ORIGINAL ARTICLE
MARCHESINI, Simone Dallegrave [1]
MARCHESINI, Simone Dallegrave. Intervention based on mindfulness and body image in patients undergoing bariatric surgery. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year. 07, Ed. 02, Vol. 06, pp. 17-39. February 2022. ISSN: 2448-0959, Access Link: https://www.nucleodoconhecimento.com.br/psychology/patients, DOI: 10.32749/nucleodoconhecimento.com.br/psychology/patients
ABSTRACT
After treatments for loss of large amounts of weight, the dissatisfaction with body image and the lack of recognition of the body itself is recurrent. These factors are elements of study due to the difficulties encountered in maintaining the results, in the long term, also in the surgical treatment of obesity. The lack of identity with the new form and dissatisfaction with body image have been pointed out as maintaining factors of poor eating habits and emotional eating that leads to weight recurrence. In this sense, the interest was raised as to whether: Would small mindfulness interventions have the ability to improve body image and favor the recognition of body distortions, in order to prevent weight recurrence in patients undergoing bariatric surgeries? This article aims to investigate the applicability of small mindfulness meditative strategies in the prevention of weight recurrence in bariatric patients. The method presented is a case report through 12 weekly meetings with a female client, 48 years of age, preoperative BMI of 42 Kg/m2 and postoperative BMI of 21.67 Kg/m2. The themes of the meetings were: psychoeducation about bariatric surgery, family approach, evaluation and psychoeducation about cognitive patterns, assessment of body image and body identity through photo composition. The other meetings were distributed among the small practices of mindfulness: breathing, movement, eating with mindfulness and body scanning. The practices demonstrated efficacy in reducing the discrepancy between the internal subjective perception of the body (interoception) and body image (exteroception). There was a positive experience of the body outside the aesthetic requirements, achievement of greater identity with body shape, exit from the perfectionist pattern and evaluation improvement of body shape and size. The small mindfulness-like meditative strategies have been shown to be effective in cognitive behavioral therapy for the prevention of weight recurrence in bariatric patients.
Keywords: Cognitive-Behavioral Therapy; Body Image; Mindfulness; Bariatric Surgery; Weight Recurrence.
1. INTRODUCTION
The current culture remains prejudiced against obesity and overweight despite efforts of body release movements and acceptance of diversity. The social concept about people living with excessive weight remains linked to the failure of willpower, without ever questioning the genetic inheritance or weakness of health. A more recent perspective referred to by Frederick et al. (2019) admits obesity as a disease and with defined heredity. From this perspective, weight control would not be entirely the responsibility of the patient, but multidimensional. These two frameworks, however, determine positions that stigmatize the individual, or as incapable in the face of the voracious behavior of obese people, or as a sick individual in the face of a genetic predisposition.
The framework of Cognitive-Behavioral Therapy observes some common characteristics in overweight and obese individuals.They are thought patterns that are repeated, interfere in the interpretation and quality of life, in the maintenance of eating symptoms, as well as in dissatisfaction with body image. In this sense, the change in rigid patterns of perception, thought and feeling open the possibility of an active and effective role for those who seek mental health beyond weight loss (SALA; VANZHULA; LEVINSON, 2019).
Freeman and De Wolf (1992) presented the automatic and repetitive thoughts that most impact on the determination of the behavior of overweight individuals. These distortions of cognition, which are errors of access and interpretation of reality, are the basis of troubled relationships with food, body image and the world.
According to Fairburn (2011) the dysfunctional self-assessment scheme, problems related to rigid eating patterns, dissatisfaction and distorted interpretation of body image itself are the central aspects of the problem of eating disorders that may or may not accompany obesity. This pattern of functioning involves perfectionism, leads individuals to minimize their positive achievements, magnify failures and potentiate lapses. In addition, it resonates with great magnitude on their self-concepts and self-esteem, and contributes to weight recurrence.
In this sense, the interest is raised as to whether: would small mindfulness interventions have the ability to exercise body image improvement and favor the recognition of body distortions, in order to prevent weight recurrence in patients undergoing bariatric surgeries? This article aims to investigate the applicability of small mindfulness meditative strategies in the prevention of weight recurrence in bariatric patients. For this, a case report was presented in a 48-year-old female client with pre-surgical BMI of 42 Kg/m2 and post-surgical of 21, 67 Kg/m2 attended in 12 meetings, in a weekly scheme divided into 6 pre-surgical and 6 post-surgical meetings. The themes of the meetings were: psychoeducation about bariatric surgery, family approach, evaluation and psychoeducation about cognitive patterns, recording of dysfunctional thoughts, evaluation of body image and body identity through photo composition. The other meetings were distributed among the mindfulness practices: breathing, movement, eating with mindfulness and body scanning.
The small interventions of Mindfulness strategies are practices taken from the eight-week program that intend acceptance in relation to thoughts, sensations or emotions that may arise in the face of internal and external perceptions of the body. The training of the exemption from judgment, typical of these practices, is a primordial posture for the gentle and curious approach to what arises moment by moment.
Changes in eating behavior tend to trigger all-or-nothing thoughts. These thoughts are manifest in the violation of rigid self-imposed diets and result in impulsive attitudes radically contrary to programmed dietary restrictions. Regarding obesity itself, thoughts are catastrophic (“Being fat is worse than having cancer”), while the sense of potency in the face of the problem is minimized (“I can’t! It’s no use even trying!”). Selectively abstract professional recommendations and disqualify family help (“The nutritionist said nothing new! My mom keeps getting in the way and just gets in the way.”). They faithfully believe in a widespread and negative pattern about their situation (“It’s no use, it’s no use to me!”; “I’ve tried everything you can imagine.”) (BACALTCHUK; HAY, 2004).
People with long periods of overweight and obesity often incur cognitive distortion called “thought reading”. This distortion is shown by the certainties of being rejected and suffering debauchery or discrimination in groups and situations of exposure (“They look at us as if we want to be fat, it seems that they are disgusted with us!”).These people internally carry the sense of obligation and duty to fulfill the expectations of thinness imposed by the prevailing culture (“I should not have ate so much. I had to control myself. Everyone stares when it’s a fat guy who’s eating!”).
According to the study by Sarwer et al. (2019) obese people, particularly those who seek bariatric surgeries, are likely to have mood disorders and eating disorders. The presence of these psychopathologies in the preoperative period influences the results of weight loss and the maintenance of results. These disorders include symptoms of binge and/or dietary restriction, excessive concern with the theme of food and the body, dissatisfaction with weight and body shape, clinical perfectionism, depression and/or anxiety.
On the other hand, the thought patterns that are recurrent in individuals in the process of weight recurrence cover the themes of food, body and control. They worry excessively and present a distortion called “cognitive fusion form/thought” that makes them jump from the imagination of excess quantitative intake of caloric foods to the feeling of being fat (DA LUZ et al., 2017).
Geller et al. (2019) explain that in bariatric patients the body mass index (BMI) is related to the prevalence of suicide, but that not all are susceptible to this factor. Other interferences are present, with body image being the most related factor to stressful events and eating behavior used to regulate unpleasant emotions. Thus, observing the so-called episodes of “emotional eating” becomes an important indicator of a bad relationship with the body itself and its image.
Fairburn (2011) states that cognitive-behavioral psychotherapies favor improvement of symptoms and symptom-maintaining factors, so they promote significant results that can be maintained over one to two years of follow-up. The same author states that acting on the factors maintaining symptoms rather than seeking the causes is one of the strategies used in Cognitive Behavioral Therapy of Eating Disorders and Obesity. Among these factors are: dissatisfaction with body image and loss of control at the time of eating. In Compulsive Eating Disorder as much as nervous bulimia, these factors should be considered.
According to Preston and Ehrsson (2014) the perceived body refers to how the individual perceives and evaluates his body; the recording of body image according to Gao et al. (2016) is the representation of body image in the human brain.
2. DEVELOPMENT
2.1 BODY IMAGE, EATING AND WEIGHT RECURRENCE: THE REPEATED CYCLE OF WEIGHT CONTROL
Mindfulness meditation, in the conceptualization of its creator Kabat-Zinn (2005), is the practice of intentionally focusing attention on the experience of the present moment. This attitude of focused will occurs with receptivity and acceptance without judging what is happening or clinging to the way this experience should or should not be.
Avoiding contact with the body, wearing loose clothes, weighing, dodging mirrors and avoiding social contact are behaviors that aim to prevent provocative situations of anxiety in relation to physical appearance (ALBERTS; THEWISSEN; RAES, 2012). On the other hand, mindfulness meditative practices, considered short interventions, favor improvements in body perception, assessment and conceptualization of oneself, and in the relationship with body image (ALBERTSON; NEFF; DILL-SHACKLEFORD, 2015).
In patients who lose large amounts of weight, Ramalho et al. (2014) and Busetto et al. (2018) refer to the occurrence of multiple improvements in general health, but the tendency of body image to suffer negative repercussions and even be the basis of weight recurrence.The excess of skin resulting from the loss of body volume leaves the memory of obesity, impairs aesthetics and favors well-being with the return of fat as a plastic resource.
In a study by Bastos et al. (2014) conducted with the Portuguese population, the incidence of weight recurrence was up to 40% in bariatric operated patients, which makes the subject a concern. In Brazil, 105,642 bariatric surgeries were performed in 2017 according to the Brazilian Society of Bariatric and Metabolic Surgery (SBCBM) with data obtained from the Hospital Information System and DATASUS[2]. The increase in the annual average in the number of surgeries in Brazil was 13.5% and together with this amount, weight recurrence rates also increased.
Regardless of whether or not there is an understanding of the biological, genetic and psychological aspects involved in the process of weight loss and recovery, Velapati et al. (2018) comments that there seems to be an unfilled gap in the treatment of people living the frustrating cycle of chronic disease control that is obesity. This fact anchors the need for further studies that favor the recognition of internal resources for the management of impulsivity in feeding, new body image and self-esteem.
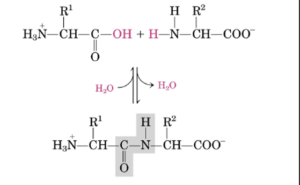
Roux-en-Y gastric bypass surgery has shown efficacy in the treatment of severe obesity. Christou et al. (2006) and Pizato et al. (2017) cite important statistics and report that 93% of those operated maintain less than 10% of the initial weight and 40% maintain 30% of the weight lost in 12 years. The reduction of the gastric reservoir that occurs in bariatric surgeries promotes metabolic alterations whose difference depends on the presence or absence of intestinal deviation and the type of this deviation. Dimitriadis et al. (2017) report that changes in anatomy caused by different surgical techniques favor the reduction of hunger hormone secretion (ghrelin), in the increase of appetite-regulating peptides, and may alter insulin secretion with improved Diabetes Mellitus-2, among other changes.
Reducing dissatisfaction with body image and favoring greater stability of long-term results is a necessary job that is not being performed in bariatric surgery. The lack of management of physiological perceptions (interoceptions) for greater control of impulsivity, the improvement of self-esteem and the assimilation of the new body image may be in the set of justifications for the problem of weight recurrence.
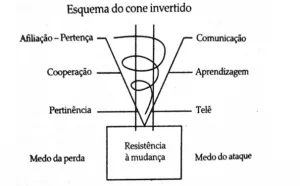
Meditative practices were effective in improving the interoceptions (physiological sensations). According to Cella et al. (2019) obese and overweight individuals with eating problems are impoverished by the body’s internal perceptions. Fischer et al. (2017) report that there is an effective experience of interventions such as “body scanning” or body scan in the format of eight weeks in group, which proved effective in increasing interoception when compared with control groups. Body signals such as heartbeat or breathing, once focused and observed without interference, through long-term body scanning practices (20 minutes), led to improved interoceptive accuracy. The perceptual levels measured with the subscale “interoceptive awareness” and the “Food Disorder Inventory-2” demonstrated the results.
People with obesity and eating problems describe impoverished awareness and distorted perception of states of hunger and satiety. In individuals who have loss of control at the time of eating, more frequent and greater sensation in patients with Compulsive Eating Disorder, the perception and awareness of hunger and satiety are worse. This phenomenon occurs due to gastric hormones, but also suffers influence from low perceptual accuracy that impairs interception. These same individuals have low esteem and impulse dysregulation (CELLA et al., 2019).
According to Vaitl (1996) and Herbert et al. (2012) hunger and satiety are classified as interoceptions because they refer to the perception of physiological sensations of internal organs, in this case the “interoceptive accuracy” of gastrointestinal signs.
The enteric nervous system, also known as the brain-intestine axis, is significantly affected by bariatric procedures. The sensations of hunger, satiety, and even the effect of empanzinamento that is caused by excess food are determined by the limit of the gastric space imposed by the surgical technique, the decreased secretion of Ghrelin and other hormonal changes.
Badoud and Tsakiris (2017) investigated the correlation between interoception and body image from behavioral and neuroimaging data. From there they traced a correlation between the perceived sensations about the physiological conditions of the own, sensations of the internal organs, and body image, the one that concerns the perception, feelings and attitudes about the body itself.
Badoud and Tsakiris (2017) explain how perceptions of internal organs (interception) affect identity formation, as well as the perception of the body itself (exteroception). This is because the interception gives sensations of homeostase and balance that ensure the biological stability of the organism and that are also linked to emotional regulation.
Cella et al. (2019) report that emotional stability is deregulated in people with disturbed eating behaviors, as occurs in biological functions. The authors also explain that this emotional instability is a predictor of compulsive eating episodes and other dietary disorders.
In obese candidates for bariatric surgery with binge eating and who participated in the study by Cella et al. (2019) it has been demonstrated that regulating impulses, decoding emotions and discriminating physiological sensations involves interception (perception of heartbeats, changes in breathing, perception of skin temperature, sweating, gastrointestinal sensations such as hunger, etc.) and that these are functions closely related to processes and patterns of thought.
Mindfulness-type meditation practice allows actions to go out of the automatic mode they usually are. The time of the experience in mindfulness is in the here and now, therefore, in the present moment. That doesn’t mean memories and fantasies can’t come up. What changes is the attitude of observation in the face of these memories, fantasies or concerns. The flow of thought and sensations is observed and contemplated without seeking changes. (KABAT-ZINN, 2005).
There is an intention of receptivity and acceptance in relation to thoughts, sensations or emotions that may arise in mindfulness practices. Nothing is rejected or even qualified as negative or good. The absence of judgment is a primordial posture for the gentle and curious approach to what is emerging.
Curiosity must be like that of a beginner or that of a child who explores the world. The explorer and curious look is invited to open up to the amazing. What comes is well received, without judgment, with a gentle attitude, free to follow the flow. Nothing should be retained or imprisoned, with an attitude of detachment.
Time here and now undoes the experience of expectations regarding how it should, or should not be. At the same time, gratitude allows there to be a positive and gentle perspective on the facts of life and with human nature itself.
Tylka and Barcalow (2015) point out that in psychological therapy it is not enough to eliminate the conception of negative body image, but it is necessary to help in the development of a positive posture with the body. They highlight that the positive body perspective involves appreciation and respect for one’s own body, as well as the ability to celebrate and honor it. To go from negative to neutral posture would just move from “I hate my body” to “I tolerate my body”.
In this sense, interventions to promote acceptance and body appreciation are important in the practice of psychotherapy of individuals who have dissatisfaction with body image; factor of maintenance of upset eating, experience of lack of control and obesity.
3. METHOD
The present article is a case report attended in a private clinic for a period of twelve weeks, divided into two stages: six preoperative meetings and six postoperative meetings. Long-term postoperative follow-up is being continued in monthly meetings.
The service began in September 2017. The client is female, at the time at 48 years of age, BMI 42 Kg/m2 (obesity grade III). Its maximum weight was 108 kg and its height 1.60 m. Its minimum weight after surgery was 55.5 Kg (BMI=21.67 Kg/m2). She was recommended for bariatric surgery by the endocrinologist after several attempts at partial weight loss. She presented total weight recurrence and increased kilograms at each diet. His clinical and metabolic examinations justified the option for bariatric surgery. The option surgery was of the mixed type: gastric bypass with Roux-en-Y intestinal bypass.
The preoperative sessions consisted of the evaluation of criteria described by Sarwer et al. (2014) as relevant points in patients who are candidates for bariatric surgeries. Items of the Bariatric Psychology Protocol of the Brazilian Society of Bariatric and Metabolic Surgery (2014) were also addressed.
The survey of the history of obesity and traumatic factors in the lifeline allowed the finding of possible situations that contributed to the triggering of the disease. The evaluation of previous attempts to lose weight and interference of the quality of family engagement in these treatments. The evaluation of the postures of the family and the client himself in the face of emotional problems brought perspective to the success of the future surgical treatment.
The personal and family history regarding the use or abuse of alcohol and psychoactive substances made it possible to suppose behavioral possibilities, as well as helped in the realization of a possible migration from obesity to alcohol dependence beyond the anatomical and physiological facilitators of surgery.
Also important conditions were the socio-biographical data, economic conditions, level of education, awareness about the procedure performed, resilience, the presence of psychiatric diagnosis, including the presence or absence of eating disorders.
The client’s history indicated the beginning of weight gain at thirteen years of age after menarche and lack of guidance on the natural biological processes of the woman. The parents were in marital conflict and the client revealed that she ate to relieve himself of the bad sensations she had when witnessing the couple’s fights. The mother charged her for a placement in her favor as the conflict revolved around the discovery of paternal adultery. The genetics for obesity was of paternal origin (grade III obese grandmother). According to reports, the client’s father was abusively using alcohol, but she herself did not exaggerate alcohol or use substances. He denied that he had been sexually abused or bullied at school due to obesity. He referred to discontent with his own body and lack of identity with his obese image. You’ve always pursued a skinny profile you’ve never been able to keep.
The client is married and has two children. Both the husband and the children showed jealousy about her and, although they expressed support for bariatric surgery, they expressed fear for possible changes in the client’s self-esteem and autonomy. Comments about possible betrayal after weight loss was made by the husband.
When he underwent diets, in the past, family members charged him control in food intake and physical exercise, but did not collaborate as to deprive her of making sweets or pasta to serve them. In an attempt to lose weight, the client made use of many appetite suppressants that are now banned on the market, as well as antidepressants. He also used diuretics and laxatives, all integrated into the formulas for weight loss.
He reported having had binge eating with episodes that always occurred at the end of treatments for weight loss. He had bouts of loss of control when eating and only interrupted food intake when he was ill. He gained weight very quickly, regained the weight lost in diet programs and always gained a percentage of increase.
4. INTERVENTIONS
4.1 PSYCHOEDUCATION ON BARIATRIC SURGERY
Colom and Vieta (2006) refer to psychoeducation as a tripod-based strategy of collaboration, information and trust.This strategy aims to provide knowledge about the problem to be addressed; develop resources so that the person himself can monitor his symptoms; provide an active role in the treatment itself and allow attention to the initial signs of worsening of the disease to favor the search for new treatment as soon as necessary.
In a review article Frederick et al. (2019) found thirty-one articles in which psychoeducation appeared as the main strategy used in the preparation of patients for bariatric and metabolic surgery. It is an internationally known and used resource.
In the present case, all mechanisms of Roux-en-Y gastric bypass surgery were clarified. The technique was presented as mixed, restrictive action (smaller stomach) and disabsorptive action (lower absorption of nutrients ingested due to intestinal deviation). Due to these characteristics, the client was oriented on the need for nutritional supplementation for the replacement of vitamins, minerals and proteins. All questions about the surgery had room for clarification at this stage. The predominant concern was with general anesthesia and hair loss in the postoperative period.
Orientations were made on future and new habits that impact surgical success, such as: abundant chewing, slow eating and attention to the new gastric space (to avoid entactions and/or vomiting), serving of meals, prioritization of taste rather than the amount of food, restriction of soda and pasty foods and partial prohibition of alcoholic beverages.
The unpleasant effects of surgery (get stuck, dumping, nutritional supplementation, loss of muscle mass) were all reported, with emphasis on dumping that occurs through ingestion of foods sweetened with sucrose, rich in simple carbohydrates or with high concentrations of fats. Dumping may take place immediately after or up to one hour after the consumption of such food. May cause diarrhea, feeling sick, drowsy, feeling faint, sweating, shorty.
Finally, issues related to alcohol intake, alcohol dependence and weight recurrence were addressed. Unlike food that is not absorbed and needs supplementation, alcohol is absorbed integrally and very quickly. This effect can promote faster brain gratification effects (disinhibition and relaxation), alcohol dependence, and unwanted effects on those who drink.
4.2 FAMILY CONSULTATION
The family sessions aimed to evaluate the family relationship, the understanding of obesity, their willingness to care for the client in the postoperative period, psychological support, financial capacity for the special care period (liquid, pasty, bland; help for dressing and bathing; returns to the multidisciplinary team; nutritional supplementation).
The family relationship was tense due to the interpretation of obesity as lack of control and bad personal habits. The macho perspective of the family environment attributes to the woman the concept of figure responsible for the house. A pattern of obese woman, with low self-esteem and readiness to serve others. Family members associated weight loss with excessive freedom, exhibitionism and female vanity. However, there was availability for the care of the client, due to its clinical picture.
Psychological support proved to be fragile, but the family bond with the team was good, which favored the commitment to return consultations. The availability of nutritional supplementation was guaranteed, given the commitment to health maintenance.
4.3 EVALUATION AND PSYCHOEDUCATION OF COGNITIVE STANDARDS
The assessment of cognitive patterns is a type of self-monitoring task also known as The Dysfunctional Thoughts Registry (RPD)[3]. This activity consists of annotating the frequency and context of behaviors for which one wants to arouse greater attention and awareness, and understanding of the links between environmental events, spontaneous thoughts and sensations. In the research by Frederick et al. (2019) this type of strategy appeared in twenty-eight articles and was considered the second cognitive-behavioral strategy most used in obesity treatments and bariatric surgery.
4.4 RECORD OF THOUGHTS, FEELINGS AND ATTITUDES OF EATING (EVALUATION OF SYMPTOMS: EMOTIONAL EATING, BINGE EATING, ANXIETY, DEPRESSION)
The recording of dysfunctional thoughts and the distinction between events, thoughts and feelings focused on cognitive restructuring. For Leahy (2017) it is from a new meaning and meaning that it is possible to increase motivation for short- and long-term changes. This intervention allows the perception of the automaticity of unrealistic and evidence-based thoughts. The opposition of automatic thoughts with rational patterns is a possible resource through strategic questions that lead the client himself to verify the existence of other possibilities of cognitively conceiving the same reality.
It was possible to observe that the “All or Nothing” thoughts related to the diet frequently appeared in the register of the client who was aware of the date of the surgical procedure and the results promoted about weight loss. “Since I’m going to operate, I’m going to eat everything I want”; “Since I’m never going to be able to eat again, I’m going to say goodbye to what I like.”
In order to search for elements of factual reality, the patient was also instructed to conduct research of patient statements in groups of bariatric operated, and to seek data on the postoperative diet in professional reports on the Internet. More ingrained and persistent beliefs about weight loss could be confronted with rational thoughts and scientific evidence, both detached from the therapist’s simple statement. The themes were: the false belief of weight loss from day to night; loss of body fluid; the idea that the weight gain process takes place in a single meal out of the pattern; caloric equivalence to the gain of 1 kg.
4.5 EVALUATION OF BODY IMAGE AND BODY IDENTITY THROUGH COMPOSITION OF PHOTOS REQUESTED OF THE PATIENT: CONSTRUCTION OF CHILDHOOD TO THE PRESENT DAYS OF THE HISTORY OF BODY IMAGE
Photos chronologically corresponding to the weight gain history were requested to evaluate the body image. There was a possibility of constructing a postoperative image according to BMI that progressed over time. In a second moment, with increased muscle mass, volume gain and healthy body design could be differentiated from the body with excess fat.The aim of this intervention was to promote coping with one’s own body image and decreased anxiety about body volume, since volume does not correspond to the amount of fat.
At this stage, short interventions were initiated in Mindfulness: self-assessment in front of the mirror in the company of the therapist and introduction to the practice Mindfulness breathing in three minutes.
In relation to the body, small interventions aim at functional reality, living and full as opposed to perfection.
The resources of kindness and compassion help in the reduction of judgment and critical function, typical of clinical perfectionism in eating disorders. They are practices focused on sensations and body perceptions in the present moment, mainly with a focus on breathing and developed in Mindfulness-Based Cognitive Therapy (SEGAL; WILLIAMS; TEASDALE, 2013).
4.6 INTRODUCTION TO MINDFULNESS INTERVENTIONS
The practice of Mindfulness breathing consists of sitting in a comfortable position and at the same time with the upright but not rigid spine. The focus is taken to the body sensations and to the perception of possible tensions. Then the mind is invited to rest in the breath, without changing it. If thoughts pass through the mind, just watch them and not follow them. The mind is all breath: it breathes, exhales, in a natural cycle.
The following invitation is to remain in the respiratory flow and detachment from thoughts to gently expand attention to the body as a whole and broaden the perception from the body in the environment to the environment in which the body is.
The following practice is Mindfulness walking: walking gently and slowly, with your eyes adred, with wide attention on every movement of the body: the exit of the foot from the ground, the transfer of weight from one leg to another, the foot support further on the ground, the knee flexion of the posterior leg, the progressive retained of the foot from the ground (from the posterior leg), the movement of the arms, the exit towards the front of the body, etc. Moment by moment the consciousness of walking.
Eating in a meditative state (practice of chocolate raisins or walnut): is an invitation to assume a respectful, erect and non-rigid posture to observe food in the palm of the hand. Then pay close to the shape, smell, color, texture, nuances and sounds of what will be ingested.
The path of cultivation of food to the table increases gratitude. Mentally monitoring the entire process of planting, harvesting and processing that this food went through until it reaches the table helps in understanding the interdependence between all things. Awaken the collaborative whole in the availability of food until the transformation in what is presented in the here and now.
It is useful for the interception the perception of the existence of hunger and its body location. Where is it located? Imagine the anatomy of the new surgically constructed stomach and realize its messages. Tune in to the visceral signals and see if there is hunger in the stomach. Continue with the nine types of hunger: hunger of the eye, nose, ear, hand and tongue (touch and taste), mouth, head and cells. The following practice is called “body scanning” or body scan and consists of inviting yourself to map the body like a scanner. The practice involves consciousness in each part of the body with onset on the left foot. The direction should be from the lower limbs toward the head, always alternating from the left limbs to the right ones.
Next, the introduction to the practice of self-compassion and love for the functional body. It is a call to mind to settle with breathing in three minutes and gently evoke a welcoming image (either). The feeling of welcome is invited to remain so that good wishes are desired to themselves in the same way as to someone you love. Within this climate of welcome, kindness and compassion the therapist guides the vows: That I may be well, that I may be happy, that I may follow with peace.
The post-surgical sessions repeated psychoeducation and mindfulness meditative techniques focused on the body (breathing, walking, body scan and self-compassion) whenever necessary.
The exploration of the physiological sensations of the body (interception) including hunger, satiety, desire to eat, satisfaction, restlessness, sleep, and emotions and feelings with records and location in the body were part of this stage: where is hunger? Where does the seat feel? In the throat? In the stomach. The hunger is the nose, it comes from the smell? The hunger is of the eye, it comes from the aesthetics of food?
5. RESULTS
In the course of the 12 sessions it was possible to perform the short interventions in Mindfulness that allowed the experience of the body outside the aesthetic requirements. The interoceptions have been trained to favor the recognition of the body in the here and now. The guided strategies allowed the client the experience of pleasurable sensations in addition to eating.
With weight loss, the client showed a greater identity with the shape and size of the body, but there was a worsening regarding the sequelae related to excess skin. This was a reason for recontracting and considerations about reconstructive surgery.
The small interventions in Mindfulness allowed the client to know practices that gradually changed the concept about themselves and about the body itself. The aesthetically valued object passed to the body of pleasure and fully functional deserving of care. This new concept of the body allowed a broad and improved self-esteem.
The cultures of acceptance and self-compassion allowed the acceptance of one’s own body nature in transition and created conditions for a more harmonious physical experience. On the other hand, self-demand and clinical perfectionism typical of food conditions, as presented in Fairburn (2008), gave space for the permissiveness of difference and beauty of individuality.
The difficulties presented with satisfaction with body image did not prevent the patient from practicing body scan, mindfulness in motion and mindfulness applied to feeding (with visualization of the new gastric space). All strategies used were duly highlighted as maintainers of the improvements obtained. The practice of self-compassion proved to be an important preparation for body visualization practices.
Self-care and self-compassion enabled better choice of food and search for healthy and sustainable physical exercises. Foods previously perceived as non-palatable and non-rewarding began to be interpreted as maintainers of health, well-being and physical disposition. Non-pleasant physical exercises could be adapted with intensity and frequency recommended for weight, height and body composition of the client.
There was a healthier positioning in social relationships with less emotional reactivity and less personalized perception of reality. The reduction of the need to please peers, less need for social approval and validation allowed the advancement of personal goals.
Weight loss promoted a sense of self-respect and self-care due to the positive and evident results related to the client’s effort. The reconstruction of body image, although difficult, was progressive and positive.
In the prevention of weight recurrence and maintenance of results, monthly sessions were maintained as interventions in the relapse prevention model.
6. DISCUSSION
The study has limitations due to the time spent. The period described in the literature for weight recurrence, according to Magro et al (2008), is in the interval between 2 and 5 years postoperatively.
In this sense it is necessary to test the short interventions in Mindfulness in a significant sample, prospectively and for a longer period of time. The development of practices with clients already in the process of weight recurrence is an alternative pathway, as well as randomized double-blind studies. Future research in this sense may prove the scientificity of the method.
Metabolic factors relevant to the surgical technique are determinants of weight loss and were not taken into account in the present study. Also the anatomical (poorly performed surgery) or hormonal (return of ghrelin level) actions responsible for weight recurrence were not examined. The focus remained on the psychological aspects of body image described in the study.
The case attended had the collaboration of the client and the good therapeutic bond. The acceptance of the proposed practices as well as the fulfillment of the requested tasks allowed the progress of the process.
Although the family did not present good acceptance of obesity as a disease, it contributed to the multidisciplinary follow-up of the client and did not negatively interfere in the surgical results.
7. FINAL CONSIDERATIONS
The present case study had as a guide question to ascertain whether small mindfulness interventions would have the ability to perform body image improvement and recognition of body distortions in patients undergoing bariatric surgeries, with the objective of preventing weight recurrence in bariatric patients. Through the course of 12 sessions it was possible to demonstrate that small interventions in Mindfulness are applicable to cognitive behavioral therapy in the prevention of weight recurrence in postoperative patients in bariatric and metabolic surgery. A decrease in the discrepancy between the internal subjective perception of the body (interoception) and body image (exteroception) was observed, with positive experience of the body outside the aesthetic requirements, greater identity with the body shape achieved, exit from the perfectionist pattern and evaluation improvement of body shape and size.
The small practices in Mindfulness contributed to the prevention of weight recurrence, especially through the insertion of the interoceptive practice of the imagination of the reduced postoperative stomach. This practice was of great importance for the adaptation and improvement of body perception from the inside out.
Considering the limitations that a case report may incur, the study showed applicability to the population to which it intended to attend and allowed benefits regarding the maintenance of surgical results in bariatric surgery.
REFERENCES
ALBERTS, H. J. E. M.; THEWISSEN, R.; RAES, L. Dealing with problematic eating behaviour. The effects of a mindfulness-based intervention on eating behaviour, food cravings, dichotomous thinking and body image concern. Appetite. v. 58, 3 ed, S.l.: Elsevier, 2012, p. 847-851. Disponível em: https://www.sciencedirect.com/science/ article/abs/pii/S0195666312000104. Acesso em: 14/05/2020.
ALBERTSON, Ellen R.; NEFF, Kristin D.; DILL-SHACKLEFORD, Karen E. Self-Compassion and Body Dissatisfaction in Women: A Randomized Controlled Trial of a Brief Meditation Intervention. Mindfulness. S.l.: Springer Nature, v. 6, 2015, p. 444–454. Disponível em: https://doi.org/10.1007/s12671-014-0277-3. Acesso em: 23/03/2020.
BACALTCHUK, J; HAY, P. J. Terapia Cognitivo-Comportamental dos Transtornos Alimentares. In: Knapp, P. (org). Terapia Cognitivo-Comportamental na Prática Psiquiátrica. Porto Alegre: Artmed, 2004, p. 299-310.
BADOUD, Deborah e TSAKIRIS, Emmanouil. From the body’s viscera to the body’s image: Is there a link between interoception and body image concerns? In: Neuroscience and Biobehavioral Reviews. v. 77, 2017, p. 237–246. Disponível em: https://doi.org/10.1016/j.neubiorev.2017.03.017. Acesso em: 30/07/2020.
BUSETTO L.; BUONGIORNO F. e SCHIFF, S. Studies on Body Image Changes After Bariatric Surgery in Adults. In: CUZZOLARO, Massimo; FASSINO, Secondo. (org) Body Image, Eating and Weight. c. 17, S.l.: Springer, 2018, p. 233-245. Disponível em: https://doi.org/10.1007/978-3-319-90817-5_17. Acesso em: 06/12/2020.
BYRNE, Susan M.; COOPER, Zafra; FAIRBURN, Christopher G. Psychological Predictors of Weight Regain in Obesity. Behav. Res. Ther, n. 42, 2014, p.1341–1356. Disponível em: https://doi.org/10.1016/j.neubiorev.2017.03.017. Acesso em: 20/08/2020.
CELLA, Stefania et al. Relationships between self-esteem, interoceptive awareness, impulse regulation, and binge eating path analysis in bariatric surgery candidates. Clinical Neuropsychiatry, v. 16, n. 5-6, 2017, p. 213-220. Disponível em: https:// doi.org/10.1016/j.neubiorev.2017.03.017. Acesso em: 20/12/2020.
COLOM, Francesc; VIETA, Eduard; SCOTT, Jan. Psychoeducation Manual for Bipolar Disorder. Cambridge: Cambridge University Press, 2006.
CHRISTOU, Nicolas; LOOK, Didier; MACLEAN, Lloyd. Weight Gain After Short- and Long-Limb Gastric Bypass in Patients Followed for Longer Than 10 Years. Annals of Surgery, v. 244, n. 5, 2006, p. 734-740. Disponível em: https://doi.org/10.1097/01.sla.0000217592.04061.d5. Acesso em: 11/11/2020.
DA LUZ, Felipe Q. et al. Early Maladaptive Schemas and Cognitive Distortions in Adults with Morbid Obesity: Relationships with Mental Health. Behav. Sci. v.7, fev/ 2017. Disponível em: https://www.researchgate.net/publication/314116001. Acesso em: 17/09/2020.
DIMITRIADIS, Georgios K.; RANDEVA, Manpal S.; MIRAS, Alexander D. Potential Hormone Mechanisms of Bariatric Surgery. Curr Obes Rep. v. 6, 3 ed, 2017, p. 253–265. Disponível em: https://doi.org/10.1007/s13679-017-0276-5. Acesso em: 22/12/2020.
FAIRBURN, Christopher. G. Cognitive behavior therapy and eating disorders. In: WILSON, G T Treatment of Binge Eating Disorder. New York: Guilford Press, 2011, p. 773–78.
FISCHER Dana; MESSNER Matthias; POLLATOS Olga Improvement of Interoceptive Processes after an 8-Week Body Scan Intervention. In: Human Neuroscience, v. 11, 2017, p. 452. Disponível em: https://doi.org/10.3389/fnhum.2017.00452. Acesso em: 20/05/2020.
FREDERICK, David A. et al. Can she be healthy at her weight? Effects of news media frames on antifat attitudes, dieting intentions, and perceived health risks of obesity. Stigma and Health Advance online publication, 2019. Disponível em: https://doi.org/10.1037/sah0000195. Acesso em: 02/09/2020.
FREEMAN, Arthur; WOLF, Rose De. The 10 Dumbest Mistakes Smart People Make And How To Avoid Them. New York: Harper Collins Publishers, 1992
GAO, Xiao et al. My Body Looks Like That Girl’s: Body Mass Index Modulates Brain Activity during Body Image Self-Reflection among Young Women. Journals Plos One. Out/2016. Disponível em: https://doi.org/10.1371/journal.pone.0164450 Acesso em: 12/08/2020.
GELLER, Shulamit et al. Psychological distress among bariatric surgery candidates: The roles of body image and emotional eating. Bariatric Surgery. v. 9, 2 ed. Aug/ 2019. Disponível em: https://doi.org/10.1111/cob.12298. Acesso em: 04/04/2020.
HERBERT, Beate et al. Interoception across modalities: on the relationship between cardiac awareness and the sensitivity for gastric functions. Journals Plos One. Mai/2012. Disponível em: https://doi.org/10.1371/journal.pone.0036646. Acesso em: 12/03/2020.
KABAT-ZINN, Jon. Full catastrophe living: Using the wisdom of your mind to face stress, pain and illness, 15ª ed. New York: Dell Publishing, 2005.
LEAHY, Robert L. Cognitive Therapy Techniques. A Practitioner’s Guide, 2 ed. New York: The Guilford Press, 2017.
MAGRO Daniéla Oliveira et al. Long-term weight regain after gastric bypass: a 5-year prospective study. Obes Surg, v.18, 2008, p. 648-651. Disponível em: https://doi.org/10.1007/s11695-007-9265-1 . Acesso em: 29/10/2020.
PIZATO, Nathalia et al. Effect of Grazing Behavior on Weight Regain Post-Bariatric Surgery: A Systematic Review Nutrients. 2017. Disponível em: https://doi.org/10.3390/nu9121322. Acesso em: 08/12/2020.
PRESTON, Catherine; EHRSSON, Henrik. Illusory Changes in Body Size Modulate Body Satisfaction in a Way That Is Related to Non-Clinical Eating Disorder Psychopathology. Journals Plos One. Jan/2014. Disponível em: https://doi.org/10.1371/journal.pone.0085773. Acesso em: 19/06/2020.
RAMALHO, Sofia Marlene Marques et al. Excessive Skin and Sexual Function: Relationship with Psychological Variables and Weight Regain in Women After Bariatric Surgery. Obes Surg, v. 25, 2014, p. 1149–1154. Disponível em: https://doi.org/10.1007/s11695-014-1514-5. Acesso em: 24/09/2020.
SARWER, David B. et al. Psychosocial Characteristics of Bariatric Surgery Candidates. In: SARWER, David B.; ALLISON, Kelly C. The ASMBS Textbook of Bariatric Surgery. v. 2. New York: Integrated Health, 2014
SARWER, David. B., et al. Psychopathology, disordered eating, and impulsivity as predictors of outcomes of bariatric surgery. Surgery for Obesity and Related Diseases. 4 ed., v. 15, 2019, p. 650-655. Disponível em: https://doi.org/10.1016/j.soard.2019.01.029. Acesso em: 10/11/2020.
SALA, Margarida; VANZHULA, Irina A.; LEVINSON, Cheri A. A longitudinal study on the association between facets of mindfulness and eating disorder symptoms in individuals diagnosed with eating disorders. In: Rev. European Eating Disorders Review, v.7, n.3, mai/2019. Disponível em: https://doi.org/10.1002/erv.2657. Acesso em: 20/07/2020.
Sociedade Brasileira de Cirurgia Bariátrica e Metabólica (SBCBM). Número de cirurgias bariátricas aumentam 46,7%. Boletim da Sociedade Brasileira de Cirurgia Bariátrica e Metabólica, n. 53, 2018. p. 5-7. Disponível em: https://www.sbcbm.org.br/portfolio/boletim-no-53-2018-2. Acesso em: 20/05/2020.
Sociedade Brasileira de Cirurgia Bariátrica e Metabólica (SBCBM). Protocolo clínico de COESAS (comissão das especialidades associadas) da SBCBM (sociedade brasileira de cirurgia bariátrica e metabólica) sobre a assistência psicológica no tratamento cirúrgico da obesidade. 2014.
SEGAL, Zindel V.; WILLIAMS, Mark; TEASDALE, John. Mindfulness Based Cognitive Therapy for Depression, 2º ed. New York: The Guilford Press, 2013.
TYLKA, Tracy L.; WOOD-BARCALOW, Nichole L. What is and what is not positive body image? Conceptual foundations and construct definition Body Image, v. 14, 2015, p.118-129. Disponível em: https://doi.org/10.1016/j.bodyim.2015.04.001. Acesso em: 20/05/2020.
VAITL D. Interoception. Biological psychology, n. 42, 1996. p. 1–27. Disponível em: https://doi.org/10.1016/0301-0511(95)05144-9. Acesso em: 20/09/2020.
VELAPATI, Saketh R. et al. Weight Regain after Bariatric Surgery: Prevalence, Etiology, and Treatment. Journal Current Nutrition Reports. v. 7 n. 4 ed. 2018. Disponível em: https://doi.org/10.1007/s13668-018-0243-0. Acesso em: 20/08/2020.
APPENDIX – FOOTNOTE
2. Departamento de Informática do Sistema Único de Saúde – DATASUS is the IT department of the Unified Health System in Brazil.
3. Registro de Pensamentos Disfuncionais.
[1] Master in Psychology from UTP; Specialist in Analytical Psychology; Specialist in Clinical Psychology; Specialist in Cognitive-Behavioral Therapy; Psychology (Undergraduate, Bachelor’s Degree, Clinic and Licentiate Degree); Artistic Education – Short Degree. ORCID: 0000-0002-7983-7174.
Submitted: November, 2021.
Approved: February, 2022.