REVIEW ARTICLE
SILVA, Natália Matos da [1]
SILVA, Natália Matos da. Consequences of the COVID-19 pandemic on mental health. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year. 07, Ed. 07, Vol. 01, p. 150-167. July 2022. ISSN: 2448-0959, Access link: https://www.nucleodoconhecimento.com.br/health/consequences-of-the-covid, DOI: 10.32749/nucleodoconhecimento.com.br/health/consequences-of-the-covid
ABSTRACT
With the rapid spread of COVID-19, several preventive measures have been taken around the world in order to control the advance of the new coronavirus. Among them, the social distancing caused by the COVID-19 pandemic stands out, which impacted the mental health of individuals due to the emergence of a state of panic worldwide and the triggering of feelings such as fear, insecurity and anguish. Therefore, this study sought to answer the following guiding question: what were the consequences of the COVID-19 pandemic on people’s mental health? Therefore, the main objective was to analyze the impacts caused on the mental health of society through the COVID-19 pandemic. Therefore, based on bibliographic and documentary research, it was possible to observe an increase in the symptoms of mood disorders, mainly depression and anxiety, in addition to acute, post-traumatic stress and panic episodes in the entire population. In this perspective, recent research has indicated the need to monitor the impacts of the pandemic on mental health, as well as implement programs for the prevention and control of crises and relevant situations of behavioral and mental disorders, in view of the time of social confinement, the pressures to sustain the economy, fear of contamination and the need to return to work.
Keywords: Mental Health, COVID-19, Stress, Prevention, Pandemic.
1. INTRODUCTION
On January 30, 2020, the outbreak of the new coronavirus – COVID-19 – was declared by the World Health Organization (WHO), recognized as a Public Health Emergency of international relevance with the highest alert level of the WHO, of accordance with the International Health Regulations.
In view of this, Brazil was in 2nd place in the ranking of countries with the highest number of cases of COVID-19, having recorded 7,753,752 confirmed cases and 196,561 deaths, according to data from the Interactive Panel of the Unified Health System (2020), on the 4th of January 2021.
Therefore, it is important to highlight the impact of the rapid advance of the disease in favoring behavioral changes capable of boosting psychological illness, generating serious consequences for the mental health of individuals. With this in mind, this study sought to answer the following guiding question: what were the consequences of the COVID-19 pandemic on people’s mental health? Therefore, the main objective is to analyze the impacts caused on the mental health of society through the COVID-19 pandemic. In addition, it had as specific objectives: to conceptualize mental health; and understand the impacts and consequences caused by COVID-19 on the mental health of individuals.
According to the WHO, mental health goes beyond the absence of mental disorders and refers to a state of complete physical, social and mental well-being that allows a person to cope with stress, apply their skills and have productivity at work and the ability to make contributions to the community in which it is inserted. In view of this, mental health is fundamental for the survival of the individual, whether collective or individual, as it makes it possible to interact with other people, reason and control emotions (OMS, 2016).
That said, this study aimed to produce informative material aimed at the mental health of the entire population, which, in turn, is experiencing a delicate moment in the face of this new coronavirus.
Discussing mental health during the pandemic is essential, since, among the preventive measures established by health agencies, social distancing and/or isolation has presented itself as a measure of greater impact, seen as a factor that has been leading individuals to the development of various disorders, such as anxiety, stress, panic, among others.
Analyzing the topic of mental health in the midst of a difficult time such as the pandemic is fundamental for students and professionals working in the area, as it provides a set of information regarding the impact generated by COVID-19 in Brazil, as well as generates the possibility of presenting techniques and strategies to manage and face the circumstances that impact mental health during the period of isolation established due to the global pandemic.
2. METHODOLOGY
The present work can be classified as an explanatory and applied research, since the explanatory research, according to Andrade (2002, p. 20), “aims to deepen the knowledge of reality, looking for the reason, the why of things and for this reason is more prone to errors”. Therefore, this research is classified as explanatory, because it evaluates the consequences of the COVID-19 pandemic on the mental health of individuals.
On the other hand, applied research generates knowledge in practical application and, according to Gil (2008, p. 47), “it is fundamentally motivated by the need to solve concrete problems, more immediate or not”. In this way, the present research is applied, as it verifies the main changes in the lives of individuals in the face of the need for social isolation due to the COVID-19 pandemic that devastated the world and brought several consequences for people and companies.
In this context, regarding the approach to the problem of this research, it is highlighted that it was based on qualitative, because, according to Richardson (1999), it describes the complexity of the problem in question, analyzes the interaction of variables, understands and classifies the dynamic processes experienced by social groups. Furthermore, it “contributes to the process of change in a given group and enables, at a greater level of depth, the understanding of the particularities of the behavior of individuals” (RICHARDSON, 1999, p. 80).
Therefore, regarding the technical procedures, this research was classified as documentary and bibliographical, because, according to Gil (2008, p. 73), it was “developed based on material already prepared, consisting mainly of books and scientific articles”. Therefore, being a research about the area of mental health and the economic area, the bibliographic research is widely used in the social sciences about the theories and practices described by the authors.
In this sense, it is observed that, although documentary and bibliographic research are similar, their difference lies in the nature of the sources, since documentary research uses materials that have not received an analytical treatment or that can still be reworked according to the research objects (GIL, 2008).
3. DEVELOPMENT
3.1 MENTAL HEALTH
The World Health Organization defines health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity”. Therefore, similarly, mental health encompasses much more than the absence of mental disorders. In fact, it is understood as the product of biological, psychological and social factors.
Estudiosos de diferentes culturas definem diversamente a saúde mental. Os conceitos de saúde mental abrangem, entre outras coisas, o bem-estar subjectivo, a auto-eficácia percebida, a autonomia, a competência, a dependência intergeracional e a auto-realização do potencial intelectual e emocional da pessoa. Numa perspectiva transcultural, é quase impossível definir saúde mental de uma forma completa. De um modo geral, porém, concorda-se quanto ao facto de que a saúde mental é algo mais do que a ausência de perturbações mentais (OMS, 2001, p. 31).
That said, in 1990, Brazil was a signatory to the Declaration of Caracas, which brought a new bias to psychiatric care. Therefore, among the guidelines, the Declaration preached integral, continuous and community-based care, with an adjustment to primary health care and that dispensed with the use of psychiatric hospitals, through normative acts. Therefore, the conditions for the development of the community network in mental health in Brazil were defined by the Federal Executive (PEREIRA, 2019).
The Psychosocial Care Centers (CAPS) were established with financial transfers from the government to the States and, especially, to the Municipalities, which had the direct management of the new provisions of the Brazilian Psychiatric Reform (RPB) (PEREIRA, 2019).
In 2001, after twelve years in the National Congress, Federal Law No. 10,216, known as the Paulo Delgado Law, was enacted, replacing the original Bill, bringing fundamental changes to the normative text, such as the provision on guarantees, rights and protection of individuals with mental disorders. However, the existence of psychiatric hospitals was not extinguished by the Law. In this way, the Law redirected mental health care, with a privilege to offer treatment in community-based services, and established on the protection and rights of individuals with mental disorders, despite not instituting clear mechanisms for the extinction progressive increase in asylums (PEREIRA, 2019).
Even so, when enacted, the Federal Law imposed a new impetus and rhythm to the Psychiatric Reform process in the country. In the context of the publication of the Law and the holding of the III National Conference on Mental Health, the Mental Health Policy of the Federal Government, in alignment with the guidelines of the Psychiatric Reform, was consolidated, receiving greater visibility and support (BRASIL, 2005).
Therefore, the Mental Health Policy originated from this Law, from which the safety of care for patients with mental disorders was proposed in services that replace psychiatric hospitals, leaving the old patterns of long-term hospitalization behind, where patients they stayed in isolated places without having contact with their families (BRASIL, 2012).
The Policy aims to structure a network of devices to allow, with the service, care for patients without mental suffering in their territory, the development of mechanisms to rehabilitate the subject in a psychosocial way and the deinstitutionalization of patients in long-term psychiatric hospitals permanence, through leisure, culture and work (BRASIL, 2012).
In view of this, it is relevant to inform about the centrality of the CAPS for the effective implementation of the Mental Health Policy, since such equipment is present in most cities in Brazil and is considered the gateway to the RAPS[2] for individuals with mental suffering ( PEREIRA, 2019).
Mental health is a very important area of public health, because it is responsible for monitoring the health-disease process, working mostly with complex biopsychosocial processes, which require an intersectoral and interdisciplinary approach, with actions that are inserted in the network of care and attention services and devices established in the territory, such as the Psychosocial Care Center (CAPS) (PEREIRA, 2019).
The biopsychosocial model was created and determined by Engels, in 1977, from the criticism regarding the deficiency in the traditional epidemiological system regarding the treatment of health as a phenomenon rooted in social organization (PUTTINI et al., 2010). In this context, the disease came to be seen not only as unicausal, as proposed by the biomedical model, but as a consequence of the relationship between tissue, interpersonal, cellular, environmental and organismal mechanisms and the criticism that the existing relationship between health-disease is considered a process (FAVA and SONINHO, 2008).
Soon, the definition of health, which was based on the absence of disease, began to be seen as a subjective well-being, from the point of view of the health-disease “paradigm”, not as a dichotomous definition, but as a process, characterizing another health care pattern, the biopsychosocial pattern (PEREIRA, 2019).
This new model brought a new way of seeing the disease by the health professional, implying the replacement of the word treat for care, since it encompasses the continuous renewal of the interpretation of respect for oneself, the world and the other, covering, in the same way, , meanings related to illness, autonomy, health and quality of life, aspects that transform into a space that is beyond scientific/technological know-how (MANDÚ, 2004).
That said, the concern about the mental health of society has increased during the difficult crisis experienced in the social sphere, as in the situation of the Covid-19 pandemic, which has come to qualify as one of the major public health problems in the world in recent decades (WHO, 2020). Therefore, it is essential to highlight that Brazilians can still suffer social and psychological impacts in different degrees of severity and intensity (FIOCRUZ, 2020).
3.2 IMPACTS OF COVID-19
According to Tseng (2020 apud SAVASSI, 2021, p. 3), the pandemic can be divided into four waves, the first being marked by the high rate of morbidity and mortality from COVID-19, the second by the impact of the reallocation of medical resources for complaints acute, the third for the impact of the interruption of care in chronic conditions and, finally, the fourth for the impacts on mental health, as shown in Figure 1.
Figure 1: Health Systems Overload Waves
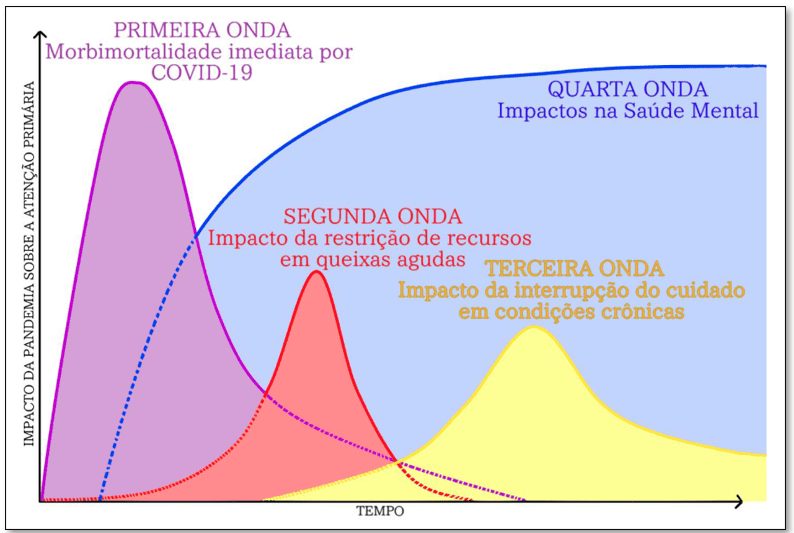
In view of this, it is possible to explain the so-called fourth wave and the impacts generated by the pandemic on the mental health of people with several factors, such as lack of economic security, social restrictions, the lack of certainty produced by a new circumstance and false and false information doubtful (SAÚDE DEBATE, 2020)
In pandemic scenarios, the number of individuals whose mental health is affected tends to be greater than the number of individuals who are infected properly. This is due to fear and uncertainties, including contamination, affecting infected people and those around them, and producing economic and psychosocial impacts that are impossible to calculate. (SAÚDE DEBATE, 2020).
Thus, despite noting that the search for psychological or psychiatric care has grown, there has been a trend in the increase of psychiatric diseases through the fourth wave of COVID-19. Examples of these diseases are mood and anxiety disorders (post-traumatic stress and panic are included), paranoid or psychotic symptoms and depression that can even lead a person to suicide (SAÚDE DEBATE, 2020).
Based on this, Shigemura et al. (2020) and Brooks et al. (2020) pointed out that patients who received the diagnosis of COVID-19 or who were suspected of having the disease experienced intense behavioral reactions and emotions, in addition to fear, anger, anxiety, guilt, insomnia, melancholy, loneliness, among other feelings. Thus, these states could progress to disorders such as depression, psychotic symptoms, Post Traumatic Stress Disorder (PTSD), suicide and panic attacks, being preponderant in patients in social isolation, where stress tends to prevail.
In view of this, it is noted that stress, anxiety and symptoms of depression in the face of the pandemic have been observed in the general population and even in health professionals (SCHMIDT et al., 2020). The Agência Brasil website pointed out that the anxiety index in Brazilians during the months of May, June and July 2020 reached 80%, from which the impact generated by the pandemic on people’s mental health can be considered as a health public crisis (GUIMARÃES, 2021).
In this context, in their study carried out in Canada after the COVID-19 outbreak, Ramírez-Ortiz
(2020) observed symptoms of stress in health professionals as an effect of the high risk of the service provided, the feeling of being very vulnerable to contamination by the virus, the high demand of patients depending on their care and depressed mood.
Given this, Weber et al. (2015) highlighted that stress has an impact on health, quality of life, social relationships and professional performance. And when the ability to work is reached, stress becomes a systemic issue in education and of social importance (SOUZA, NOVAES and ZIRPOLI, 2021).
Therefore, in another study, the same authors found that about 10% of healthcare professionals in China had PTSD symptoms as a result of their routine care for patients diagnosed with COVID-19; and when their friends and family were infected, the possibility of having PTSD symptoms was 2 to 3 times greater (RAMÍREZ-ORTIZ et al., 2020).
From this perspective, Stroebe, Schut and Stroebe (2007) state that the fact of not being able to be with family members and provide support, regardless of the severity of the health condition, can become a trigger for the appearance of symptoms of sadness and guilt.
Due to the fact that the transmission of the virus happens through personal contact, family members are commonly separated from their other relatives diagnosed with COVID-19, in order to avoid contagion, however, in situations of greater severity of the disease, when it happens death, it is observed that the person may have feelings of frustration and incapacity for not being present with their loved one (SUN, BAO and LU, 2020).
In this aspect, the pandemic ended up generating the aggravation of stressors, with the manifestation of frustration, distorted sleep, stress, discouragement and anxiety being notorious. These factors are framed in the main symptoms of mental illness, also called Common Mental Disorders (CMD) (TRINDADE, MORCERF and DE OLIVEIRA, 2018).
Therefore, according to Temsah et al. (2020) and Wang et al. (2020), from the point of view of mental health, an increase in symptoms of mood disorders was observed, mainly depression and anxiety, in addition to acute, post-traumatic stress and panic episodes in the entire population.
In this respect, stress, worry and fear are considered adaptive responses to real or perceived threats, although they are sometimes exaggerated in the context in which they occur (WHO, 2020a).
For example, stress by itself is not considered a disease. The problem with stress lies in its aggravation and persistence, as it can generate psychological and physical illnesses. Among the most common problems, it is possible to highlight respiratory problems, high blood pressure, panic attacks, gastritis, depression, skin diseases and increased anxiety. These pathologies end up waking up when there is a lot of stress (SALAS, 2020).
In addition, the fear of becoming infected, efforts to meet the demands generated by changes in routine in the social, work and family environments, end up accelerating the manifestation of changes in affection and mood in individuals, especially in those with a history of diseases or are part of risk groups (BARROS-DELBEN et al., 2020).
Furthermore, Silva et al. (2020) pointed out that, in the context of the pandemic, there was the emergence of fear, increased levels of stress and anxiety in healthy people and the intensification of symptoms related to pre-existing psychiatric disorders (GUIMARÃES, 2021).
During the pandemic, fear is capable of intensifying the levels of anxiety and stress in healthy individuals and raising the symptoms of those with pre-existing mental disorders (RAMÍREZ-ORTIZ et al., 2020).
Therefore, Pimentel and Silva (2020) state that it is essential to separate the psychological effects that were produced in the COVID-19 pandemic, from the dimensions related to human suffering, that is, to understand and contextualize, in addition to providing policies for the reducing vulnerability and identifying demands that are particular to each population.
In addition, attention should be paid to other risk factors, such as previous diagnosis of mental disorder, lack of social support, low self-esteem and low purchasing power. Therefore, these factors can generate a significant influence on the person’s level of vulnerability in the psychosocial field.
From this perspective, Wang et al. (2020) highlighted that 53.8% of the population of China suffered from the psychological impacts of the COVID-19 pandemic, with a classification of moderate to severe. In this context, it was observed that these people considered to be in a state of vulnerability were mainly those who were part of risk groups: diagnosed individuals, family members, health professionals and individuals diagnosed with mental disorders. In this way, all were referred to psychological support services offered by the Chinese government (SHIGEMURA et al., 2020).
Therefore, it is highlighted that relevant changes in mental health have an impact on the functioning of day-to-day tasks, usually related to lack of attention, lack of concentration, lack of motivation, anhedonia (loss of pleasure in things), small accidents, increase in errors, decrease in interest in interacting with other individuals and propensity to leave work (CRUZ et al., 2020).
That said, it is important to draw attention to the fact that mental health should not be taken care of only when problems get bigger than the person is capable of handling. It is necessary to take some precautions for its prevention (SALAS, 2020).
A world like this was not imagined in normal times, and living in the midst of what is unknown can bring feelings that cause anxiety, anguish, panic, among others. Depending on how this situation is experienced, individuals who already have symptoms related to depression or any other problem related to mental health may have a worsening in their condition. The United Nations published the “Policy Brief: Covid-19 and the need for action in mental health”, where it expressed concern about the impacts generated by the pandemic on the mental health of individuals, leading to apprehension regarding the effects produced by the virus in the health of family members and of the patients themselves (GUIMARÃES, 2021).
Faced with this and knowing the impacts generated by COVID-19 on mental health, the World Health Organization carried out the preparation of several messages of psychosocial support and the well-being of people, which were directed to various groups that make up society. It was recommended that the population look for information regarding COVID-19 in reliable sources, search for stories of individuals who managed to achieve recovery from the disease and maintain a healthy routine, practicing physical exercises and having a regulated diet (MS-ARGENTINA, 2020).
In view of this, a study was carried out by Johnson, Saletti-Cuesta and Tumas (2020) regarding the relevance of knowledge about the risks for the emergence of mental disorders, in addition to the availability of psychotherapeutic and dynamic intervention programs during the pandemic. The support offered by the Chinese country, initially, was intended to reduce the consequences of the disease on the mental health of the population and served as a model for the rest of the world (DONG and BOUEY, 2020).
Lee (2020), Liu et al. (2020), Schmidt et al. (2020) and The Lancet (2020) point out that recent research has indicated the need to monitor the impacts of the pandemic on mental health, as well as implement programs for the prevention and control of crises and relevant situations of behavioral and mental disorders, in view of the time of social confinement, the pressures to sustain the economy, the fear of contamination and the need to return to work.
Thus, in summary, it is essential to emphasize that when debating the COVID-19 pandemic and mental health, it is essential to consider the social context in which the individual is inserted and their mental health, taking into account the lack of adherence to measures to prevent the fight against COVID-19; the stereotype; the grieving process and the use of medicines whose effectiveness has not been scientifically proven, which can lead to several consequences on psychological and physical health (WHO et al., 2020).
4. CONCLUSION
This article was based on the following guiding question: what were the consequences of the COVID-19 pandemic on people’s mental health? In order to analyze the impacts caused on the mental health of society through the COVID-19 pandemic.
Thus, through this research, it was possible to verify that the changes caused by the pandemic caused some people to develop mental illnesses or that pre-existing illnesses were accentuated, mainly due to the stress and anxiety caused during social isolation.
The social isolation caused by the COVID-19 pandemic has impacted the mental health of individuals due to the emergence of a state of panic worldwide and the triggering of feelings such as fear, insecurity and anguish due to the feeling of isolation. That said, it is noteworthy that, even though isolation is a measure widely used in the context of public health in order to preserve the physical health of the person, it is essential to think about the well-being and mental health of individuals who have been subjected to this isolation phase.
The expansion of the pandemic has demonstrated an increase in the most common mental disorders, especially adaptive disorders, which comprise debilitating behavioral and emotional changes, in association with episodes of panic, anxiety, stressful events and depression (SCHWARTZ et al., 2020). The pandemic ended up generating the aggravation of stressors, with the manifestation of frustration, distorted sleep, stress, discouragement and anxiety being noted.
Therefore, the importance of mental health care is highlighted, since physical, cognitive and mental well-being are essential for a better quality of life for the population. To this end, it is mentioned the need to create programs for the prevention and control of crises and relevant frameworks of behavioral and mental disorders to support society.
REFERENCES
ARGENTINA. COVID-19 Recomendaciones para la asistencia y continuidad de la atención ambulatoria en salud mental durante la pandemia. Ministerio de Salud, 2020. Disponível em: http://www.msal.gob.ar/images/stories/bes/graficos/0000001885cnt-covid-19_recomendaciones-asistencia-atencion-ambulatoria-salud-mental.pdf Acesso em: 13 abr. 2022.
BARROS-DELBEN, P. et al. Saúde mental em situação de emergência: Covid-19. Debates em Psiquiatria, v. 1, n. 2, p. 18-28, 2020. Disponível em: https://d494f813-3c95-463a-898c-ea1519530871.filesusr.com/ugd/c37608_6bd285d2f02b40098a94c81c49d603b8.pdf. Acesso em: 13 abr. 2022.
BRASIL. Ministério da Saúde. Reforma psiquiátrica e política de saúde mental no Brasil: documento apresentado à Conferência Regional de Reforma dos Serviços de Saúde Mental: 15 anos depois de Caracas. Brasília: Ministério da Saúde, 2005.
BRASIL. Ministério da Saúde. Saúde Mental em dados – 12. Informativo eletrônico. Brasília: Ministério da Saúde, 2012.
BROOKS, S. K. et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet Infect Dis, v. 395, n. 10227, p. 912–920, 2020. Disponível em: https://doi.org/10.1016/S0140-6736(20)30460-8 Acesso em: 13 abr. 2022.
CRUZ, R. M. et al. Retorno ao trabalho? Indicadores de saúde mental em professores durante a pandemia da COVID-19. Polyphonía, v. 31, 2020. Disponível em: https://www.revistas.ufg.br/sv/article/view/66964/35826. Acesso em: 13 abr. 2022.
DONG, L.; BOUEY, J. Public Mental Health Crisis During COVID-19 Pandemic, China. Emerg. Infect. Dis. Preprints. v. 26, n. 7, p. 1616-1618, 2020. Disponível em: https://pubmed.ncbi.nlm.nih.gov/32202993/. Acesso em: 13 abr. 2022
FAVA, G.; SONINHO, N. O modelo biopsicossocial trinta anos depois. Psychotherapy and psychosomatics, v. 77, n. 1, p. 1-2, 2008. Disponível em: https://pubmed.ncbi.nlm.nih.gov/18087201/. Acesso em: 01 jul. 2022.
FIOCRUZ. Fundação Oswaldo Cruz. Cartilha Saúde Mental e Atenção Psicossocial: Recomendações Gerais. Rio de Janeiro: Fiocruz, 2020. Disponível em: https://portal.fiocruz.br/documento/cartilha-saude-mental-e-atencao-psicossocial-na-pandemia-covid-19. Acesso em: 13 abr. 2022.
GIL, A. C. Como elaborar projetos de pesquisa. 4. ed. São Paulo: Atlas, 2008.
GUIMARÃES, E. Como está a saúde mental dos professores na pandemia? LeiaJá, 15 de outubro de 2021. Disponível em: https://m.leiaja.com/carreiras/2021/10/15/como-esta-saude-mental-dos-professores-na-pandemia/. Acesso em: 13 abr. 2022.
JOHNSON, M. C.; SALETTI-CUESTA, L.; TUMAS, N. Emociones, preocupaciones y reflexiones frente a la pandemia del COVID-19 en Argentina. Ciência & Saúde Coletiva Preprints, v. 25, n. 6, 2020. Disponível em: http://www.cienciaesaudecoletiva.com.br/artigos/emociones-preocupaciones-y-reflexiones-frente-a-la-pandemia-del-covid19-en-argentina/17552 Acesso em: 13 abr. 2022.
LEE, S. A. Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death Studies, v. 44, n. 7, p. 393-401, 2020. Disponível em: https://pubmed.ncbi.nlm.nih.gov/32299304. Acesso em: 13 abr. 2022.
LIU, N. et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Research, v. 287, p. 112921, 2020. Disponível em: http://www.sciencedirect.com/science/article/pii/S016517812030545X. Acesso em 13 abr. 2022.
MANDÚ, E. N. T. Intersubjetividade na qualificação do cuidado em saúde. Revista Latino-Americana de Enfermagem, v. 12, n. 4, p. 665-675, 2004.
OMS. Saúde mental depende de bem-estar físico e social, diz OMS em dia mundial. Nações Unidas, 2016. Disponível em: https://nacoesunidas.org/saude-mental-depende-de-bem-estar-fisico-e-social-diz-oms-em-dia-mundial/. Acesso em: 13 abr. 2022.
PAINEL INTERATIVO DO SISTEMA ÚNICO DE SAÚDE. Covid-19 no Brasil. Secretarias Estaduais de Saúde. Brasil, 2020. Disponível em: https://infoms.saude.gov.br/extensions/covid-19_html/covid-19_html.html. Acesso em: 04 jul. 2022.
PEREIRA, M. L. Perfil dos usuários do serviço de saúde mental de um município de médio porte de Minas Gerais. Trabalho de Conclusão de Curso (Bacharelado em Serviço Social). Departamento de Economia Doméstica. Universidade Federal de Viçosa. Minas Gerais, 2019. 55f.
PIMENTEL, A. D. S. G.; SILVA, M. N. R. M. O. Psychic Health in times of Corona Virus. Research, Society and Development, v. 9, n. 7, p. 1–13, 2020. Disponível em: https://doi.org/10.33448/rsd-v9i7.3602. Acesso em: 13 abr. 2022.
RAMÍREZ-ORTIZ, J. et al. Consecuencias de la pandemia COVID-19 en la Salud Mental asociadas al aislamiento social. SciELO Preprints, p. 1–21, 2020. Disponível em: https://doi.org/10.1590/SCIELOPREPRINTS.303 Acesso em: 13 abr. 2022.
RICHARDSON, R. J. Pesquisa social: métodos e técnicas. 3. ed. São Paulo: Atlas, 1999.
SALAS, P. Ansiedade, medo e exaustão: como a quarentena está abalando a saúde mental dos educadores. Revista Nova Escola. 2020. Disponível em: https://novaescola.org.br/conteudo/19401/ansiedade-medo-e-exaustao-como-a-quarentena-esta-abalando-a-saude-mental-dos-educadores. Acesso em: 13 abr. 2022.
SAÚDE DEBATE. Impacto da pandemia: a quarta onda da Covid-19 e a saúde mental. Conselho Regional de Medicina do Estado do Paraná (CRM-PR), 2020. Disponível em: <https://www.crmpr.org.br/Impacto-da-pandemia-a-quarta-onda-da-Covid19-e-a-saude-mental-11-54965.shtml>. Acesso: 13 abr. 2022.
SAVASSI, L. C. M. Ensaio acerca das curvas de sobrecarga da COVID-19 sobre a atenção primária. Journal of Management & Primary Health Care, 2021. Disponível em: https://www.jmphc.com.br/jmphc/article/view/1006/933. Acesso em: 04 jul. 2022.
SCHMIDT, B. et al. Saúde mental e intervenções psicológicas diante da pandemia do novo coronavírus (COVID-19). Estudos de Psicologia (Campinas), v. 37, 2020. Disponível em: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0103-166X2020000100501&nrm=iso. Acesso em: 13 abr. 2022.
SCHWARTZ, J.; KING, C. C.; YEN, M. Y. Protecting Healthcare Workers During the Coronavirus Disease 2019 (COVID-19) Outbreak: Lessons From Taiwan’s Severe Acute Respiratory Syndrome Response. Clinical infectious diseases, v. 71, n. 15, p. 858-860, 2020. Disponível em: https://pubmed.ncbi.nlm.nih.gov/32166318. Acesso em: 13 abr. 2022.
SHIGEMURA, J. et al. Public responses to the novel 2019 coronavirus (2019‐nCoV) in Japan: Mental health consequences and target populations. Psychiatry and Clinical Neurosciences, v. 74, n. 4, p. 281–282, 2020. Disponível em: https://doi.org/10.1111/pcn.12988. Acesso em: 13 abr. 2022.
SILVA, A. F. da. et al. Saúde mental de docentes universitários em tempos de pandemia. Physis, Rio de Janeiro, v. 30, n. 2, p. 1-4, 2020. Disponível em: https://www.ims.uerj.br/wp-content/uploads/2020/05/physis30_2_a16.pdf. Acesso em: 13 abr. 2022.
SOUZA, M. E. I. B. de.; NOVAES, N. M. F.; ZIRPOLI, B. B. P. O impacto da pandemia por Covid-19 na saúde mental dos professores: revisão sistemática da literatura. Trabalho de Conclusão de Curso (Curso de Psicologia). Faculdade Pernambucana de Saúde, 2021. Disponível em: https://tcc.fps.edu.br/bitstream/fpsrepo/1158/1/O%20Impacto%20da%20Pandemia%20por%20Covid-19%20na%20Sa%C3%BAde%20Mental%20dos%20Professores_Revis%C3%A3o%20Sistem%C3%A1tica%20da%20Literatura.pdf. Acesso em: 13 abr. 2022.
STROEBE, M.; SCHUT, H.; STROEBE, W. Health outcomes of bereavement. Lancet, v. 370, n. 9603, p. 1960–1973, 2007. Disponível em: https://doi.org/10.1016/S0140-6736(07)61816-9. Acesso em: 13 abr. 2022
SUN, Y.; BAO, Y.; LU, L. Addressing mental health care for bereavements during COVID-19 pandemic. Psychiatry and Clinical Neurosciences Preprints, v. 74, ed. 7, p. 1–5, 2020. Disponível em: https://doi.org/10.1111/pcn.13008. Acesso em: 13 abr. 2022
TEMSAH, M. H. et al. The psychological impact of COVID-19 pandemic on health care workers in a MERS-CoV endemic country. Journal of Infection and Public Health, v. 13, n. 6, p. 877-882, 2020. Disponível em: http://www.sciencedirect.com/science/article/pii/S1876034120304871. Acesso em: 13 abr. 2022.
THE LANCET. COVID-19: protecting health-care workers. The Lancet, v. 395, n. 10228, p. 922, 2020. Disponível em: https://doi.org/10.1016/S0140-6736(20)30644-9. Acesso em: 13 abr. 2022.
TRINDADE, M. de A.; MORCERF, C. C. P.; DE OLIVEIRA, M. S. Saúde mental do professor: uma revisão de literatura com relato de experiência. Revista Interdisciplinar de Extensão, v. 2, n. 4, p. 18, 2018.
WANG, Y. et al. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychology, health & medicine, v. 26, n. 1, p. 1-10, 2020. Disponível em: https://pubmed.ncbi.nlm.nih.gov/32223317. Acesso em: 13 abr. 2022.
WANG, Y. et al. Psychological assistance during the coronavirus disease 2019 outbreak in China. J Health Psychol, v. 25, n. 6, p 733-737, 2020. Disponível em: https://doi.org/10.1177/1359105320919177. Acesso em: 13 abr. 2022
WEBER, L. N. D. et al. O Estresse No Trabalho Do Professor. Imagens da Educação, v. 5, n. 3, p. 40-52, 2015. Disponível em: https://periodicos.uem.br/ojs/index.php/ImagensEduc/article/view/25789. Acesso em: 01 jul. 2022.
WHO. World Health Organization. Mental health and psychosocial considerations during the COVID-19 outbreak. World Health Organization, 2020a. Disponível em: https://apps.who.int/iris/handle/10665/331490. Acesso em: 13 abr. 2022.
WHO. World Health Organization. Q&A on coronaviruses (COVID-19). World Health Organization, 2020. Disponível em: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/q-a-coronaviruse. Acesso em: 13 abr. 2022.
APPENDIX – FOOTNOTE
2. Psychosocial Care Network.
[1] Graduated from the Vale do Aço School of Medicine – UNIVAÇO, Ipatinga – Minas Gerais. Physician postgraduate in Psychiatry, by IPEMED, city of São Paulo/SP. ORCID: 0000-0001-7660-7077.
Sent: May, 2022.
Approved: July, 2022.















