ORIGINAL ARTICLE
OLIVEIRA, Arthur Aires de [1], MOREIRA, Danilo José Silva [2], PIMENTEL, Jhon Allyson Sena [3], COSTA, Pedro Henrique de Magalhães [4], DIAS, Claudio Alberto Gellis de Mattos [5], ARAÚJO, Maria Helena Mendonça de [6], OLIVEIRA, Euzébio de [7], DENDASCK, Carla Viana [8], SOUZA, Keulle Oliveira da [9], FECURY, Amanda Alves [10]
OLIVEIRA, Arthur Aires de. Et al. Analysis of the Main Preexisting Risk Factors In Patients Diagnosed With COVID-19 In Amapá, Amazônia, Brazil. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year 06, Ed. 06, Vol. 17, pp. 56-72. June 2021. ISSN: 2448-0959, Access link: https://www.nucleodoconhecimento.com.br/health/preexisting-risk, DOI: 10.32749/nucleodoconhecimento.com.br/health/preexisting-risk
SUMMARY
COVID-19 (Coronavirus Disease 2019) is an infection caused by the SARS-CoV-2 virus, with first cases reported in December 2019 in Wuhan City. It was found that in patients with comorbidities, there is a higher risk of complications and mortality in case of infection. The disease was considered by the World Health Organization in 2020 as a public health emergency and, in Brazil, the Ministry of Health implemented measures for epidemiological monitoring of cases registered in the different federative units of the country. Among these, Amapá assumes high levels of incidence and mortality. This study aims to analyze the main previous risk factors found in patients with COVID-19 in the State of Amapá. For this, secondary data available in the Coronavirus Amapá Panel were used through a search conducted on May 22, 2020. On the platform, data were collected on the number of patients diagnosed with COVID-19, as well as the number of deaths due to the disease, with joint evaluation in each topic of comorbidities found. After grouping this data into Microsoft Excel spreadsheets, a quantitative and descriptive analysis of these was performed. In the State, a total of 28,927 patients diagnosed with COVID-19 were registered until the day of collection. About 1.31% (378 cases) of these had a risk factor that could susceptible them to develop complications resulting from COVID-19, with diabetes and chronic heart disease being the conditions with the highest number of records. Still in the State of Amapá, 420 deaths in patients with COVID-19 were found. Of this total, 75.71% (318 cases) had previous risk factors for higher risk of complications due to COVID-19, with hypertension and diabetes being the predominant conditions. With the study, it was noticed in Amapá that a large part of the population of patients diagnosed with the disease and who died had a history of risk factor for COVID-19. Due to the notification of risk factors in the death situation that were not recorded in the number of diagnosed patients, as well as the nonspecificity inherent to the condition of patients monitored by the state’s health mechanisms, it was not possible to perform a more detailed analysis about the degree of complication and lethality rate generated by a given risk factor and its association with coronavirus infection.
Keywords: COVID-19, Risk factors, Comorbidity.
INTRODUCTION
In the first half of December 2019, the first case of pneumonia of unknown origin had been reported in Wuhan, Hubei Province, China. Subsequently, an outbreak of severe acute respiratory syndrome pneumonia (SRAG) plagued the province, drawing the attention of the World Health Organization (WHO), which, starting from the circumscription of its attributions, declared that the situation was an epidemic caused by a new subtype of virus belonging to the coronaviridae family, coronavirus-2, constituting a Public Health Emergency of International Importance (ESPII), on January 30, 2020 (COSTA et al., 2020a; FERRARI, 2020; GAUTRET et al., 2020; GUAN et al., 2020; LI et al., 2020; LIMA et al., 2020; MARTINS-CHAVES; GOMES; GOMEZ, 2020; OLIVEIRA et al., 2020; RENU; PRASANNA; GOPALAKRISHNAN, 2020; RODRÍGUEZ-COLA et al., 2020; TAY et al., 2020; ZHAI et al., 2020).
In February 2020, the WHO Director General named the disease coronavirus-19 disease (COVID-19), an infection caused by SARS-CoV-2 (of the expression Severe Acute Respiratory Syndrome Coronavirus 2), one of the seven known coronavirus subtypes (COSTA et al., 2020a; RENU; PRASANNA; GOPALAKRISHNAN, 2020; HONG et al., 2020).
From the Brazilian perspective, COVID-19 infection was declared by the Ministry of Health (MS) as a Public Health Emergency of National Importance (ESPIN) on February 3, 2020, and had its first case confirmed in Brazil on February 26 (OLIVEIRA et al., 2020; OLIVEIRA; LUCAS; IQUIAPAZA, 2020). As a measure of support to the Health System, the Department of Informatics of the Unified Health System (DATASUS), through the Contingency Plan, acted providing virtual assistance to the population through the application “Coronavírus SUS” (BRASIL, 2020a).
In Brazil, the progress of the pandemic is mainly monitored by the MS through statistical indices that reflect the status of each federative unit (UF), and the State of Amapá assumes high epidemiological indices, especially regarding the incidence coefficient of COVID-19 (BRASIL, 2020c).
Until July 17, 2020, Amapá led the Brazilian North in the ranking of the COVID-19 Incidence Coefficient per notification UF (number of confirmed cases per 100,000 inhabitants), whose value was 3,637.4 followed by Roraima, with 3,327.1, which in turn was subsequenced by the State of Amazonas, with 1962.0. As for the COVID-19 Mortality Coefficient (number of deaths per 100,000 inhabitants), Amapá was in 7th place (55.2) (BRASIL, 2020c).
Risk factors relate to any conditions that impair the body’s immune response to an illness. Thus, these factors include both comorbidities, that is, chronic diseases previously installed and that act concomitantly in the patient’s organism, as well as particularities of individuals, namely: puerperal condition, smoking, alcohol consumption, among others (PIRES; OAK; XAVIER, 2020; ENGIN; ENGIN; ENGIN, 2020; KHALIQ; PHOSWA, 2020).
Studies suggest that patients infected with COVID-19 who have comorbidities have higher immunological vulnerability as well as a higher lethality rate when compared to patients affected only by the virus. The main comorbidities listed include hypertension, diabetes, heart disease and chronic diseases of the respiratory system (COSTA et al., 2020a; FERRARI, 2020; MARTINS-CHAVES; GOMES; GOMEZ, 2020; RENU; PRASANNA; GOPALAKRISHNAN, 2020; YANG et al., 2020).
Given the global panorama and in view of the status of the State of Amapá, it is essential to carry out analyses, studies and promotions in scientific research, in order to establish appropriate managements for patients affected by underlying diseases and/or conditions that represent potential risk factors to the prognosis of patients diagnosed with SARS-CoV-2, aiming to mitigate the complications presented by them (RENU; PRASANNA; GOPALAKRISHNAN, 2020; YANG et al., 2020).
GOALS
To analyze the distribution of the main preexisting risk factors in patients diagnosed with COVID-19 in the State of Amapá, Amazônia, Brazil.
METHODOLOGY
This study aimed to make a quantitative and descriptive analysis of the number of patients affected by COVID-19 in Amapá who attest to risk factors for the disease, and for this, a consultation was made on May 22, 2020 at the Coronavirus Amapá Panel (painel.corona.ap.gov.br).
On the main page of the Coronavirus Amapá Panel, it was clicked on “download CSV” to obtain the main data of covid-19 cases in the State of Amapá. Then, in the “Comorbidities of confirmed patients” of the same page, the option “Inspect” in the upper right corner was selected to generate a list of comorbidities and their numerical relationship. The same process was repeated in the “Comorbidities of Dying Patients”. Subsequently, for each of the lists obtained, the “Fromatted CSV” option was selected in the “Download CSV” field to obtain the files and use them in Microsoft Excel.
Within these files, some comorbidities and risk situations were joined in the same set in order to standardize the results. To be: they are grouped -in Chronic Heart Diseases- chronic heart disease, chronic heart disease, chronic heart disease, chronic heart disease, cardiovascular disease, heart disease, cardiopathic disease, chronic heart disease, heart disease; are also in – Chronic Respiratory Diseases – chronic respiratory diseases, chronic respiratory disease, chronic respiratory diseases, chronic decompensated chronic respiratory disease; They are still in – Hypertension- hypertension, HAS, hypertensive; again are in – Heart Disease and Hypertension- Chronic heart disease (HAS), chronic heart disease – HAS, cardiovascular disease including hypertension, chronic heart disease HAS, heart disease (HAS), chronic heart disease – HAS; as well as in – Immunosuppression- immunosuppression, chromosomal disease carrier or RF state; Again are in – Heart Disease and Diabetes – chronic heart disease and diabetes, heart and diabetic; Thus they are in high risk pregnancy – high-risk pregnant woman, high-risk pregnant woman; Finally are in – Advanced Stage Chronic Kidney Diseases – Advanced Stage Chronic Kidney Disease, Advanced-Stage Chronic Kidney Disease, Advanced-Stage Chronic Kidney Disease.
In the spreadsheet “Comorbidities of Patients in Death”, the number of cases registered as “No information” were disregarded due to the inconclusiveness of this cutoff. The other data were selected and grouped as described above.
The present study used secondary data available in the public access domain and took into account ethical aspects based on Resolution 466/12.
RESULTS
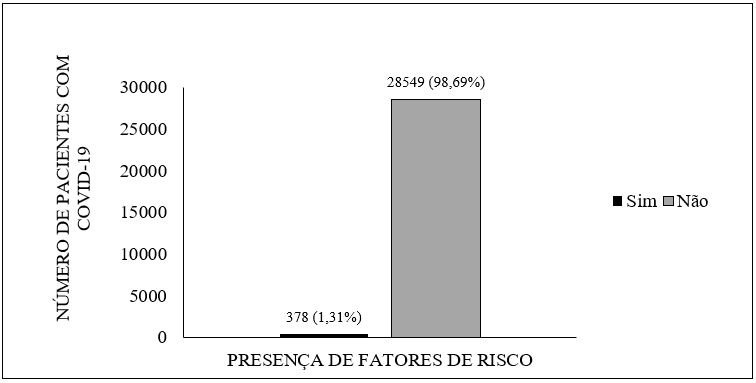
Among the 28,927 confirmed cases of COVID-19 in Amapá that were reported until the day of collection, approximately 1.31% of patients (378 cases) had a risk factor that could susceptible them to develop complications due to involvement by SARS-CoV-2, as shown in Figure 1.
Figure 1 Presence of risk factors in patients diagnosed with COVID-19 in Amapá until May 22, 2020.
As for patients who had risk factors, 5.02% of them (19 cases) had more than one. Associations include heart disease and hypertension (3.44%), heart disease and diabetes (1.06%), angioplasty and coronary atheromatosis (0.26%) and chronic kidney disease and diabetes (0.26%).
Regarding the main risk factors reported alone by affected patients, it was found that the majority had diabetes 29.89% (112 cases), followed by chronic heart diseases with 28.84% (109 cases).
It is noticed that diseases of the cardiological sphere are present in a majority way, considering that 173 patients in total are affected by diseases of this class, adding individuals with multiple risk factors and individuals only with heart disease.
Table 1 – Distribution of risk factors in patients diagnosed with COVID-19 in Amapá.
| Risk factors | Number of reports | Percentage(%) |
| diabetes | 113 | 29,89% |
| Chronic Heart Disease | 109 | 28,84% |
| Chronic Respiratory Diseases | 71 | 18,78% |
| hypertension | 46 | 12,17% |
| Heart Disease and Hypertension | 13 | 3,44% |
| immunosuppression | 11 | 2,91% |
| Heart Disease and Diabetes | 4 | 1,06% |
| High Risk Pregnancy | 4 | 1,06% |
| Advanced Stage Chronic Chronic Disease | 3 | 0,79% |
| Angioplasty and Coronary Atheromatosis | 1 | 0,26% |
| Chronic Heart Disease and Diabetes | 1 | 0,26% |
| Liver Cirrhosis | 1 | 0,26% |
| depression | 1 | 0,26% |
| Total | 378 | 100,00% |
Source: Coronavirus Amapá Panel.
In total, 420 deaths were recorded at the time of the study. Of this quantitative, it was found that 318 patients had a history of comorbidity or predisposing condition to complications.
Figure 2 – Presence of risk factors in patients who died with COVID-19 in Amapá until May 22, 2020.
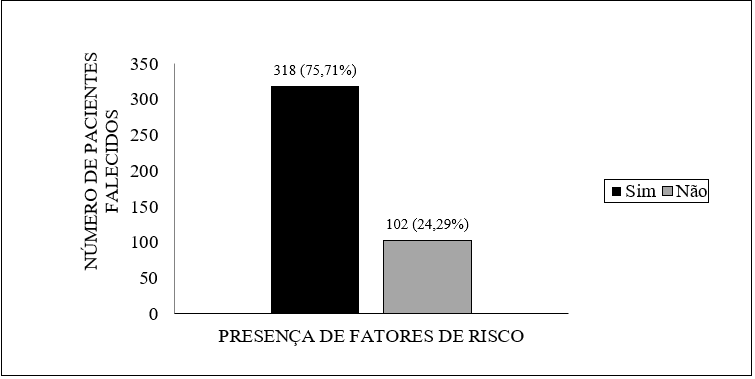
Regarding the risk factors present in patients who died, the main record was hypertension, present in 38.68% of patients (123 cases). It was also noted the presence of other aggravating factors that were not previously described in individuals with confirmed infection. They are obesity, cerebrovascular disease, neoplasia, smoking, Alzheimer’s, pancreas disease, dengue, alcohol consumption and puerperal period.
Table 2 – Distribution of risk factors recorded in patients who died with COVID-19 in Amapá.
| Comorbidity | Number of deaths | Percentage (%) |
| hypertension | 123 | 38,68% |
| diabetes | 93 | 29,25% |
| Diseases Of The Skin | 27 | 8,49% |
| Heart | 19 | 5,97% |
| obesity | 19 | 5,97% |
| Respiratory Diseases | 15 | 4,72% |
| Cerebrovascular Diseases | 8 | 2,52% |
| Immunosuppressive Diseases | 3 | 0,94% |
| Neoplasms | 3 | 0,94% |
| smoking | 2 | 0,63% |
| Alzheimer ‘s | 1 | 0,31% |
| Pancreas Disease | 1 | 0,31% |
| Liver Disease | 1 | 0,31% |
| dengue fever | 1 | 0,31% |
| Etilist | 1 | 0,31% |
| Puerpera | 1 | 0,31% |
| Total | 318 | 100,00% |
Fonte: Painel Coronavírus Amapá.
DISCUSSION
The states of the Amazon region of Brazil have considerable socioeconomic discrepancies when compared to the others, a situation that may reflect the greatest impact on the health system observed. In the State of Amapá, after the first case was reported on March 25, 2020, COVID-19 spread massively, as well as in the other federative units (DIAS et al., 2020; MENDONÇA et al., 2020).
The number of patients with COVID-19 who have risk factors for the disease in Amapá, compared to the total number of infected patients, is considered low. There is consensus in the literature that comorbidities and situations of immunological vulnerability are considered aggravating factors for the COVID-19 condition, and this fact may have prompted individuals in the risk groups to redouble their care (COSTA et al., 2020b; RODRÍGUEZ-COLA et al., 2020).
In a study conducted by Wang et al. (2020), it was reported that of 36 patients who required care in the Intensive Care Unit UTI), 26 (72.2%) had comorbidities, a finding that indicates that a history of chronic diseases can lead to the development of complications. Silva et al. (2020), in a clinical and epidemiological characterization study with 1560 patients diagnosed with COVID-19 from the city of Macapá-AP, found that 102 patients (6.54%) comorbidities.
The main comorbidities recorded alone in the patients in the present study were diabetes, chronic heart diseases, chronic respiratory diseases and hypertension. A meta-analysis made with a total of 1576 participants by Yang et al. (2020) also highlights hypertension (21.1%), diabetes (9.7%), cardiovascular diseases (8.4%) and diseases of the respiratory system (1.5%) as the most frequent comorbidities. Silva et al. (2020) found that of the 102 patients with comorbidities diagnosed with COVID-19 evaluated, chronic cardiovascular diseases (38.33%), diabetes (24.16%) and chronic respiratory diseases (13.33%) were the most prevalent risk factors. These conditions are associated with a high risk of serious manifestations of COVID-19 (GOMES; GOMEZ, 2020; MARTINS-CHAVES), which is explained in parts by the increased expression of angiotensin-converter enzyme 2 (ECA2) in alveolar, cardiac, β pancreatic and vascular endothelium epithelial cells. ECA2 allows the entry of the virus into the cells of the body, a fact that corroborates the failure of the corresponding organs during the infectious condition (ANGHEBEM; REGO; TARTH, 2020; ASKIN; TANRIVERDI; ASKIN, 2020).
Some patients also had other comorbidities and risk factors, including immunosuppression, high-risk pregnancy, chronic kidney diseases, angioplasty with coronary atheromatosis, liver cirrhosis, and depression.
Data from the present study show a lethality for patients with immunosuppressive diseases of 27.27%. It is believed that the more compromised the immunity of patients with COVID-19, the worse the prognosis of the disease, a reason that frames immunosuppressed patients as groups at risk for the disease (GOMES; GOMEZ, 2020; MARTINS-CHAVES). However, there is a report in the literature that most of the immunosuppressed patients evaluated followed with a good prognosis. A study conducted by Hrusak et al. (2020) with pediatric patients undergoing anticancer treatment showed that of 9 children diagnosed with COVID-19, 8 followed with mild symptoms or were even asymptomatic. Besides, Bussalino et al. (2020) state that the maintenance of immunosuppression may make the course of COVID-19 mild for the patient by reducing the storm of cytokines characteristic of the disease.
Regarding pregnancy, 4 cases of high-risk pregnancy were reported in the State. Maternal risks are suspected because systemic and local immunological changes are triggered in the mother’s body, ranging from a pro-inflammatory state to an anti-inflammatory state (LIU et al., 2020). In the case of pregnant women with COVID-19, a meta-analysis made by Trippela et al. (2020) with 275 pregnant women affected by the disease showed that 269 described their symptomatology, and 91.82% had symptoms, including fever and cough as the most common, and 8.18% were asymptomatic. Most patients present mild or asymptomatic symptoms, with few reports on the development of complications (CAPARROS-GONZALEZ, 2020; TRIPPELA et al., 2020).
In relation to chronic coronary diseases, only 3 confirmed cases were reported to the epidemiological surveillance system of Amapá coronavirus. However, 27 cases of deaths of patients who previously had comorbidities of this class of diseases were inserted into the system, suggesting a possible underreporting of comorbidities. In a prospective cohort study produced by Cheng et al. (2020) with 701 individuals affected by COVID-19, it was noticed that 26.7% of the people analyzed had hematuria and 43.9% proteinuria. These clinical findings suggest the presence of laboratory problems (MOITINHO et al., 2020). Given that SARS-CoV-2 acts directly on the ECA2 receiver (ASKIN; TANRIVERDI; ASKIN, 2020) and which has already been evidenced an overexpression of this enzyme in the proximal tubular cells of patients with chronic oral diseases (ANA et al., 2020), it is believed that the history of life diseases may aggravate the picture of COVID-19 (RENU; PRASANNA; GOPALAKRISHNAN, 2020). In addition, it has been associated with the preexistence of renal diseases with the impairment of the functionality of the patient’s immune system, a process that could be explained by the inflammatory process established during nephropathy. This fosters the idea that these diseases are risk factors for COVID-19 (OYELADE; ALQAHTANI; CANCIANI, 2020).
Regarding the relationship between angioplasty and coronary atheromatosis with COVID-19, no reports were found in the literature that could support the association between these risk factors and virus infection.
Of the reported cases of liver diseases in the State of Amapá, only 1 case of liver cirrhosis has been reported. It was also recorded the death of a patient who had previous liver disease, but it is not possible to affirm that it is the same patient since the preexisting disease was not specified. The literature shows that SARS-CoV-2 infection also involves the liver (AGHAGOLI et al., 2020), and the presence of liver diseases is considered a determining factor for the severity of the COVID-19 picture (RENU; PRASANNA; GOPALAKRISHNAN, 2020). A meta-analysis by Oyelade, Alqahtani and Canciani (2020) involving 5,595 patients showed a prevalence of liver diseases in a patient with COVID-19 of 3%, and of these, severity was reported in 57.33%. The same study revealed a mortality rate of 17.65%. Despite the severity, there was no correlation in the literature between pre-existing liver disease and the result of COVID-19.
In the only case of depression registered in the State, there is a concern of the scientific community about the possibility of neuropsychic diseases also constituting a risk to the COVID-19 condition. Mental health disorders, as well as the state of psychological distress, directly influence the functioning of an individual’s immune system, which may susceptible them to viral infections of the respiratory tract, which evidences a possible relationship between the patient’s emotional state and the degree of involvement by SARS-CoV-2 (RAJKUMAR, 2020). However, the effects generated by the virus on the patients in question, as well as the immunological response generated by the organism, are not well elucidated in the literature (TROYER; KOHN; HONG, 2020). For patients with a history of mental health weakness, greater attention should be paid to the condition, since it may relapse or worsen amid the installed pandemic scenario and a possible diagnosis of COVID-19 (YAO; CHEN; XU, 2020).
Data collected from the Amapá coronavirus panel indicate that 76% of the patients who died had comorbidities or pre-existing aggravating factors. An epidemiological survey by Almeida et al. (2020) in the State of Maranhão found that of the 100 patients diagnosed with COVID-19 and who died, 78% had previous comorbidities, assuming a pattern similar to what was observed in Amapá.
It is observed that hypertension is the most recorded risk factor among amapaense patients who died. However, it is not possible to determine the lethality rate for hypertensive patients, since the number of confirmed cases of the disease is lower than that reported of death. Nevertheless, the literature shows that this disease is one of the main aggravating factors for the COVID-19 condition, together with other cardiovascular diseases (AGHAGOLI et al., 2020; ALMEIDA et al., 2020; FERRARI, 2020). The pathophysiological mechanism proposed to explain this relationship involves the reinthine system. Due to the higher binding of SARS-CoV-2 to ECA2, the concentration of this enzyme is reduced in the host, resulting in high levels of angiotensin II and decreased angiotensin 1-7, effects that generate vasoconstriction and sodium retention and worsen the hypertensive condition (TADIC et al., 2020).
Regarding the relationship between diabetes and COVID-19, it is possible to worsen the patient’s clinical conditions, considering that SARS-COV-2 promotes increased blood glucose in patients with type 2 diabetes (BORNSTEIN et al., 2020). Worsening in the condition of diabetics may be related to the fact that this comorbidity decreases the body’s natural immunity (COSTA et al., 2020b; MA; HOLT, 2020). In relation to the reported cases of this disease in Amapá, it is noticeable that the number of confirmed patients (112) is quantitatively close to those who died (93), thus corroborating the idea that diabetes can aggravate the covid-19 condition to the point that the patient dies (COSTA et al., 2020b; RONCON et al., 2020).
Another important characteristic of the diabetes and SARS-COV-2 relationship is the mechanisms of complications resulting from the union of these two factors, since individuals who have diabetes and are infected by a virus are more at risk of developing complications (LACOBELLIS, 2020). A hypothesis about diabetes acting negatively, together with the virus, is related to ECA2, since it is present in several tissues and acts as a gateway to infectious agents on the cell surface (AGHAGOLI et al., 2020; MA; HOLT, 2020). In addition, patients who use Angiotensin-Suppressing Enzyme Inhibitors (IECAs) are more likely to develop complications due to higher ACE2 production, which favors the action of SARS-CoV-2 (FANG; KARAKIULAKIS; ROTH, 2020; FERRARI, 2020; MA; HOLT, 2020).
Heart diseases, in turn, are conditions associated with worse prognoses and high lethality rates (AGHAGOLI et al, 2020). A meta-analysis by Huang, Wang and Li (2020) found that of the 41 patients with COVID-19 evaluated, 6 (15%) had diseases of the cardiac sphere. In fact, there is a considerable number of patients with heart diseases who died in Amapá (19), generating a lethality rate of 15.07%. The literature associates this severity with the presence of ECA2 receptors in the heart, which are highly expressed in the organ, which can lead to the development of acute myocardial injury and chronic cardiovascular damage (AGHAGOLI et al, 2020). In addition, the advanced age and immunosenescence effect observed in most patients with heart disease may be associated with the prognosis of the COVID-19 condition (DRIGGIN et al., 2020).
A considerable number of patients with respiratory diseases were also observed, which corresponds to a lethality rate of 21.12% taking into account the number of patients diagnosed with COVID-19 who reported pre-existing comorbidities. The pre-existence of respiratory diseases is associated with severe conditions of COVID-19 (MARTINS-CHAVE; GOMES, GOHETS GOMEZ, 2020; YANG et al., 2020). It is known that the immune system responds to Infection by SARS-CoV-2 with an inflammatory process marked by the action of immune cells, tissue necrosis and local hyperplasia, effects that can impair the process of gas exchange of the lungs and generate a picture of severe pneumonia (GIMENEZ et al., 2020), which may justify why respiratory diseases are a risk factor for COVID-19.
Also in the information provided by the Coronavirus Amapá Panel, it is observed that some risk factors for COVID-19 found in patients who died were not reported from the session of risk factors of patients diagnosed with the disease, such as obesity, cerebrovascular diseases, neoplasms, smoking, Alzheimer’s disease, pancreatic disease, dengue, alcohol ism and puerperal period. This prevents a reliable analysis of the epidemiological scenario of the locality. However, some aspects about these conditions have been discussed in the literature.
About obesity, it has long been known that it is directly associated with poor prognoses and time-consuming recovery in cases of viral infections. This finding is attributed to the constant inflammatory state characteristic of obese individuals, supported by high levels of inflammatory drugs, which contributes to the impairment of the immunological response generated by these patients and, consequently, to the decrease in the ability to fight infectious agents (COSTA et al., 2020b; HUSSAIN et al., 2020; KORAKAS et al., 2020). In the context of COVID-19, other factors associated with obesity may be responsible for the higher chances of worsening the clinical picture, which includes deficient respiratory mechanics, low rate of gas exchange in the lungs, increased airway resistance, reduced lung strength and lower lung volume (STEFAN et al., 2020). A meta-analysis conducted by Hussain et al. (2020) showed that of the 2,451 patients with Body Mass Index (BMI) greater than 25 kg/m2 analyzed, 531 died, corresponding to a lethality rate of 21.66%. The same study also evaluated patients with BMI less than 25kg/m2,which totaled 24,506. Of these, 1701 died, a lethality rate of 6.94%. The comparison between these values demonstrates that overweight and obesity can influence the prognosis of the patient.
Cerebrovascular diseases have been reported in more severe cases of COVID-19 (WANG et al., 2020). The mechanism behind the increase in severity for this class of patients is still uncertain, although it is already suggested that it is similar to that of cardiovascular diseases (PRANATA et al., 2020).
Regarding the relationship between neoplasms and COVID-19, it is believed that cancer patients are susceptible to the development of complications due to the weakening of their immunological activity (ASOKAN; RABADIA; YANG, 2020; AL-QUTEIMAT; AMER, 2020). In fact, a retrospective study by Zhang et al. (2020) showed that, of 28 cancer patients evaluated, 8 died (mortality rate of 28.6%), indicating a poor prognosis for patients with pre-existence of neoplasms.
The history of smoking in turn is speculated as an important risk factor for the development of severe conditions of the disease, since smoking is associated with impaired lung health (VARDAVAS; NIKITARA, 2020). Although only one case of smoking has been reported in patients who died in our epidemiological analysis, there are studies that demonstrate an increased risk of severity in patients with a history of smoking. Alqahtani et al. (2020), in a meta-analysis involving 139 current smokers and 28 former smokers diagnosed with COVID-19, found that 31 current smokers (22.30%) and 13 former smokers (46%) worsened of their clinical conditions. In the same study, 5 current smokers of the 13 who developed complications died (mortality rate of 38.5%). These observations only reinforce that individuals who have already smoked or smoked should avoid the practice in the midst of the pandemic and always adopt preventive measures.
On Alzheimer’s disease, the association between advanced age and dementia, remarkable characteristics of the disease, as well as the possible impairment of neurocognitive development of these individuals during social isolation in the pandemic, encourage the scientific community to evaluate the pre-existence of Alzheimer’s as a risk factor for COVID-19 (BRASIL, 2020b; FERINI-STRAMBI; SALSONE, 2020). In the case of mortality, Bianchetti et al. (2020) found that of 82 patients diagnosed with COVID-19 and with dementia, 51 (62.2%) died, a rate higher than that of 26.2% observed in patients who did not have dementia, which points out that not only Alzheimer’s disease but also other dementias may be associated with a severe covid-19 condition.
The reported case of an etilist patient who died suggests habit as a possible risk factor for the disease. This association is supported by the previous knowledge that alcohol abuse can compromise liver function (EHRMANN; URBAN; DVORAN, 2019), which would scare the patient to develop complications and, consequently, a more severe picture of COVID-19.
The relationship between puerperium and COVID-19 is not as well established when compared to pregnancy (AN et al., 2020). Meanwhile, Tutiya et al. (2020) reported two cases of pulmonary microthrombi formation in puerperal women diagnosed with COVID-19. Besides, An et al. (2020) reported two cases of puerperal women who presented respiratory distress and worsening of the condition after delivery. These observations reinforce the need to monitor the condition of patients after delivery until there is stabilization.
Dengue and pancreatic diseases that have been reported in deaths due to COVID-19 in Amapá, however, no reports have been found in the literature on the association of these diseases and the development of complications of viral infection, although diseases that compromise the patient’s immunity tend to increase the chances of worsening pre-existing conditions (MARTINS-CHAVES; GOMES; GOMEZ, 2020).
CONCLUSION
The pre-existence of comorbidities or other conditions that impair the body’s immune response is a potential aggravating factor of the infectious condition generated by the new coronavirus, which may lead the patient to death. In the State of Amapá, a large part of the population of patients diagnosed with the disease and who died had a history of risk factor for COVID-19.
The main comorbidities reported in patients diagnosed with the disease were diabetes, chronic heart disease, chronic respiratory diseases and hypertension. The comorbidity with the highest record in cases of death was hypertension.
The notification of risk factors in the death chart that were not recorded in the picture of diagnosed patients, as well as the nonspecificity inherent to the condition of patients monitored by the health mechanisms of the State made a more detailed analysis about the degree of complication and lethality rate generated by a given comorbidity when it was associated with coronavirus infection.
For greater completeness and reliability of the results of a study like this, it is essential that sufficiently accurate and coherent data be obtained, so that the passage of patients through the health network can be analyzed and then included in scientific research, making it possible to understand and face the current pandemic and its repercussions in Amapá.
REFERENCES
AGHAGOLI, G. et al. Cardiac involvement in COVID‐19 patients: Risk factors, predictors, and complications: A review. J Card Sug., v. 35, p. 1302-1305, abr. 2020.
ALMEIDA, J. S. et al. Caracterização epidemiológica dos casos de covid-19 no maranhão: uma breve análise. Revista Prevenção de Infecção e Sáude, v. 6, mai. 2020.
AL-QUTEIMAT, O. M.; AMER, A. M. The Impact of the COVID-19 Pandemic on Cancer Patients. Am J Clin Oncol., abr. 2020. DOI: 10.1097/COC.0000000000000712.
ALQAHTANI, J. S. et al. Prevalence, Severity and Mortality associated with COPD and Smoking in patients with COVID-19: A Rapid Systematic Review and Meta-Analysis. PLoS One, v. 15, n. 5, e0233147, mai. 2020.
AN, P. et al. Postpartum exacerbation of antenatal COVID-19 pneumonia in 3 women. CMAJ, v. 192, n. 22, p. 603-606, jun. 2020.
ANGHEBEM, M. I.; REGO, F. G. M.; PICHETH, G. COVID-19 e Diabetes: a relação entre duas pandemias distintas. Revista Brasileira de Análises Clínicas. DOI: 10.21877/2448-3877.20200001. 2020.
ASKIN, L.; TANRIVERDI, O.; ASKIN, H. S. The Effect of Coronavirus Disease 2019 on Cardiovascular Diseases. Arq. Bras. Cardiol., São Paulo, v. 114, n. 5, p. 817-822, mai. 2020.
ASOKAN, I.; RABADIA, S. V.; YANG, E. H. The COVID-19 Pandemic and its Impact on the Cardio-Oncology Population. Curr Oncol Rep., v. 22, n. 6, mai. 2020.
BIANCHETTI, A. et al. Clinical presentation of COVID-19 in dementia patients. J Nutr Health Aging, mai., 2020. DOI: 10.1007/s12603-020-1389-1.
BORNSTEIN, S. R. et al. Practical recommendations for the management of diabetes in patients with COVID-19. The lancet Diabetes & endocrinology, v. 9, n. 6, p. 546-550, jun. 2020.
BRASIL. Plano de contingência DATASUS: Situação de crise provocada pelo novo coronavírus (covid-19). Versão 1.0, 2020a.
BRASIL. MINISTÉRIO DA SAÚDE. Alzheimer: o que é, causas, sintomas, tratamento, diagnóstico e prevenção. Disponível em:< https://saude.gov.br/saude-de-a-z/alzheimer>. Acesso em: 31 jul. 2020b.
BRASIL. MINISTÉRIO DA SAÚDE. Painel de casos de doença pelo coronavírus 2019 (COVID-19) no Brasil pelo Ministério da Saúde. Versão 2.0. Disponível em:< https://covid.saude.gov.br/>. Acesso em: 10 de jul. de 2020c.
BUSSALINO, E. et al. Immunosuppressive therapy maintenance in a kidney transplant recipient SARS-CoV-2 pneumonia: a case report. Am J Transplant., abr. 2020. DOI: 10.1111/ajt.15920.
CAPARRO-GONZALEZ, R. A. COVID-19 in PregnantWomen and Neonates: A Systematic Review of the Literature with Quality Assessment of the Studies. Rev Esp Salud Pública., v. 94, abr. 2020.
CHENG, Y et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Internacional, v. 97, n. 5, p. 829-838, mar. 2020.
CHINAZZI, M. et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science, v. 368, n. 6489, p. 395-400, mar. 2020.
COSTA, I. B. S. S. et al. O Coração e a COVID-19: O que o Cardiologista Precisa Saber. Arq. Bras. Cardiol., v. 114, n. 5, p. 805-816, mai. 2020a.
COSTA, F. F. et al. Metabolic syndrome and COVID-19: An update on the associated comorbidities and proposed therapies. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, v. 14, n. 5, p. 809-814, 2020b.
DIAS, N. L. et al. Predição da propagação do SARS-CoV-2 no Estado do Amapá, Amazônia, Brasil, por modelagem matemática. Revista Científica Multidisciplinar Núcleo do Conhecimento, vol. 06, ano 05, ed. 05, p 73-95, mai., 2020.
DRIGGIN, E. et al. Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the COVID-19 Pandemic. J Am Coll Cardiol., v. 75, n. 18, p. 2352–2371, mai. 2020.
ENGIN, A. B.; ENGIN, E. D.; ENGIN, A. Two important controversial risk factors in SARS-CoV-2 infection: obesity and smoking. Environmental Toxicology and Pharmacology, v. 78, mai. 2020. DOI: 10.1016/j.etap.2020.103411.
ENGSTROM, E. et al. Recomendações para a organização da Atenção Primária à Saúde no SUS no enfrentamento da Covid-19. Observatório Covid-19 Fiocruz, Nota técnica. p. 13, mai. 2020.
EHRMANN, J.; URBAN, O.; DVORAN, P. Alcohol-related liver diseases. Cent Eur J Public Health, v. 27, p. 10-14, dez. 2019.
FAN, C. et al. ACE2 Expression in Kidney and Testis May Cause Kidney and Testis Damage After 2019-nCoV Infection. MedRxiv, fev. 2020. DOI: 10.1101/2020.02.12.20022418.
FANG, L.; KARAKIULAKIS, G.; ROTH, M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?. The Lancet. Respiratory Medicine, v. 8, n. 4, mai. 2020.
FERINI-STRAMBI, L.; SALSONE, M. COVID-19 and neurological disorders: are neurodegenerative or neuroimmunological diseases more vulnerable?. J Neurol., jul. 2020. DOI: 10.1007/s00415-020-10070-8.
FERRARI, F. COVID-19: Dados Atualizados e sua Relação Com o Sistema Cardiovascular. Arq. Bras. Cardiol., v. 114, n. 5, p. 823-826, mai. 2020. DOI: 10.36660/abc.20200215.
GAUTRET, P. et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. International journal of antimicrobial agents, mar. 2020. DOI: 10.1016/j.ijantimicag.2020.105949.
GIMENEZ, V. M. M. et al. Lungs as target of COVID-19 infection: Protective common molecular mechanisms of vitamin D and melatonin as a new potential synergistic treatment. Life Sci., v. 354, ago. 2020. DOI: 10.1016/j.lfs.2020.117808.
GUAN, W. et al. Clinical characteristics of coronavirus disease 2019 in China. New England journal of medicine, v. 382, n. 18, p. 1708-1720, fev. 2020.
HONG, H. et al. Clinical characteristics of novel coronavirus disease 2019 (COVID-19) in newborns, infants and children. Pediatrics and Neonatology, v. 61, n. 2, p. 131-132, abr. 2020.
HRUSAK, O. et al. Flash survey on severe acute respiratory syndrome coronavirus-2 infections in paediatric patients on anticancer treatment. European Journal of Cancer, v. 132, p. 11-16, abr. 2020.
HUANG, C.; WANG, Y.; LI, X. Características clínicas de pacientes infectados com o novo coronavírus de 2019 em Wuhan, China. Lanceta, v. 395, p. 497–506, jan. 2020.
HUSSAIN, A. Obesity and mortality of COVID-19. Meta-analysis. Obes Res Clin Pract., jul. 2020. DOI: 10.1016/j.orcp.2020.07.002.
KHALIQ, O. P.; PHOSWA, W. N. Is Pregnancy a Risk Factor of COVID-19?. European Journal of Obstetrics & Gynecology and Reproductive Biology, 2020. DOI: 10.1016/j.ejogrb.2020.06.058.
IACOBELLIS, G. COVID-19 and diabetes: can DPP4 inhibition play a role?. Diabetes research and clinical practice, v. 162, abr. 2020. DOI: 10.1016/j.diabres.2020.108125.
LI, H. et al. Coronavirus disease 2019 (COVID-19): current status and future perspective. International journal of antimicrobial agents, v. 55, n. 5, mai. 2020.
LIU, H. et al. Why are pregnant women susceptible to COVID-19? An immunological Viewpoint. Journal of reproductive immunology, v. 139, jun. 2020.
LIMA, D. L. P. et al. COVID-19 no estado do Ceará, Brasil: comportamentos e crenças na chegada da pandemia. Ciênc. saúde coletiva, v. 25, n. 5, p. 1575-1586, mai. 2020.
LUCENA, T. M. C. et al. Mechanism of inflammatory response in associated comorbidities in COVID-19. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, mai. 2020. DOI: 10.1016/j.dsx.2020.05.025.
MA, R. C. W.; HOLT, R. I. G. COVID‐19 and diabetes. Diabetic Medicine, abr. 2020. DOI: 10.1111/dme.14300.
MARTINS-CHAVES, R. R.; GOMES, C. C.; GOMEZ, R. S. Immunocompromised patients and coronavirus disease 2019: a review and recommendations for dental health care. Braz. res oral., São Paulo, v. 34, e048, mai. 2020.
MENDONÇA, F. D. Região Norte do Brasil e a pandemia de COVID-19: análise socioeconômica e epidemiológica. Journal Health NPEPS, v. 5, n. 1, 2020.
MOITINHO, M. S. et al. Lesão renal aguda pelo vírus SARS-COV-2 em pacientes com COVID-19: revisão integrativa. Rev. Bras. Enferm., Brasília, v. 73, n. 2, jul. 2020.
OLIVEIRA, A. C.; LUCAS, T. C.; IQUIAPAZA, R. A. What has the COVID-19 pandemic taught us about adopting preventive measures?. Texto & Contexto Enfermagem, Florianópolis, v. 29, mai. 2020. DOI: 10.1590/1980-265x-tce-2020-0106.
OLIVEIRA, W. K. et al. Como o Brasil pode deter a COVID-19. Epidemiol. Serv. Saude, Brasília, v. 9, n. 2, p. 1-8, abr. 2020.
OMS. ORGANIZAÇÃO MUDIAL DA SAÚDE. Painel da Doença de Coronavírus da OMS (COVID-19). Disponível em:< https://covid19.who.int/>. Acesso em: 10 de jul. de 2020.
OYELADE, T.; ALQAHTANI, J.; CANCIANI, G. Prognosis of COVID-19 in Patients with Liver and Kidney Diseases: An Early Systematic Review and Meta-Analysis. Trop. Med. Infect. Dis., v. 5, n. 80, mai. 2020.
PRANATA, R. et al. Impact of cerebrovascular and cardiovascular diseases on mortality and severity of COVID-19–systematic review, meta-analysis, and meta-regression. J Stroke Cerebrovasc Dis., v. 29, n. 8,: mai. 2020.
PIRES, L. N.; CARVALHO, L.; XAVIER, L. L. COVID-19 e desigualdade: a distribuição dos fatores de risco no Brasil. Research Gate, abr. 2020. DOI: 10.13140/RG.2.2.27014.73282.
RAJKUMAR, R. P. Ayurveda and COVID-19: Where psychoneuroimmunology and the meaning response meet. Brain, behavior and immunity, v. 87, p. 8-9, jul. 2020.
RENU, K.; PRASANNA, P. L.; GOPALAKRISHNAN, A. V. Coronaviruses pathogenesis, comorbidities and multi-organ damage – A review. Life sci., v. 255, mai. 2020. DOI: 10.1016/j.lfs.2020.117839.
RODRÍGUEZ-COLA, M. et al. Clinical features of coronavirus disease 2019 (COVID-19) in a cohort of patients with disability due to spinal cord injury. Spinal Cord Series and Cases, v. 6, n. 39, mai. 2020.
RONCON, L. et al. Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome. Journal of Clinical Virology, v. 127, jun. 2020. DOI: 10.1016 / j.jcv.2020.104354.
RUBIO-PÉREZ, I. et al. COVID-19: Conceptos clave para el cirujano. Cirugía Española, v. 98, n. 6, p. 310-319, jun./jul. 2020.
SIA, S. F. et al. Pathogenesis and transmission of SARS-CoV-2 in golden hamsters. Nature, mai. 2020. DOI: 10.1038/s41586-020-2342-5.
SILVA, A.W.C. et al. Caracterização clínica e epidemiologia de 1560 casos de COVID-19 em Macapá/AP, extremo norte do Brasil. Research, Society and Development, v. 9, n.8, e150985499, jun. 2020.
STEFAN. N. et al. Obesity and impaired metabolic health in patients with COVID-19. Nat Rev Endocrinol., abr. 2020. DOI: 10.1038/s41574-020-0364-6.
TAY, M. Z. et al. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol, v. 20, p. 363-374, abr. 2020. DOI: 10.1038/s41577-020-0311-8.
TADIC, M. et al. COVID‐19 and arterial hypertension: Hypothesis or evidence? J Clin Hypertens (Greenwich), jul. 2020. DOI:10.1111/jch.13925.
TRIPPELA, G. et al. COVID-19 in PregnantWomen and Neonates: A Systematic Review of the Literature with Quality Assessment of the Studies. Pathogens, v. 9, n. 6, jun. 2020.
TROYER, E. A.; KOHN, J. N.; HONG, S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain, behavior and immunity¸ v. 87, p. 34-39, jul. 2020.
TUTIYA, C. T. et al. Possible formation of pulmonary microthrombi in the early puerperium of pregnant women critically ill with COVID-19: Two case reports.
Case Rep Womens Health, v. 27, e00237, jun. 2020.
VARDAVAS, C. I.; NIKITARA, K. COVID-19 and smoking: A systematic review of the evidence. Tob Induc Dis., v. 18, mar. 2020. DOI: 10.18332/tid/119324.
WANG, D. et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. Journal of American Medical Asssociation, v. 323, n. 11, p. 1061-1069, fev. 2020.
YANG, J. et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis., v. 94, p. 91-95, mai. 2020.
YAO, H.; CHEN, J. H.; XU, Y. F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry, v. 7, n. 4, mar. 2020.
ZHAI, P. et al. The epidemiology, diagnosis and treatment of COVID-19. International journal of antimicrobial agents, v. 55, n. 5, mai. 2020.
ZHANG, L. et al. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol., v. 31, n. 7, p 894-901, jul. 2020.
[1] Medical scholar. Federal University of Amapá (UNIFAP).
[2] Medical scholar. Federal University of Amapá (UNIFAP).
[3] Medical scholar. Federal University of Amapá (UNIFAP).
[4] Medical scholar. Federal University of Amapá (UNIFAP).
[5] Biologist, PhD in Theory and Behavior Research, Professor and researcher of the Chemistry Degree Course of the Institute of Basic, Technical and Technological Education of Amapá (IFAP) and the Graduate Program in Professional and Technological Education (PROFEPT IFAP).
[6] Doctor, Master in Teaching and Health Sciences, Professor and researcher of the Medical Course of Macapá Campus, Federal University of Amapá (UNIFAP).
[7] Biologist, PhD in Tropical Diseases, Professor and researcher of the Physical Education Course, Federal University of Pará (UFPA).
[8] Teóloga, Doctora en Psicoanálisis Clínica. Trabaja desde hace 15 años con Metodología Científica (Método de Investigación) en Orientación de Producción Científica para Estudiantes de Maestría y Doctorado. Especialista en Investigación de Mercados e Investigación en Salud, Estudiante de Doctorado en Comunicación y Semiótica (PUC SP).
[9] Social Scientist, Specialist in Management and Teaching of Higher Education, Master’s student in Anthropic Studies in the Amazon (UFPA).
[10] Biomedical, PhD in Tropical Diseases, Professor and researcher of the Medical Course of Macapá Campus, Federal University of Amapá (UNIFAP), Pro-Rector of Research and Graduate Studies (PROPESPG) of the Federal University of Amapá (UNIFAP).
Submitted: June, 2021.
Approved: June, 2021.















