REVIEW ARTICLE
SANTOS, Amadhonnis Pereira dos [1], SANTOS, Tiago França dos [2], FERREIRA, Jostein Henrique Cavalcanti [3], DIAS, Cláudio Alberto Gellis de Mattos [4], ARAÚJO, Maria Helena Mendonça de [5], DENDASCK, Carla Viana [6], OLIVEIRA, Euzébio de [7], FECURY, Amanda Alves [8]
SANTOS, Amadhonnis Pereira dos. et al. Celiac Disease: a review. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year 07, Issue 10, Volume 09, pp. 53-69. October 2022. ISSN: 2448-0959, Access Link: https://www.nucleodoconhecimento.com.br/health/celiac, DOI: 10.32749/nucleodoconhecimento.com.br/health/celiac
ABSTRACT
Celiac Disease (CD) is an immune-mediated enteropathy in response to the ingestion of gluten in genetically predisposed individuals, causing a malabsorptive syndrome. This review aims to conceptualize CD, describe its pathophysiology, highlight its epidemiology, detail associated clinical presentations, outline the diagnostic approach, and explain the treatment. To achieve this, works in English, Portuguese, and Spanish from the last five years were sought in the following databases: PubMed, LILACS, and SciELO, using the following keywords: “doença celíaca” and “celiac disease.” The search resulted in 175 articles, with 40 works chosen after screening and evaluation. The results revealed that CD affects approximately 1% of the global population, can be diagnosed at any age, but with more typical symptoms in children and atypical symptoms in adults. The pathogenesis involves the genetic factor HLA DQ2/DQ8, gluten ingestion, the formation of tissue transglutaminase antibodies, and an inflammatory reaction that damages the duodenum, impairing its absorptive function. Typical symptoms include chronic diarrhea, abdominal distension, weight loss, poor growth, and vitamin deficiencies. Atypical symptoms include dermatitis herpetiformis, refractory iron-deficiency anemia, delayed puberty, infertility, and neurological diseases. Diagnosis involves a suspected clinical picture, serologies for autoantibodies, genetic testing, and duodenal biopsy. Treatment is lifelong adherence to a gluten-free diet. Despite being well-characterized, CD remains underdiagnosed, and additional studies are needed.
Keywords: Celiac Disease, Malabsorptive Syndrome, Gluten.
INTRODUCTION
Celiac Disease (CD) is an immune-mediated condition triggered by gluten exposure (MAHADEV et al., 2018). Its discovery is attributed to the British pediatrician Samuel Gee in 1888 (BARROS, 2019). As Oliveira (2018) states, it is a chronic disease of the small intestine caused by gluten ingestion in genetically predisposed individuals. Gluten is a protein found in the following grains: wheat, rye, and barley (AL-ABACHI, 2022).
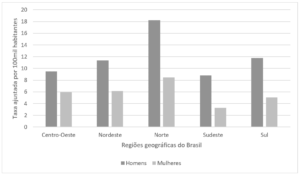
CD affects approximately 1% of the general population and is more common in men than in women (KOTZE, 2020). It can affect individuals of all age groups, and prevalence rates in Europe, around 1%, have also been similarly found in the Middle East, North Africa, and India (AL-ABACHI, 2022). According to Labrada et al. (2020), CD is considered the most common chronic inflammatory disease of the digestive tract. Oliveira (2022) reports that about 90% of cases go undiagnosed.
CD is characterized by diverse clinical presentations, including both intestinal and extraintestinal manifestations (OLIVEIRA, 2022). Gastrointestinal symptoms of the disease may include weight loss, constipation, diarrhea, and abdominal pain and distension, although many patients exhibit few or none of these symptoms (KOTZE, 2021). Iron-deficiency anemia and osteoporosis are possible clinical manifestations, particularly in adults (LASA, 2018). As Barros (2019) notes, CD can have the following clinical presentation forms: classic, non-classic, latent, and asymptomatic.
The definitive diagnosis of CD relies on a combination of clinical presentation, serological tests, and intestinal histology. Therefore, there is no gold standard for CD diagnosis, and a sequential approach with serological tests followed by duodenal biopsy is necessary (RAITERI et al., 2022). In Brazil, the Clinical Protocol and Therapeutic Guidelines for Celiac Disease, published by the Ministry of Health in 2015, outlines the diagnostic tests for the disease (CRUCINSCKI, 2021).
The only available treatment today is a lifelong gluten-free diet. Alternative research to develop a vaccine for CD was discontinued due to unsatisfactory results (KHAN et al., 2020).
OBJECTIVE
This work aims to appropriately conceptualize celiac disease, describing its pathophysiology, addressing its epidemiology, detailing the associated clinical presentations that are crucial for a proper diagnostic approach, and explaining the treatment for the disease and its complications.
METHOD
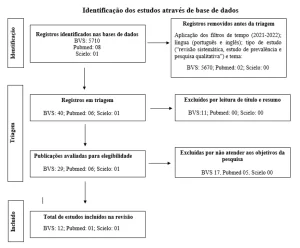
To conduct the review article, we sought to obtain references through searches in the following databases: PubMed, LILACS, and SciELO. The following keywords were used: “doença celíaca” and “celiac disease.”
To select the works, we employed the method of identifying the articles found in the search, conducting a screening, deciding on their eligibility, and including them in the study. In the database searches, we used the following filters: free full text, publications from the last 5 years, and review articles. Only works with content relevant to the subject, with accessible full text, and available in English, Portuguese, or Spanish were included.
The initial identification gathered all the works found in all the searched databases. Subsequently, we conducted screening by analyzing the title and abstract of the publications, assessing their relevance to Celiac Disease and determining which works were eligible. Finally, all works considered eligible were read in their entirety, and the exclusion of works that were not thematically relevant or lacked relevance to the review was performed. All studies approved in the selection stages were included in the results of this work.
RESULTS
Research in the databases on Celiac Disease with the applied filters yielded 175 articles in the work identification phase. After screening, 104 articles were excluded, leaving 71 works (40.57%) of eligible articles. Following the reading of the works, 31 eligible articles (43.66%) were excluded, concluding the selection with 40 included articles.
DISCUSSION
DEFINITION AND EPIDEMIOLOGY
Celiac Disease (CD) is also known as non-tropical sprue and gluten-sensitive enteropathy (LABRADA et al., 2020). CD is a multifactorial autoimmune disease resulting from the interaction of various genetic and environmental factors (AL-BLUWI et al., 2021). It is an autoimmune systemic disorder triggered by gluten consumption (KOTZE, 2018). It is a chronic condition in which the autoimmune reaction to gluten damages the duodenal mucosa, leading to inadequate nutrient absorption (GOBBO, 2018).
As stated by Balaban et al. (2019), CD was once considered the prototype of malabsorption in childhood, but the diagnosis in adults has shown a different phenotype. Classically, the disease develops during the first three years of life when gluten-containing cereals are introduced into the diet. However, a second peak of incidence is also observed in the third decade of life (FERREIRA, 2018). According to MOSCA et al. (2022), CD can occur at any age, with heterogeneous symptoms or conditions, and many patients go undiagnosed.
The average age for diagnosis is around 45 years in Europe in the last decade, but this does not mean that CD cannot be diagnosed in childhood and youth; it simply reflects that more diagnoses are occurring in this age group in recent years (MARTÍNEZ-RODRIGUEZ et al., 2020). Rato (2021) points out that the aging population, the increasing prevalence of CD, and the delay in its diagnosis explain the considerable increase in CD diagnoses in adulthood, especially in the elderly.
There has been a significant increase in CD prevalence worldwide in recent decades, primarily due to the greater availability of serological screening tests with improved sensitivity and specificity (AL-BLUWI et al., 2021). Several articles indicate a prevalence of 1% in the general population (SHAHRIARI et al., 2018; KOTZE, 2020). Martinello (2017) reports a prevalence of 1/214 in Brazil.
Patients with CD can develop up to 15% of other autoimmune diseases, and there is an increased prevalence of CD in individuals with different immune-mediated diseases (KOTZE, 2018). Autoimmune diseases such as diabetes mellitus (DM) and Hashimoto’s Thyroiditis are prevalent in CD patients (KHAN et al., 2020; BINICIER, 2020). PRIETO et al. (2021) mention the coexistence of DM and CD in about 5% of cases, with DM occurring a few years before the development of CD.
As Julian (2019) notes, there is an increased prevalence of CD among epilepsy patients, and an increased prevalence of epilepsy among those with CD. Khan et al. (2020) also state that since the 1960s, dermatitis herpetiformis has been established as the cutaneous manifestation of CD.
PATHOPHYSIOLOGY
In the pathogenesis of CD, there is a strong genetic component, as evidenced by its high familial recurrence and the high concordance of the disease among monozygotic twins, approximately 75% to 80% (RAITERI et al., 2022). CD is characterized by the expression of human leukocyte antigen (HLA) class II DQ2 or DQ8 molecules involved in the activation of T lymphocytes and the initiation of the autoimmune process. The T cell-mediated inflammatory process leads to the atrophy of the villi in the mucosa of the small intestine, causing malabsorption (MOSCA et al., 2022).
The presence of HLA DQ2/DQ8 is a pathogenic requirement for the development of the typical immune alterations found in CD (RAITERI et al., 2022). When studying HLA DQ2 (present in 90 to 95% of CD cases), Bajor et al. (2019) also mention that its genetic variations are related to the course of CD development and its complications. However, HLA DQ2/DQ8 can be found in up to 30%-40% of the general population; therefore, its specificity is notably low in ensuring a predisposition to CD (RAITERI et al., 2022). There are reports that the DQ7 haplotype may also represent a genetic predisposition to CD, but this confirmation still needs to be confirmed through further studies and in larger populations of celiac individuals (GOBBO, 2018).
In these genetically predisposed individuals, celiac disease is triggered by the ingestion of gluten and related prolamins in the diet (LAU, 2022). Thus, there is a combination of factors causing the disease: a strong genetic influence and exposure to dietary gluten (KOTZE, 2021).
CD is characterized by severe atrophy of the mucosa of the small intestine, leading to impaired digestion and malabsorption of nutrients, resulting in gastrointestinal disturbances and alterations in anthropometric parameters (LADINO et al., 2019). Through contact with the gliadin, an immune response to this fraction occurs, with the production of antibodies (BARROS, 2019).
This immune response is triggered by the ingestion of gluten, which is present in the endosperm of cereal seeds such as wheat, rye, and barley (SOLDERA, 2021; TEIXEIRA, 2017). Gluten is a compound of prolamins and glutelins, and the residues of glutamine are deaminated by the tissue transglutaminase enzyme, which can lead to inflammation of the intestinal mucosa, atrophy of the duodenal villi, causing malabsorption (EL-METWALLY et al., 2020).
Gluten is the primary protein complex in wheat and contains proteins that induce hypersensitivity reactions: gliadins (monomeric) and glutenins (protein aggregates), with equivalents in barley and rye. Gliadins and glutenins are storage proteins that impart viscoelastic physical characteristics to wheat flour (FERREIRA, 2018).
Prieto et al. (2021) point out that this malabsorptive syndrome triggered by gluten ingestion is primarily caused by tissue transglutaminase antibodies, which is an IgA-mediated response. Gluten proteins induce T-cell-associated inflammation in the small intestine and trigger an autoimmune response to their own proteins, such as tissue transglutaminase, leading to villous atrophy, crypt hypertrophy, and intraepithelial lymphocytosis (BINICIER, 2020).
A T-cell-mediated response to dietary gluten leads to the overproduction of inflammatory cytokines, contributing to mucosal damage in the intestine (GOBBO, 2018). Symptoms are related to the extent of mucosal involvement rather than the severity of pathology in the proximal small intestine mucosa. It is believed that the lesion pathology covers 30-50% of the entire small intestine mucosa, although this data still lacks further evidence from other studies (AKAY et al., 2020).
Gliadin binds to tissue transglutaminase enzyme in the intestinal lumen, forming a macromolecular complex that, in individuals predisposed to CD, is recognized as an antigen by antigen-presenting cells. In this activation process, macrophages release various pro-inflammatory cytokines that activate intraepithelial lymphocytes and result in the histological changes that define CD (GOBBO, 2018).
As an immune-mediated disease, CD has, in its pathophysiology, an inflammatory response based on the actions of helper T cells (Th1 and Th2) and pro-inflammatory cytokines such as interleukin-6 (IL-6) and tumor necrosis factor alpha (TNFα) (GOBBO, 2018).
According to Rouvroye et al. (2020), current evidence suggests that the neurological disorders associated with CD are also caused by this humoral immune response and cell-mediated response.
Wijarnpreecha et al. (2018) points out that smoking is a protective factor for the development of CD and speculates that this may be due to cigarette substances altering the ability of T cells to respond to gliadin and reducing intestinal permeability. However, the study itself acknowledges limitations that do not invalidate the theory but require further studies for confirmation.
When examining the association between CD and gastrointestinal tumors, Lasa (2018) provides support for an increased risk of colorectal adenomas but clarifies that more studies are needed to confirm the hypothesis. Zullo et al. (2017) report that CD patients have a higher risk of developing lymphoma and adenocarcinoma of the small intestine.
CLINICAL SYMPTOMS
According to Raiteri et al. (2022), Celiac Disease (CD) poses a true diagnostic challenge. The disease can manifest at any age and has a broad spectrum of clinical presentations, including symptomatic, intestinal, and extraintestinal forms, as well as asymptomatic cases detected through complementary tests.
A study based on screening tests demonstrated that 50 to 70% of celiac children are asymptomatic (GOBBO, 2018). Mosca et al. (2022) also warn that, due to the fact that routine screening for CD is not offered to the general public, many people have little awareness of the disease and remain undiagnosed.
Traditionally, CD has been considered a cause of malabsorption, leading to a common clinical picture in children, typically including chronic diarrhea and growth retardation. Atypical manifestations, common in adults, may initially present with symptoms such as iron-deficiency anemia or osteoporosis (LASA, 2018).
Gobbo (2018) explores the symptomatology, showing its variation, ranging from classic signs of malabsorption syndrome such as chronic diarrhea, abdominal distension, muscle atrophy, weight loss, hair changes, stunted growth, and vitamin deficiencies to nonspecific and extraintestinal symptoms, such as dental enamel defects, dermatitis herpetiformis, refractory iron-deficiency anemia, folic acid deficiency, arthritis, delayed puberty, infertility, neurological diseases, and intestinal lymphoma.
Oliveira (2018) writes that in response to these various modes of presentation, experts have created the Oslo Classification, which subdivides the disease into classical, non-classical, and asymptomatic or subclinical presentations. Classical CD is demonstrated by signs and symptoms of malabsorption, while the non-classical form is characterized by other gastrointestinal symptoms, besides diarrhea, and extraintestinal clinical features. Subclinical disease is described as being below the threshold of clinical detection. Potential Celiac Disease designates the condition of patients who have a future risk of developing the disease.
Neurological disorders are notably frequent in celiac individuals who do not even have gastrointestinal symptoms. Peripheral neuropathy manifests through paresthesias and pain that begin in the extremities. It is suspected in the absence of other causes when there is positive serology. In gluten ataxia, patients exhibit limb incoordination, unstable gait, poor coordination, severe fine motor skills impairments, and speech and vision problems. It also appears to be idiopathic and is related to the presence of anti-gliadin antibodies (VINAGRE-ARAGÓN et al., 2018; S MEARNS et al., 2019).
There is an association between CD and epilepsy, as CD is twice as prevalent in epileptics compared to the general population, with a higher prevalence of epilepsy in celiac individuals as well (ROUVROYE et al., 2020).
Hematological alterations are common in CD, such as anemia, coagulopathies, thromboembolism, and thrombocytopenia. Anemia can be microcytic due to iron deficiency or macrocytic due to a lack of vitamin B12. Thrombocytopenia is usually associated with autoimmune manifestations (PANTIC et al., 2022).
According to Binicier (2020), due to its autoimmune nature, CD is often associated with other autoimmune diseases. Therefore, in diagnosed cases, especially after the age of 40, screening for autoimmune, endocrine, and rheumatic comorbidities is recommended.
Dermatitis Herpetiformis (DH), a chronic autoimmune skin disorder caused by gluten hypersensitivity, is referred to as a cutaneous manifestation of CD. Its clinical presentation includes papulovesicular lesions, crusty lesions, itching, and burning, primarily affecting the elbows, knees, and buttocks. Gastrointestinal symptoms are not common in patients with DH (DO VALE et al., 2019).
Balaban et al. (2019) also describe a rare clinical entity that is potentially fatal. This is Celiac Crisis (CC), which can affect both children and adults. CC begins abruptly with profuse diarrhea, leading to severe dehydration, hemodynamic instability, and significant electrolyte and metabolic disturbances, necessitating hospitalization and intensive support.
DIAGNOSTIC STRATEGY
The absence of a “gold standard” test for the diagnosis of Celiac Disease (CD) indicates that isolated clinical, serological, or histological features are not sufficient to define the condition (RAITERI et al., 2022). The best way to diagnose CD is by combining different practices, such as observing the patient’s diet, testing for immunoglobulins, and performing intestinal biopsy (MARTÍNEZ-RODRIGUEZ et al., 2020).
Raiteri et al. (2022) point out that various guidelines agree that the approach to diagnosing CD should follow a sequential logic, starting with a suggestive clinical presentation, followed by serological tests, and ultimately, intestinal biopsy obtained by digestive endoscopy in the case of a positive serology or in the case of persistent malabsorption, even if serologically negative.
Serological markers can be used as screening methods, diagnostic support, or in the evaluation of treatment response. The tests for anti-tissue transglutaminase antibodies (anti-tTG) and anti-endomysium antibodies (anti-EMA) are the most commonly used in clinical practice (LABRADA et al., 2020).
The measurement of IgA anti-tTG is the recommended initial test, with a sensitivity of 98% and specificity of 96%. The IgA anti-EMA test has similar parameters. Elevated levels of these antibodies are almost always associated with typical celiac enteropathy. In individuals with IgA deficiency, serological tests should be based on the determination of IgG anti-tTG, IgG anti-EMA, and/or IgG anti-gliadin. Therefore, the summarized serological testing sequence is: measuring total IgA and IgA anti-tTG; measuring IgA anti-EMA if anti-tTG has a low titer; and measuring IgG anti-tTG, IgG anti-EMA, and IgG anti-gliadin in cases of IgA deficiency (GOBBO, 2018).
Ferreira (2018) also explains that the definitive diagnosis is based on the confirmation of histological changes in the mucosa of the small intestine from biopsies collected in the duodenum. The expected histological changes in CD are villous atrophy or absence, crypt hyperplasia, and lymphoplasmacytic infiltration in the lamina propria. However, there is still ongoing debate about the necessity of performing duodenal biopsies in light of advances in serological marker detection techniques.
According to Labrada et al. (2020), the definitive diagnosis of CD is only considered when, in addition to symptoms associated with positive serology and characteristic histology, clinical improvement occurs after a gluten-free diet for at least two weeks.
Although not present in established guidelines, the “four out of five rule,” as mentioned by Raiteri et al. (2022), outlines a simple diagnostic model defined by the presence of 4 out of 5 criteria, including: 1- typical disease symptoms, such as malabsorption and diarrhea; 2- positivity for autoantibodies; 3- positivity for human leukocyte antigen (HLA) DQ2 or DQ8; 4- intestinal damage confirmed by biopsy; and 5- a response to a gluten-free diet.
Labrada et al. (2020) also emphasize the importance of healthcare professionals accessing new knowledge regarding CD management, different presentation patterns, and diagnostic criteria, as this would facilitate early recognition. According to their work, the average time from the onset of symptoms to diagnosis is 20 years.
TREATMENT
The immune response in Celiac Disease is triggered by the ingestion of gluten, and thus far, the only effective treatment available is a strict gluten-free diet (SOLDERA, 2021).
Dehghani et al. (2017) and Martinello (2017) make it clear that the definitive removal of gluten from the diet results in symptom remission, serological normalization, and restoration of intestinal mucosa.
In more detailed terms, LABRADA et al. (2020) reports, based on gluten-free dietary compliance, that symptoms regress after 2 weeks, serological titers normalize between 6 to 12 months, and intestinal villi recover in about 2 years following treatment initiation.
Without treatment, individuals with celiac disease are exposed to a high rate of morbidity and mortality, becoming susceptible to various complications, including osteoporosis, infertility, anemia, neurological disorders, and even cancer, with intestinal lymphoma being the most prevalent neoplasia (MARTINELLO, 2017).
According to Ferreira (2018), it is of paramount importance to educate patients within the dietary therapy about gluten-free food alternatives, reading product labels, and participating in support groups.
The cornerstone of treatment is the exclusion of wheat, oats, barley, and rye, as well as their derivatives, from the diet. It is likely that oats, by themselves, do not trigger harmful effects. However, products containing oats in their composition may be contaminated with gluten (LABRADA et al., 2020).
Regarding the challenges of maintaining a gluten-free diet, Bessa et al. (2019) demonstrated that most celiac patients in their study who followed a restricted diet were subject to therapeutic failures. These occurrences were related, among other factors, to the emergence of symptoms due to errors in diet compliance, the adoption of behaviors related to risk factors such as handling, preparing, and sharing meals in contaminated environments and with contaminated products, lack of hygiene, or separation of gluten-contaminated utensils, and the failure to check food labels.
Da Silva et al. (2020) reported that celiac patients with an annual income of less than $5,000.00 face difficulties in maintaining the recommended therapy. This demonstrates that purchasing power influences the adoption of a lifelong gluten-free diet. Processed foods that are safe for celiac individuals tend to have a higher cost compared to products that are known to contain or may contain gluten.
There are situations where the use of medicinal strategies is necessary. In the case of Dermatitis Herpetiformis, Da Silva et al. (2019) suggests combining medications with dietary restrictions during the initial years of treatment. Dapsone, which relieves itching within a few hours and improves skin lesions within days, is the drug of choice. As a second-line treatment, in cases of no response or problems with adverse effects of dapsone, sulfasalazine is considered. For itching, systemic corticosteroids and antihistamines have limited effects.
In the case of Celiac Crisis, Balaban et al. (2019) mentions the need for hospitalization to replenish fluids, correct electrolyte imbalances, and acid-base disturbances. Although there are reports that fuel the debate over the use of corticosteroids, an approach involving their prescription has been observed in practice.
CONCLUSIONS
The results showed that Celiac Disease (CD) has epidemiological relevance, and there is currently an increasing number of diagnosed cases. Adequate knowledge of the pathophysiology, the various clinical presentations, and the serological options for diagnosis is what enables better diagnostic accuracy.
Nutritional knowledge is also crucial for an effective therapeutic approach with a gluten-free diet, resolving symptoms, and preventing complications. Therefore, specialized multiprofessional care for individuals with CD is of great importance.
The large number of results obtained regarding CD reflects the significance of the topic and the significant progress in defining and characterizing the disease. However, the results still point to underdiagnosis, emphasizing the importance of continuous updates in CD studies.
REFERENCES
AKAY, Seval et al. Serum iron and vitamin B 12 deficiency could indicate celiac disease by flexible spectral imaging color enhancement. Revista Associação Médica Brasileira. v. 66, n. 6, p. 818-823, 2020. Disponível em: https://www.scielo.br/j/ramb/a/PKbgQDX5tCZ6sGYqRKKPZ5h/abstract/?lang=en. Acesso em: 28 out. 2022.
AL-ABACHI, Khaldoon Thanoon. Screening for Celiac Disease in Patients with Irritable Bowel Syndrome Fulfilling Rome III Criteria. Journal of Coloproctology. v. 42, n. 01, p. 20-24. 2022. Disponível em: https://www.scielo.br/j/jcol/a/kYN9nVMTnnx6cwbX57W636v/ . Acesso em: 28 out. 2022.
AL-BLUWI, Ghada S. M.et al. Prevalence of Celiac Disease in Patients With Turner Syndrome: Systematic Review and Meta-Analysis. Front. Med. 17. 2021. Disponível em: https://pubmed.ncbi.nlm.nih.gov/34222285/ . Acesso em: 28 out. 2022.
BAJOR, Judit et al. Classical celiac disease is more frequent with a double dose of HLA-DQB1*02: A systematic review with meta-analysis. Journal PLOS ONE v. 14, n. 2, 2019. Disponível em: https://pubmed.ncbi.nlm.nih.gov/30763397/ . Acesso em: 28 out. 2022.
BALABAN, Daniel Vasile et al. Celiac crisis, a rare occurrence in adult celiac disease: A systematic review. World Journal of Clinical Cases. v. 7, n. 3, p. 311-319, 2019. Disponível em: https://pubmed.ncbi.nlm.nih.gov/30746372/ . Acesso em: 28 out. 2022.
BARROS, Marina Carvalho de Azevedo. DOENÇA CELÍACA: REVISÃO BIBLIOGRÁFICA E RELATO DE CASO. Tese (Residência em Clínica Médica). Hospital do Servidor Público Municipal. São Paulo. 2019. Disponível em: https://docs.bvsalud.org/biblioref/2021/06/1247948/tcc-dc-marina-barros-final.pdf. Acesso em: 28 out. 2022.
BESSA, Cristina Costa et al. Health Control For Celiac Patients: An Analysis According To The Pender Health Promotion Model. Texto & Contexto Enfermagem. v. 29, 2019. Disponível em: http://www.revenf.bvs.br/scielo.php?script=sci_arttext&pid=S0104-07072020000100303. Acesso em: 28 out. 2022.
BINICIER, Omer Burcak; TOSUN, Ferahnaz. Evaluation of adult celiac disease from a tertiary reference center: a retrospective analysis. Revista Associação Médica Brasileira. v. 66, n. 1, p. 55-60, Disponível em: https://www.scielo.br/j/ramb/a/xjhbLPFB3cDVpnFLqJK3fJh/?lang=en. Acesso em: 28 out. 2022.
DA SILVA, Leonardo Alexandrino et al. Accuracy of the clinical indicators of ineffective health management in celiac people. Revista Brasileira de Enfermagem. v. 73, n.3. 2020. Disponível em: https://www.scielo.br/j/reben/a/hQXM6yfMq56Yz9rbSGFkT7t/?lang=en. Acesso em: 28 out. 2022.
DEHGHANI, Seyed Mohsen et al. The effect of gluten-free diet among celiac patients aged 3-12 years old on BMI during 2006 to 2014 at Nemazee Teaching hospital. Rev. gastroenterol. Perú. v.37, n.4, p.323-328. 2017. Disponível em: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1022-51292017000400005&lng=es&nrm=iso&tlng=en. Acesso em: 28 out. 2022.
DO VALE, Everton Carlos Siviero et al. Consensus on the treatment of autoimmune bullous dermatoses: dermatitis herpetiformis and linear IgA bullous dermatosis – Brazilian Society of Dermatology. Anais Brasileiros de Dermatologia. v. 94, n. 2 Suppl 1, p. 48-55. 2019. Disponível em: https://www.scielo.br/j/abd/a/wghvzvbYvdGcZfXvtws7qBb/?lang=en Acesso em: 28 out. 2022.
EL-METWALLY, Ashraf et al. The Epidemiology of Celiac Disease in the General Population and High-Risk Groups in Arab Countries: A Systematic Review. Biomed Res Int. 2020. DOI: 10.1155/2020/6865917. Disponível em: https://pubmed.ncbi.nlm.nih.gov/32596351/ . Acesso em: 28 out. 2022.
FERREIRA, Fátima; INÁCIO, Filipe. Patologia associada ao trigo: Alergia IgE e não IgE mediada, doença celíaca, hipersensibilidade não celíaca, FODMAP. Rev Port Imunoalergologia Lisboa v. 26, n. 3, p. 171-187. 2018. Disponível em: http://www.scielo.pt/scielo.php?script=sci_arttext&pid=S0871-97212018000300002&lang=pt . Acesso em: 28 out. 2022.
GOBBO, Letícia de Cácia Vilela. DOENÇA CELÍACA NA INFÂNCIA. Tese (Residência em Clínica Médica). Hospital do Servidor Público Municipal. São Paulo. 2018. Disponível em: https://docs.bvsalud.org/biblioref/2021/07/1281709/tcc-leticia-de-cacia.pdf . Acesso em: 16 out. 2022.
JULIAN, Thomas; HADJIVASSILIOU, Marios; ZIS, Panagiotis. Gluten sensitivity and epilepsy: a systematic review. Journal of Neurology, v. 266, n. 7, p. 1557-1565. 2019. Disponível em: https://pubmed.ncbi.nlm.nih.gov/30167878/. Acesso em: 28 out. 2022.
KHAN, Sahar et al. Another Chicken and Egg Story: Systematic Review on Lichen Planus as a Precursor for Celiac Disease in Adult Population. Cureus, v. 12, n. 8. 2020. DOI: 10.7759/cureus.9526. Disponível em: https://pubmed.ncbi.nlm.nih.gov/32775115/. Acesso em: 28 out. 2022.
KOTZE, Lorete Maria da Silva. KOTZE, Luiz Roberto. MORENO, Isabela. NISIHARA, Renato. Immune Mediated Diseases In Patients With Celiac Disease And Their Relatives: A Comparative Study Of Age And Sex. Arquivos de Gastroenterologia [online]. v. 55, n. 04, p. 346-351. 2021. Disponível em: https://www.scielo.br/j/ag/a/nmnJY6RHx48rnrFgwpJhcPc/abstract/?lang=en. Acesso em: 28 out. 2022.
KOTZE, Lorete Maria da Silva. MALLMANN Andyara. MIECZNIKOWSKI, Rebeca C. CHRISOSTOMO, Kadija Rahal. KOTZE, Luiz Roberto. NISIHARA, Renato. Reproductive Aspects In Brazilian Celiac Women. Arquivos de Gastroenterologia [online]. v. 57, n. 01, p. 107-109. 2020. Disponível em: https://www.scielo.br/j/ag/a/XhHk6FfFChhVMsFSnfdHzwp/?lang=en. Acesso em: 28 out. 2022.
KOTZE, Lorete Maria da Silva. KOTZE, Luiz Roberto. NISIHARA, Renato. UTIYAMA, Shirley R. R. SERONEGATIVE CELIAC DISEASE IN BRAZILIAN PATIENTS: A SERIES OF CASES. Arquivos de Gastroenterologia [online]. v. 58, n. 02, p. 214-216. 2021. Disponível em: https://www.scielo.br/j/ag/a/fDGHNyvYVB38SCYm3tTfWHy/?lang=en. Acesso em: 13 out. 2022.
LABRADA, Oleydis Brizuela et al. Doença celíaca em adultos. Um desafio no novo milênio. Multimed, Granma v. 24, n. 4, p. 949-968. 2020. Disponível em: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1028-48182020000400949&lang=pt. Acesso em: 28 out. 2022.
LADINO, Liliana et al. Detection of anti-tissue transglutaminase IgA antibodies (tTG IgA) in children with type 1 diabetes mellitus. Rev. Fac. Med. v. 68, n. 3, p.347-351. 2020. Disponível em: http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0120-00112020000300347. Acesso em: 28 out. 2022.
LASA, J.; RAUSCH, A.; ZUBIAURRE, I. Risk of colorectal adenomas in patients with celiac disease: a systematic review and meta-analysis. Rev. Gastroenterol. Mex. (Engl Ed). v. 83, n. 2, p. 91-97. 2018. Disponível em: https://pubmed.ncbi.nlm.nih.gov/29422261/. Acesso em: 28 out. 2022.
LAU, Wing-Yu Siobhan; HEATON, Paul Anthony; PAUL, Siba Prosad. Improved Adherence To The Espghan Guidelines Is Necessary For Diagnosing Celiac Disease In Children: A Single-Center Experience. Arquivos de Gastroenterologia. v. 58, n. 2, p. 164-167. 2021. Disponível em: https://www.scielo.br/j/ag/a/HShTnNYDsCWzFzV3RzPWY4z/?lang=en. Acesso em: 28 out. 2022.
MAHADEV, Srihari et al. Prevalence of Celiac Disease in Patients With Iron Deficiency Anemia-A Systematic Review With Meta-analysis. American Gastroenterological Association. v. 155, n. 2, p. 374-382. 2018. Disponível em: https://pubmed.ncbi.nlm.nih.gov/29689265/. Acesso em: 28 out. 2022.
MARTINELLO, Flávia; ROMAN, Camila Fontana; SOUZA, Paula Alves de. Efeitos do consumo de probióticos sobre as bifidobactérias intestinais de pacientes celíacos. Arquivos de Gastroenterologia. 2017. Disponível em: https://www.scielo.br/j/ag/a/hBLm56K3tvytnFT39vGSgbT/abstract/?lang=pt. Acesso em: 28 out. 2022.
MARTÍNEZ-RODRÍGUEZ, Alejandro et al. Tools Used to Measure the Physical State of Women with Celiac Disease: A Review with a Systematic Approach. International Journal of Enviromental Research and Public Health. v. 17, n. 2. 2020. DOI: 10.3390/ijerph17020539 Disponível em: https://pubmed.ncbi.nlm.nih.gov/31952137/. Acesso em: 28 out. 2022.
MOSCA, Caterina et al. Newly Diagnosed Celiac Disease and Bone Health in Young Adults: A Systematic Literature Review. Calcif Tissue Int. v. 110, n. 6, p. 641-648. 2022. Disponível em: https://pubmed.ncbi.nlm.nih.gov/34978602/. Acesso em: 28 out. 2022.
OLIVEIRA, Gracinda Nogueira; MOHAN, Rajiv; FAGBEMI, Andrew. Review Of Celiac Disease Presentation In A Pediatric Tertiary Centre. Arquivos de Gastroenterologia. v. 55, n. 01, p. 86-93. 2018. Disponível em: https://www.scielo.br/j/ag/a/4xJWVXZK8FHqn4c67FT5SKb/?lang=en. Acesso em: 28 out. 2022.
PANTIC, Nikola et al. Celiac Disease and Thrombotic Events: Systematic Review of Published Cases. MDPI Journals Nutrients. v. 14, n.10, 2022. Disponível em: https://pubmed.ncbi.nlm.nih.gov/35631302/. Acesso em: 28 out. 2022.
PRIETO, Jose et al. New Evidence in the Pathogenesis of Celiac Disease and Type 1 Diabetes Mellitus: A Systematic Review. Cureus, v. 13, n. 7. 2021. DOI: 10.7759/cureus.16721. Disponível em: https://pubmed.ncbi.nlm.nih.gov/34513356/. Acesso em: 28 out. 2022.
RAITERI, Alberto et al. Current guidelines for the management of celiac disease: A systematic review with comparative analysis. World Journal of Gastroenterology. v.28, n. 1, p. 154-175. 2022. Disponível em: https://pubmed.ncbi.nlm.nih.gov/35125825/. Acesso em: 28 out. 2022.
RATO, Beatriz; VERÍSSIMO, Manuel Teixeira. Doença Celíaca no Idoso. Medicina Interna, Lisboa. v. 28, n. 2, p. 53-61. 2021. Disponível em: http://www.scielo.pt/scielo.php?script=sci_arttext&pid=S0872-671X2021000200053&lang=pt. Acesso em: 28 out. 2022.
ROUVROYE, Maxine D. et al. The Neuropathology of Gluten-Related Neurological Disorders: A Systematic Review. MDPI Journals Nutrients. v. 12, n.3, 2020. Disponível em: https://pubmed.ncbi.nlm.nih.gov/32244870/. Acesso em: 28 out. 2022.
S MEARNS, Elizabeth et al. Neurological Manifestations of Neuropathy and Ataxia in Celiac Disease: A Systematic Review. MDPI Journals Nutrients. v. 12, n.11, 2019. Disponível em: https://pubmed.ncbi.nlm.nih.gov/30759885/. Acesso em: 28 out. 2022.
SHAHRIARI, Mahdi et al. Association Of Potential Celiac Disease And Refractory Iron Deficiency Anemia In Children And Adolescents. Arquivos de Gastroenterologia. v. 55, n. 01, p. 78-81. 2018. Disponível em: https://www.scielo.br/j/ag/a/q8dkSkf7MMGzmFc5y83zmpt/?lang=en. Acesso em: 28 out. 2022.
SOLDERA, Jonathan; SALGADO, Karina; PÊGAS, Karla Lais. Refractory celiac disease type 2: how to diagnose and treat? Revista da Associação Médica Brasileira. 2021, v. 67, n. 2, p. 168-172. 2021. Disponível em: https://www.scielo.br/j/ramb/a/Ry3SDkcmpzvRWzCWkppmZMS/. Acesso em: 28 out. 2022.
TEIXEIRA, Fernando Augusto Montanha; LOPES, Fernanda Oliveira de Andrade; MACHADO, Ana Paula de Souza Lobo. Dieta isenta de glúten e risco de desfechos gestacionais desfavoráveis em mulheres com doença celíaca: revisão sistemática. Sociedade Brasileira de Reprodução Humana – Reprodução & Climatério. v. 32, n. 2, p. 120-126. 2017. Disponível em: https://www.sciencedirect.com/science/article/pii/S1413208717300031. Acesso em: 28 out. 2022.
VINAGRE-ARAGÓN, Ana et al. Movement Disorders Related to Gluten Sensitivity: A Systematic Review. MDPI Journals Nutrients. v. 10, n.8. 2018. Disponível em: https://pubmed.ncbi.nlm.nih.gov/30096784/. Acesso em: 28 out. 2022.
WIJARNPREECHA, Karn et al. Cigarette smoking and risk of celiac disease: A systematic review and meta-analysis. United European Gastroenterology Journal. v. 6, n. 9, p. 1285-1293. 2018. Disponível em: https://pubmed.ncbi.nlm.nih.gov/30386601/. Acesso em: 28 out. 2022.
ZULLO, Angela et al. A Challenging Diagnosis of Jejunal Adenocarcinoma in a Celiac Patient: Case Report and Systematic Review of the Literature. Journal of Gastrointestinal and Liver Diseases. v. 26, n. 4, p. 411-415. 2017. Disponível em: https://pubmed.ncbi.nlm.nih.gov/29253057/. Acesso em: 28 out. 2022.
[1] Medical student at the Federal University of Amapá (UNIFAP).
[2] Medical student at the Federal University of Amapá (UNIFAP).
[3] Medical student at the Federal University of Amapá (UNIFAP).
[4] Biologist, Ph.D. in Theory and Research of Behavior, Professor, and researcher in the Chemistry Teaching degree program at the Institute of Basic, Technical, and Technological Education of Amapá (IFAP), in the Professional and Technological Education Graduate Program (PROFEPT IFAP), and in the Biodiversity and Biotechnology Graduate Program of the BIONORTE Network (PPG-BIONORTE), Amapá branch.
[5] Physician, Master of Teaching and Health Sciences, Professor, and researcher in the Medicine program at the Macapá Campus, Federal University of Amapá (UNIFAP).
[6] Ph.D. in Psychology and Clinical Psychoanalysis. Ph.D. in progress in Communication and Semiotics at the Pontifical Catholic University of São Paulo (PUC/SP). Master’s degree in Religious Sciences from the Mackenzie Presbyterian University. Master’s degree in Clinical Psychoanalysis. Bachelor’s degree in Biological Sciences. Bachelor’s degree in Theology. With over 15 years of experience in Scientific Methodology (Research Methods) in guiding the Scientific Production of Master’s and Ph.D. students. Specialized in Market Research and Health-related Research. ORCID: 0000-0003-2952-4337.
[7] Biologist, Ph.D. in Tropical Diseases, Professor, and researcher at the Physical Education Department, Federal University of Pará (UFPA).
[8] Biomedical scientist, Ph.D. in Tropical Diseases, Professor, and researcher at the Medicine Department, Campus Macapá, Federal University of Amapá (UNIFAP), and at the Postgraduate Program in Health Sciences (PPGCS UNIFAP). Also, the Vice Dean for Research and Postgraduate Studies (PROPESPG) at the Federal University of Amapá (UNIFAP).
Submitted: October 2022.
Approved: October 2022.