated transmission of genes encoding these enzymes.
Ampicillin resistance is already described in several studies, however, despite the high rate of resistance, this drug is considered first-line therapy for susceptible bacteria in pregnant women because of its safety profile (MACHADO, 2018; BAIL, 2019; BRÍGIDO, 2020). In this work, it was noticed that the addition of beta-lactamase inhibitors was sufficient to improve the action profile of this class of medication. The total understanding of the types of beta-lactamases produced by the strains and their action profile still generates many doubts in the scientific community, since it is not known how the general profile of bacterial pathogens will respond to the clinical application of the new wave of beta-lactamase inhibitors (TOOKE, 2019).
It is the guidance of the European Association of Urology that aminopenicilins be used only in exceptional situations, such as in the treatment of complicated UTI, where they should be associated with other classes of antibiotic; while 3rd and 4th generation cephalosporins should be reserved for cases of pyelonephritis and urosepse (UAE, 2018).
Fluoroquinolones are widely used in the empirical treatment of UTI, including cases of high urinary tract infections. In a major literature review, Lee et al (2016) pointed out that in Japan and Australia the susceptibility of E. coli to these drugs was approximately 90%; in the USA between 70~88% and in China 74~84%. In addition, in northern European countries 80% was found, while other European and some Mediterranean regions showed approximately 60% susceptibility. Ny et al (2018), in Russia and Eastern Europe, showed sensitivity of 85%. In Brazil we also found varied results regarding the sensitivity of E. coli às fluoroquinolonas: Marks et al (2020) 96%, Brígido et al (2020) 85%, Machado et al (2019) 83%; while Cunha et al (2016) 75%, Figueredo et al (2020) 71%; Bail et al (2020) 61%; Tiago et al (2020) 54,6%.
According to Lee et al (2016), the susceptibility of gram-negative bacteria to ciprofloxacin was much higher in patients under 20 years of age than in older patients. The reason for this observation may be the lower exposure to fluoroquinolones in young individuals, since these drugs do not have a good safety profile in the pediatric population.
No national or international guideline recommends the use of quinolonas as a first-line in patients with uncomplicated urinary infection. In addition, it is determined that there is significant increase in the manifestation of serious side effects on musculoskeletal systems. In this respect, the use of these drugs is outlawed in conditions such as: management of self-limiting infections, patients with a history of adverse effects, solid organ transplants or those who make continuous use of corticosteroids because in these groups the risk of tendinitis and tendon rupture is exacerbated (ANVISA, 2018). A similar report was issued by the European Medicine Agency which suspended advertising, restricted use and suggested increased surveillance of healthcare professionals in the adverse effects of quinonines (EMA, 2019)
Although the results of this study demonstrated moderate sensitivity to phosphomycin (71.6%) and nitrofurantoin (77.9%), for more than a decade they have been considered antimicrobials of choice for empirical treatment of uncomplicated acute cystitis (GUPTA et al, 2011). Phosphomycin inhibits peptidoglycan synthesis at an earlier stage than beta-lactam antibiotics or glycopeptides and has a broad spectrum of activity, including E. esbl-producing coli. Nitrofurantoin, on the other hand, acts by damaging bacterial DNA in its highly active reduced form. Naber et al (2008), in Brazil and Europe, found sensitivity of 87% and 96.4% for phosphomycin and nitrofurantoin, respectively. Even today after the popularization of its use, resistance is low 0-5% (LEE et al, 2016). In Russia and Eastern Europe, sensitivity to nitrofurantoin and phosphomycin were 98.8% and 98.7% (NY et al, 2018); in our country, Machado et al (2018) identified that sensitivity was 95.1% and 97.5% and Cunha et al (2016) found more than 92%.
The present study observed sensitivity to sulfamethoxazole-trimethoprim in only 55.8%. This drug has been used for more than 30 years as first-line therapy for UIs and prophylaxis of recurrent cystitis. However, antimicrobial resistance to this agent has been increasing over the years, approaching 18-22% in some areas of the United States and Europe. The ARESC study (NABER, 2008) already observed high rates of Resistance of E. coli to sulfamethoxazole-trimethoprim (29%), confirmed by recent studies in Russia and South Korea (NY et al, 2018) and by Kim et al (2015) who reported resistance between 22-32.6% and 39.4%. In Brazil, Machado et al (2018), Bail et al (2019), Figueredo et al (2020) and Castillo et al (2019) found 25%, 35.7%, 39.5% and 62% respectively making their empirical use questionable. Still, it is reported that its sensitivity profile has been increasing in recent years due to the reduction in its prescription (KANG et al, 2018).
Several global initiatives have warned of the rational use of antibiotics suggesting the implementation of local education programs, control in the prescription and sale of antibiotics and support in the implementation of guidelines for the management of infectious diseases. Who stated that only antibiotics holding antimicrobial sensitivity tests (TSAs) greater than 80% should be prescribed. Therefore, any drug with a resistance rate greater than or equal to 20% should not be administered empirically given the inefficacy and induction of the emergence of new resistant bacteria (FIGUEREDO; CRUZ; PITA, 2020; CUNHA, 2016; DORON & DAVIDSON, 2011; GUPTA et al, 2011).
The duration of treatment has also been debated in recent years, recent guidelines recommend single-dose treatment or shorter regimens, up to 5 days. A systematic review showed that there was no difference in symptom improvement between 3-day regimens and 5 to 10 days of antibiotic use in women with uncomplicated cystitis. Longer treatments are subject to more side effects and abandonment by the user, however they are related to lower recurrence in the short term (MILO et al, 2005).
CONCLUSIONS
Urinary tract infections are still a public health problem given their high incidence in the population. Women of reproductive age are the most affected due to anatomical and behavioral factors, but the prevalence increases in men after the 6th decade of life.
The E. coli bacteria was the predominant pathogen in these infections in both sexes and in all age groups. The resistance profile of this bacterium has some particularities at the local level, such as good sensitivity to beta-lactams and moderate sensitivity to nitrofurantoin and phosphomycin. The results presented show the need for uroculture and TSA for the therapy to be adequate and effective, avoiding the improper prescription of medications, which in addition to not treating the infection can induce bacterial resistance.
Developing research that explores the epidemiological profile of the region is important because it provides a theoretical framework for the medical community to base its therapeutic decisions considering the local resistance pattern, resulting in better care, reducing morbidity and recurrence of these infections.
REFERENCES
ALFAYATE MIGUELEZ, Santiago; GARCIA-MARCOS, Luis. Rational use of antimicrobials in the treatment of upper airway infections. J. Pediatr. (Rio J.), Porto Alegre , v. 96, supl. 1, p. 111-119, Mar. 2020
ARAÚJO, K.L; QUEIROZ, A.C; Análise do perfil dos agentes causadores de infecção do trato urinário e dos pacientes portadores, atendidos no Hospital e Maternidade Metropolitano-SP. J Health Sci Inst., v.30, n.1, p.7-12, 2012.
BAIL, Larissa et al. Perfil de sensibilidade de bactérias isoladas em uroculturas de pacientes atendidos em um hospital brasileiro. Cadernos da Escola de Saúde, v. 17, n. 2, p. 52-60, 2017.
BRAMBILLA, Gabriela Gonçalves; DA SILVA ECKER, Alessandra Barrochelli. Incidência de microrganismos em infecções no trato urinário e sua relação com o antibiograma em um laboratório da região do noroeste do paraná. REVISTA UNINGÁ, v. 56, n. 4, p. 85-97, 2019.
BRASIL, ANVISA. Agência Nacional de Vigilância Sanitária. PROJETO STEWARDSHIP BRASIL. Avaliação Nacional dos Programas de Gerenciamento do Uso de Antimicrobianos em Unidade de Terapia Intensiva Adulto dos Hospitais Brasileiros. Gerência de Vigilância e Monitoramento em Serviços de Saúde. Gerência Geral de Tecnologia em Serviços de Saúde. Brasília-DF, 2019.
BRASIL, ANVISA – Agência Nacional De Vigilância Sanitária. Risco de efeitos colaterais graves incapacitantes e potencialmente irreversíveis e restrições no uso – quinolonas e fluoroquinolonas sistêmicas e inalatórias. 2018.
BRÍGIDO, Heliton Patrick Cordovil et al. Perfil de resistência de agentes de infecção urinária em crianças internadas em um hospital de pediatria em Belém do Pará. Brazilian Journal of Health Review, v. 3, n. 4, p. 9808-9818, 2020.
CASTILLO, Naiara Campos Paixão de. et al. Resistência Bacteriana em Uroculturas de mulheres em Macapá: comparação dos resultados ambulatoriais e hospitalares. Revista Científica Multidisciplinar Núcleo do Conhecimento. Ano 04, Ed. 10, Vol. 13, pp. 128-165. Outubro de 2019. ISSN: 2448-0959
CUNHA, M. A., ASSUNÇÃO, G. L., MEDEIROS, I. M., & FREITAS, M. R. (2016). ANTIBIOTIC RESISTANCE PATTERNS OF URINARY TRACT INFECTIONS IN A NORTHEASTERN BRAZILIAN CAPITAL. Revista do Instituto de Medicina Tropical de São Paulo, 58, 2. doi:10.1590/S1678-9946201658002
DORON, S., & DAVIDSON, L. E. (2011). Antimicrobial stewardship. Mayo Clinic proceedings, 86(11), 1113–1123. https://doi.org/10.4065/mcp.2011.0358.
EAU GUIDELINES. Edn. presented at the EAU Annual Congress Copenhagen 2018. ISBN 978-94-92671-01-1. EAU Guidelines Office, Arnhem, The Netherlands.
European Medicines Agency (EMA). Disabling and potentially permanent side effects lead to suspension or restrictions of quinolone and fluoroquinolone antibiotics. 11 March 2019 EMA/175398/2019. Disponível em <https://www.ema.europa.eu/en/documents/referral/quinolone-fluoroquinolone-article-31-referral-disabling-potentially-permanent-side-effects-lead_en.pdf> Acesso em 12 out 2020.
FERNANDES, Thaís Siqueira. Infecção do trato urinário no idoso: revisão de literatura. Repositório de Trabalhos de Conclusão de Curso, 2020.
FIGUEREDO, Fernando Gomes; CRUZ, Ítalo Silva; PITA, Pablo. Avaliação do perfil de resistência bacteriana em uroculturas no cariri cearense–brasil. Avaliação do perfil de resistência bacteriana em uroculturas no cariri cearense–brasil, p. 1-388–416. Comunicação científica e técnica em medicina [recurso eletrônico] /Organizador Benedito Rodrigues da Silva Neto. – Ponta Grossa, PR: Atena, 2020
FRANÇA, Fabrício Rota et al. Incidência de infecção relacionada à assistência à saúde na unidade de terapia intensiva de um hospital de médio porte. Revista funec científica-multidisciplinar-ISSN 2318-5287, v. 9, n. 11, p. 1-12, 2020.
GOLDMAN, L., SCHAFER, A. I. Cecil: Medicina 24ª edição. Rio de Janeiro: Elsevier, 2014
GUPTA, Kalpana et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clinical infectious diseases, v. 52, n. 5, p. e103-e120, 2011.
HADDAD JM, FERNANDES DA. Infecção do trato urinário. São Paulo: Federação Brasileira das Associações de Ginecologia e Obstetrícia (Febrasgo); 2018. (Protocolo Febrasgo – Ginecologia, nº 63/Comissão Nacional Especializada em Uroginecologia e Cirurgia Vaginal).
IRONMONGER D, EDEGHERE O, GOSSAIN S, HAWKEY PM. Use of antimicrobial resistance information and prescribing guidance for management of urinary tract infections: survey of general practitioners in the West Midlands. BMC Infect Dis. 2016 May 24;16:226. doi: 10.1186/s12879-016-1559-2. PMID: 27221321; PMCID: PMC4877747.
JORGE, H. M. S.; VIDAL, E. C. F. Infecção do trato urinário hospitalar e suas implicações para a gestão do cuidar: revisão integrativa. Cadernos de Cultura e Ciência, Crato, v. 13, n. 1, p.39-48, 2014.
JÚNIOR, A. N., FILHO, M. Z., REIS, R. B. Urologia Fundamental. Sociedade Brasileira de Urologia (SBU) São Paulo: Planmark, 2010
KANG CI, KIM J, PARK DW, et al. Clinical Practice Guidelines for the Antibiotic Treatment of Community-Acquired Urinary Tract Infections. Infect Chemother. 2018;50(1):67–100. doi:10.3947/ic.2018.50.1.67
KIM, Woong Bin et al. Recent antimicrobial susceptibilities for uropathogenic Escherichia coli in patients with community acquired urinary tract infections: a multicenter study. Urogenital Tract Infection, v. 12, n. 1, p. 28-34, 2017.
LEE, Dong Sup et al. Role of age and sex in determining antibiotic resistance in febrile urinary tract infections, International Journal of Infectious Diseases, Volume 51, 2016, Pages 89-96, ISSN 1201-9712, https://doi.org/10.1016/j.ijid.2016.08.015.
MACHADO, Ariane Dhoyce; NAUMANN, Daniele Cristina; FERRAZZA, Magda Helena Soratto Heitich; TENFEN Adrielli; GUEVOHLANIAN-SILVA, Bárbara Yasmin; WEBER, Karla. Prevalência de infecção urinária em um laboratório de análises clínicas da cidade de Jaraguá do Sul, SC, no ano de 2017. RBAC, v. 51, n. 3, p. 213-8, 2019.
MARKS, Fernanda Ossani et al. Infecção do trato urinário: etiologia, perfil de sensibilidade e resistência aos antimicrobianos em hospital pediátrico. Research, Society and Development, v. 9, n. 8, 2020.
MARTINS, Milton de Arruda; CARRILHO, Flair José; ALVES, Venâncio Avancini Ferreira; CASTILHO, Euclides Ayres de; CERRI, Giovanni Guido. Clínica Médica: Doenças hematológicas, oncologia, doenças renais. 2ª edição. Barueri-SP. Editora Manole [S.l: s.n.], 2016.
MILO G, KATCHMAN EA, PAUL M, CHRISTIAENS T, BAERHEIM A, LEIBOVICI L. Duration of antibacterial treatment for uncomplicated urinary tract infection in women. Cochrane Database Syst Rev. 2005;(2):CD004682. Published 2005 Apr 18.
NABER KG, SCHITO G, BOTTO H, PALOU J, MAZZEI T. Surveillance study in Europe and Brazil on clinical aspects and Antimicrobial Resistance Epidemiology in Females with Cystitis (ARESC): implications for empiric therapy. Eur Urol. 2008;54(5):1164–75
NÓBREGA, M M. Bacteriúria em mulheres após estudo urodinâmico: fatores de risco e análise microbiológica. São Paulo, 2015. Dissertação de Mestrado. Faculdade de Ciências Médicas da Santa Casa de São Paulo – Curso de Pós-Graduação em Pesquisa em Cirurgia.
NY, Sofia et al. Antimicrobial resistance of Escherichia coli isolates from outpatient urinary tract infections in women in six European countries including Russia. Journal of global antimicrobial resistance, v. 17, p. 25-34, 2019. ISSN 2213-7165.
OLIVEIRA, Sergio Marcelino; SANTOS, Ludimylla Lins Gondim. Infecção do trato urinário: estudo epidemiológico em prontuários laboratoriais. Journal Health NPEPS. 2018; 3(1):198-210.
OLIVEIRA, M. K. R.; ALENCAR, S. S.; DIAS, C. A. G. M.; FECURY, A. A. Perfil epidemiológico da mortalidade dos setores intensivos de um hospital público de Macapá/AP. Temas em Saúde, v. 20, p. 163-177, 2020. https://temasemsaude.com/wp-content/uploads/2020/04/20209.pdf
RESENDE, J. A. et al. Infecção do trato urinário de origem hospitalar e comunitária: revisão dos principais micro-organismos causadores e perfil de susceptibilidade. Revista Científica Fagoc Saúde. Vol 1. 2016. ISSN: 2448-282X
RODRIGUES, S. C. S.; FECURY, A. A.; DIAS, C. A. G. M.; OLIVEIRA, E. Occurrence of Staphylococcus Aureus in Hospitals: A literature review. Revista Científica Multidisciplinar Núcleo do Conhecimento, v. 02, p. 33-42, 2016. https://www.nucleodoconhecimento.com.br/health/staphylococcus-aureus
SANTOS, Amanda Grossi et al. Prevalência de positividade bacteriana em exames de urina de um laboratório particular em itapevi. 2017. Revista Saúde em Foco – Edição nº 9 – Ano: 2017.
SANTOS, Maria José Amador dos; PORCY, Claude; DE OLIVEIRA MENEZES, Rubens Alex. Etiologia e perfil de resistência bacteriana em uroculturas de pacientes atendidos em um hospital público de Macapá-Amapá, Brasil. Um estudo transversal. REVISTA DIAGNÓSTICO E TRATAMENTO• VOLUME 24• EDIÇÃO 4, p. 135, 2019
TIAGO, Keyla Pereira et al. Frequência e resistência de uroculturas provenientes de pacientes internados na unidade de terapia intensiva do hospital municipal de Santarém-PA. RBAC, v. 52, n. 1, p. 64-70, 2020.
TOOKE, C. L., HINCHLIFFE, P., BRAGGINTON, E. et al. β-Lactamases and β-Lactamase Inhibitors in the 21st Century. Journal of molecular biology, 431(18), 3472–3500. https://doi.org/10.1016/j.jmb.2019.04.002
WIJTING, I. E. A. et al. Urinary tract infections in a university hospital: pathogens and antibiotic susceptibility. The Netherlands Journal of Medicine, v. 77, n. 6, p. 210-219, 2019.
ZAVALA-CERNA, Maria G. et al. The Clinical Significance of High Antimicrobial Resistance in Community-Acquired Urinary Tract Infections. Canadian Journal of Infectious Diseases and Medical Microbiology, v. 2020, 2020.
[1] Academic of the 11th period of the medical course at the Federal University of Amapá (UNIFAP).
[2] Academic of the 11th period of the medical course at the Federal University of Amapá (UNIFAP).
[3] Academic of the 11th period of the medical course at the Federal University of Amapá (UNIFAP).
[4] Biologist Master in Forest Sciences from the Federal University of Rio Grande do Norte (UFRN). PhD student at the Federal University of Viçosa (UFV).
[5] Biologist, PhD in Theory and Behavior Research, Professor and researcher of the Chemistry Degree Course of the Institute of Basic, Technical and Technological Education of Amapá (IFAP) and the Graduate Program in Professional and Technological Education (PROFEPT IFAP).
[6] Theologian, PhD in Psychoanalysis, researcher at the Center for Research and Advanced Studies – CEPA.
[7] Biologist, PhD in Topical Diseases, Professor and researcher of the Physical Education Course, Federal University of Pará (UFPA).
[8] Biomedical, PhD in Topical Diseases, Professor and researcher of the Medical Course of Macapá Campus, Federal University of Amapá (UNIFAP).
Posted: February 2021
Approved: February 2021