CLINICAL CASE
SILVA, Agnaldo Plácido da [1], PLÁCIDO, Eloá Jessica Mendes dos Santos [2], MORAES, Walber [3]
SILVA, Agnaldo Plácido da. PLÁCIDO, Eloá Jessica Mendes dos Santos. MORAES, Walber Breno de Souza. Revista Científica Multidisciplinar Núcleo do Conhecimento. Condylar hypoplasia: Clinical case. Multidisciplinary Scientific Journal Núcleo do Conhecimento. Year 06, Ed. 02, Vol. 01, pp. 124-131. February 2021. ISSN: 2448-0959, Access link: https://www.nucleodoconhecimento.com.br/health/condylar-hypoplasia, DOI: 10.32749/nucleodoconhecimento.com.br/health/condylar-hypoplasia
ABSTRACT
The formation of the face and the stomatognathic system is complex in nature and involves the development of multiple tissue processes that must unite and fuse in an extremely orderly manner. Disorders in the growth of these tissue processes or in their fusions can result in facial changes. The temporomandibular joint is one of the most complex in the human body, with the condylar process responsible for the expression of mandibular growth. Condylar hypoplasia is characterized by a defective formation of the condylar process that can be congenital or acquired. In the case presented, the patient has facial asymmetry since the first year of life, only on the left side. Thus, professionals working in the region of the temporomandibular joint must have knowledge of the existence and clinical implications for an early diagnosis in order to avoid the development of facial asymmetries, restoring the patient’s function, aesthetics and psychological status.
Keywords: Temporomandibular Joint. Facial asymmetry. Condylar hypoplasia. Condylar Process.
INTRODUCTION
The temporomandibular joint is one of the most complex joints in the human body (SHIVHARE et al., 2013), it is defined as a synovial, bilateral, interdependent joint, with its own movements, however simultaneous. It is also the only one in the cephalic skeleton classified as triaxial, that is, it is capable of performing movements around three axes (LIMONGI; MANZI and LIMONGI, 2019). It consists of the condylar process and the articular eminence of the temporal bone. The TMJ appears for the first time in the 8th week of gestation, where it is possible to observe two areas widely separated from the mesenchymal blasts that appear close to the eventual location of the mandibular condyle and the glenoid fossa (HORN et al., 2016). Bone and cartilage are first seen in the mandibular condyle at approximately the 10th gestational week (PEDRA et al., 2003). At birth, the articular surfaces are covered by fibrous connective tissue, over time the tissue is slowly converted into fibrocartilage and, in the same period of time, the deepening of the articular fossa occurs (HORN et al., 2016) . The head of the mandible plays a very important role in the joint, as it is responsible for the expression of mandibular growth (VASCONCELOS et al., 2012).
During embryonic development, morphological and functional changes may occur, such as condylar hyperplasia and hypoplasia, defects associated with specific diseases or syndromes (dysostosis of the facial jaw or first branchial arch syndrome), ankylosis, bifid condyle, among others (LIMONGI; MANZI and LIMONGI , 2019).
Bearing in mind that the growth of the skull, maxilla and mandible are closely related, and if there is no compensation in the growth of one of these areas, there will be an asymmetric development in some part of the craniofacial skeleton that may have resulted in deviation of the chin and mandibular midline (PROFFIT and WHITE JR, 1990).
Condylar hypoplasia is defined in the literature by Neville (NEVILLE et al., 2009) as a defective growth of the mandibular condyle, which can be congenital or acquired. In the case of congenital condylar hypoplasia, it is associated with syndromes of the head and neck, including mandibulofacial dysostosis, oculo-auriculo-vertebral syndrome (Goldenhar syndrome) and hemifacial microsomy. In the most severe cases, agenesis of the entire condyle or branch (condylar aplasia) can be observed. In the case of acquired condylar hypoplasia, it occurs due to disorders of the growth center of the developing condyle. The most common cause is trauma in the condylar region during the first and second decade of life, other causes include infections, radiation therapy and rheumatoid or degenerative arthritis (NEVILLE et al., 2009).
Hypoplasia can develop after the loss of one or both of the condylar growth centers, occurs in the early stages of development and can be accompanied by ankylosis, resulting from hemorrhages and inflammation in the adjacent structures causing fibrosis in the joint capsule (IBIKUNLE et al ., 2016) (HORN et al., 2016). Its severity is related to the period of growth of the condyles, up to approximately 25 years old, since condylar growth is more active in the first years of life (MOZE; HOYTE and BISSOON, 2012), and any disturbance during this phase can accentuate condylar hypoplasia, which will result in facial, skeletal and dental deformation, which will lead to a shortening of the mandibular branch (JACOBSON and STARR, 2008) (HORN et al., 2016). An early diagnosis, even in childhood, provides the patient with the possibility of being treated with orthopedic therapy. In cases of late diagnosis in adult patients, treatment will involve orthognathic surgery to correct skeletal deformity (JACOBSON and STARR, 2008).
CLINICAL CASE
A 6-year-old female child arrived at the Buccomaxillofacial Surgery and Traumatology service at Hospital Nossa Senhora do Perpetuo Socorro, located in the City of Garanhuns, accompanied by her mother; she reported that her daughter had asymmetry of the face on the left side. In the patient’s anamnesis, her companion (mother) had stated that such asymmetry has existed since the first years of life, and with the passing of the years, it became more and more accentuated, being the subject of comments in the child’s social environment. The mother was also asked if the child, during the first months of life, had suffered any trauma or had pictures of purulent otitis, but the mother did not remember any of these facts having occurred.
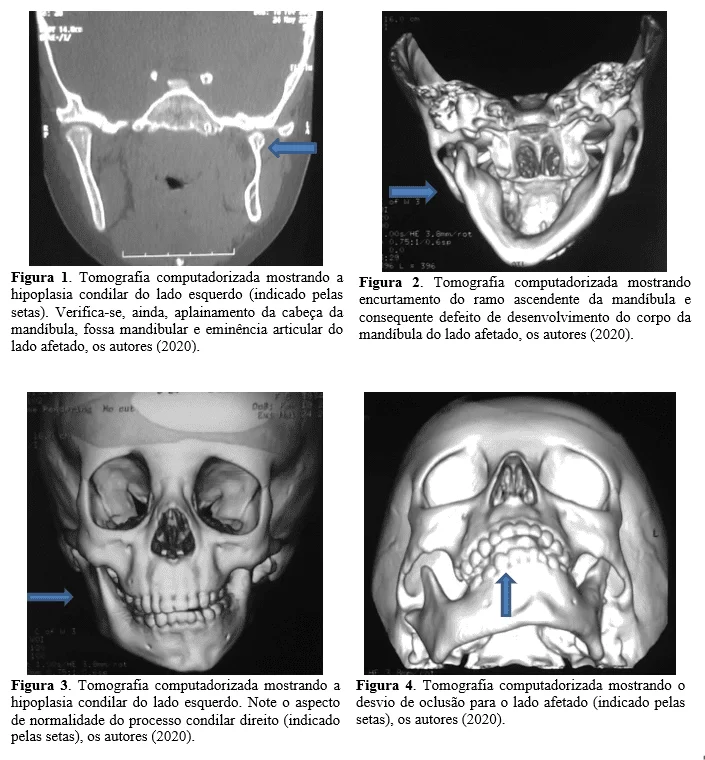
Initially, an extra oral examination was performed in which facial asymmetry was found, in addition to deflection in the mouth opening movement. In order to better assess the bony structures of the face and the TMJs, a computed tomography scan was requested. CT scan showed condylar hypoplasia on the left side, it was also possible to verify that the articular bone surfaces on this side (joint eminence, condylar process, and mandibular fossa) were flattened, in addition to shortening of the ascending branch of the mandible on the affected side and developmental defect of the body of the jaw. However, on the right side, all the articular bone components were within normality aspects. (Figure 1) –
RESULTS
As therapy, the patient was referred for follow-up and orthopedic treatment with an orthodontist, seeking to correct the occlusal plane and minimize facial asymmetry with a probable future need for orthognathic surgery, after the patient’s complete bone maturation.
DISCUSSION
Upon presentation of a patient with facial asymmetry, more specifically asymmetry of the mandibular zone, according to mentioned authors, condylar hypoplasia is described as having two possible origins and several diagnoses. For Miloro; Larsen and Waite (2008) one of the most common causes of facial asymmetry, in this case, mandibular, would be the trauma to the condyle; in many cases neither the child nor the parents have any memories of the traumatic event (MILORO; LARSEN and WAITE, 2008).
According to the literature, it is possible to be of acquired origin (by trauma during the growth of the condyle, by infections or degenerative arthritis) or of congenital origin (hemifacial microsomy or causes of genetic origin). In these cases, imaging tests are of great importance in establishing a diagnosis (conventional radiographs, panoramic radiography, computed tomography). These tests help to establish the anatomical degree of the deformation and the relationship between the deformation and the rest of the facial skeleton (MISHRA et al., 2013).
Condylar hypoplasia requires a multidisciplinary approach, “it is an ambiguous topic and with several possible causes, so that a correct and accurate diagnosis can be formed, the case must be well studied and evaluated every possible factor before starting a treatment for mandibular asymmetry. ”(FONSECA, 2015).
An important fact is that, according to the mother’s report, asymmetry has been present since the patient’s first year of life, that is, at birth she had no irregularities on her face, which leads us to believe that this condition was acquired over growth. In this case, the patient had started an orthopedic follow-up to minimize facial asymmetry. Early orthopedic therapy has been shown to be effective, since the problem is not only skeletal, but also muscular in that it presents elements of soft tissue with possible alteration (MOULIN-ROMSÉE et al., 2004). “With the stimulation of the functional apparatus, it is possible to obtain some soft tissue development and, in this way, improve facial development” (RIBEIRO et al., 2011).
Radiographic monitoring will be carried out in order to determine whether or not there is active growth of the mandibular condyle during orthopedic treatment. Condylar growth activity can be observed by comparing radiographs, either by cephalometric, panoramic or other imaging methods described in the literature, and with the emergence of new technologies for three-dimensional reconstruction of bone structures, these exams are becoming even more accurate and valuable (ROTH et al., 2010).
The evaluation of facial growth is of great importance in cases of skeletal, craniofacial or facial deformities, as well as in cases of asymmetry caused by hyper or condylar hypoplasia (BITTENCOURT et al., 2005) (CISNEROS and KABAN, 1984). Through this knowledge, it is possible to determine the ideal moment, the type and size of the surgery, that is, if the surgery should be performed at an early age or if bone growth should be completed, thus determining a less invasive form for the patients. more serious cases (BITTENCOURT et al., 2005).
CONCLUSION
Candillar hypoplasia can be seen as a pathological condition that represents a challenge for both orthodontists and oral and maxillofacial surgeons, due to its progressive and severe dentofacial deformity. Understanding the etiology, nature of the deformity, chronological and biological age are essential requirements to achieve better treatment results, early diagnosis is one of the fundamental prerequisites for restoring the patient’s function, aesthetics and psychological status.
REFERENCES
BITTENCOURT, L. P. et al. Skeletal scintigraphy for assessment of condylar uptake in class III malocclusion. Radiologia Brasileira, São Paulo, v. 38, n. 4, p. 273-277, July/Aug. 2005.
CISNEROS, G. J.; KABAN, L. B. Computerized Skeletal Scintigraphy for Assessment of Mandibular Asymmetry. Oral Maxillofac Surg, v. 42, n. 8, p. 513-520, Aug. 1984.
FONSECA, E. F. R. P. D. ASSIMETRIA MANDIBULAR: DIAGNÓSTICO PRECOCE EM ORTODONTIA. Universidade Fernando Pessoa. Porto, p. 47. 2015.
HORN, D. D. S. G. et al. Hipoplasia condilar de provável origem otológica. Revista CEFAC, v. 18, n. 3, p. 801-806, Maio-Junho 2016.
IBIKUNLE, A. A. et al. Management of a Rare Case of Mandibular Condylar Aplasia in a Resource‑limited Setting. Nigerian Journal of Experimental and Clinical Biosciences ¦, v. 4, n. 2, p. 48-52, July-December 2016.
JACOBSON, N.; STARR,. Implant-supported Rehabilitation of Severe Malocclusion Due to Unilateral Condylar Hypoplasia: Case Report. J Oral Implantol, v. 34, n. 2, p. 90-96, 2008.
LIMONGI, M. C.; MANZI, F. R.; LIMONGI, J. B. F. Temporomandibular joint alterations: two clinical case-reports of bifid condyle and temporomandibular joint ankylosis. Revista CEFAC, v. 21, n. 2, p. 1-7, 2019.
MILORO, M.; LARSEN, P. E.; WAITE, P. D. Pricipios de Cirurgias Bucomaxilofacial. São Paulo: Santos, v. II, 2008.
MISHRA, L. et al. Hemifacial Microsomia: A Series of Three Case Reports. Journal of Clinical and Diagnostic Research, v. 7, n. 10, p. 2383–2386, Oct. 2013.
MOULIN-ROMSÉE, C. et al. Treatment of Hemifacial Microsomia in a Growing Child: The Importance of Co-Operation between the Orthodontist and the Maxillofacial Surgeon. Journal of Orthodontics, v. 31, n. 3, p. 190-200, Sep. 2004.
MOZE, K.; HOYTE, T.; BISSOON, A. K. Cone Beam Computed Tomography in the Diagnosis of Unilateral Condylar Hypoplasia: Report of a Case. West Indian Med J, v. 61, n. 7, p. 739-742, Oct. 2012.
NEVILLE, B. W. et al. Patologia Oral e Maxilofacial. 3ª. ed. Rio de Janeiro: Elsevier, 2009. 17 p.
PEDRA E CAL NETO, J. O. A. et al. CRESCIMENTO E DESENVOLVIMENTO DA MAXILA. Revista Hospital Universitário Pedro Ernesto, UERJ, v. 33, n. 3, p. 25-29, JANEIRO / JUNHO 2003.
PROFFIT, W. R.; WHITE JR, R. P. Who Needs Surgical-Orthodontic Treatment? Int J Adult Orthodon Orthognath Surg, v. 5, n. 2, p. 81-89, 1990.
RIBEIRO, F. A. V. et al. Tratamento não-cirúrgico de microssomia hemifacial por meio da ortopedia funcional dos maxilares. RGO – Rev Gaúcha Odontol., Porto Alegre, v. 59, n. 1, p. 131-134, Jan./Mar. 2011.
ROTH, L. S. et al. Hiperplasia condilar: considerações sobre o tratamento e relato de caso. Revista de Cirurgia e Traumatologia Buco-maxilo-facial, Camaragibe, v. 10, n. 3, p. 19-24, Jul./Set. 2010.
SHIVHARE, P. et al. Condylar Aplasia and Hypoplasia: A Rare Case. Case Reports in Dentistry, p. 1-5, 2013.
VASCONCELOS, B. C. D. E. et al. Mandibular asymmetry: literature review and case report. Brazilian Journal of Otorhinolaryngology, v. 78, n. 4, p. 137, July/August 2012.
[1] PhD student in Biomedical Sciences at IUNIR- Italian University Institute of Rosario – Argentina. Specialist in Buccomaxillofacial Surgery and Traumatology – FACSETE – Faculdade de Sete Lagoas. Graduated in dentistry from ASCES – Associação Caruaruense de Ensino Superior. Graduated in Biologist at UPE – Universidade de Pernambuco.
[2] Graduated in Physiotherapy at UNINASSAU.
[3] Degree in Biology UPE- University of Pernambuco. Master in Natural Resources – UFCG. Professor at UNOPAR.
Submitted: July 2020.
Approved: January 2021.