NASCIMENTO, Thalita Silva [1] MARCHTEIN, Rachel [2]
NASCIMENTO, Thalita Silva; MARCHTEIN, Rachel. Herbal prescriptions in primary care to health. Multidisciplinary Core scientific journal of knowledge. 01 year. Vol. 09. pp 659-670. October/November 2016. ISSN:2448-0959
Summary
It is remarkable the increasing use of herbal medicine in the present day. The present study of the exploratory type, based on literature search, investigates the importance of herbs by professional decision entered in the public health service. The development of herbal remedies can be treated as an important strategy for the public health service. The proper use of medicinal plants in primary health care represents an option to be offered to the population to try to improve your health and quality and life. The safest place for the individual to obtain this information is in the health unit. It is necessary that the healthcare professional is able to transmit this information. The Ministry of health carries out various actions with other governmental and non-governmental bodies for the elaboration of public policies directed to the insertion of medicinal plants and herbal medicine in the SUS and the development of the sector. Health professionals must be enabled for the prescription of herbal medicines, based on technical and scientific knowledge and ethical principles, so that can spread knowledge and make a safe use of the same, looking this way, fill in a rational way and qualified to the needs of the population seeking care in the SUS. It is possible to realize, therefore, that the decision of phytotherapy by entered in the public health service must occur along with your training.
Key words: phytotherapy, health system, primary care.
1. INTRODUCTION
Phytotherapy is a portmanteau of the words of Greek origin phito (plants) and therapia (treatment). She improves disease States through the use of natural substrates like plants, fresh or dried, or preparations thereof, in order to prevent, alleviate or cure a disease. For this, several parts of the plant are used in different preparations for prophylactic or therapeutic use as: root, bark, flowers or leaves (KALLUF, 2008).
During your evolutionary process, man learned to differentiate the various types of plants and went on to dominate your use both for food and for the relief of ailments and diseases (FERREIRA; Pinto, 2010). The plants and herbs are used as medicines by the human being from the beginning of your story. There are reports that since 5000 BC. treatment with plants was already known (KALLUF, 2008).
Resulted in this process, the use of medicinal herbs for many people. However, it is important to note that several times, this feature is used due to the lack of access to medicine and indiscriminately (MELO et al. 2012).
According to RDC No. 26/14 – ANVISA, "are considered herbal medicines the obtained with unique job of active raw materials plants whose safety and efficacy are based on clinical evidence and are characterized by the constancy of your quality. ”
Just like any medicine the herbal medicines should offer a guarantee of quality, prove their therapeutic effects and ensure safety for the population. This is achieved through etnofarmacológicos surveys, tecnocientíficas documentation in bibliography and/or indexed publications and/or pharmacological and toxicological studies, pre-clinical and clinical. Beyond the control of raw materials, finished product, packaging materials, pharmaceutical formulation and stability studies.
Nowadays the development of herbal remedies can be treated as an important strategy for the public health service. They present themselves as an option to increase the therapeutic resources, preserving biodiversity, rescue lore, promoting environmental education and popular, Agroecology and social development.
Fits then discuss the use of herbal medicine in the basic attention and preparation of these professionals for this practice.
2. MATERIALS AND METHODS
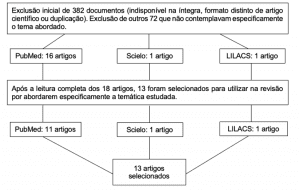
The present study is exploratory type, based on literature search, investigates the importance of herbs by professional decision entered in the public health service. The search of the scientific articles was held in the databases MEDLINE, LILACS, SCIELO. The keywords used were herbal medicine, medicinal plants, SUS, health system, primary care. Were also used in references cited in these articles the Health Ministry manuals and books relevant to the topic. The review was conducted between the months of January and April 2016.
3. RESULTS AND DISCUSSION
3.1. HERBAL MEDICINE AND BASIC CARE
The basic attention is known as the "gateway" in the unified health system (SUS), is the first contact between the user and the network system of health care. The basic attention is based on the principles of universality, accessibility, continuity of care, link, integrality of attention, accountability, humanization, equity and social participation (BRAZIL, 2011a).
Is strategic to solve the health problems that are found in the highest frequency and relevance. Are essential to health care for disease control and prevention.
At the International Conference on Primary Health Care in Alma-Ata in 1978, it was the first time that the World Health Organization recommended that Member countries should identify and enhance traditional health practices within their territories, Recognizing the "use of herbal medicines with prophylactic purpose, remedial and therapeutic" (BRAZIL .2012).
The tenth National Conference on health in 1996 recommended the inclusion of health practices as herbal medicine, acupuncture and homeopathy in the SUS, contemplating the popular practices and alternative therapies. It was also recommended that the city manager of health stimulate pharmaceutical care herbal medicine with extensive public participation in the development of standards for your use (BRAZIL, 2006a).
Today, dozens of municipalities in Brazil, develop programs in the basic attention and herbs in the family health strategy.
It is observed in some municipalities in Brazil increasingly growing interest of health professionals to be trained in this area. The professionals see this practice complement as a possibility to improve your day to day work in public service, expanding the reach of your prescription and innovating in health care (BRAZIL, 2012).
The proper use of medicinal plants in primary health care (PHC) represents one more option to be offered to the population to try to improve your health and quality and life (SILVA et al. 2006). However, it is important to note that this usage should be rational, understanding a proper prescription, a timely availability, acceptable prices, the dispensation under appropriate conditions, consumption in the recommended doses, respecting the intervals pre-defined and in the period of time indicated (BRAZIL, 2001).
To promote the rational use of medicinal plants and herbal remedies in the SUS is necessary to develop strategies of disclosure and information for health professionals, as users. Orient correctly about treatment, dose, dosage and possible interactions reduces misunderstandings and facilitates the attainment of rational use of medicinal plants and herbal remedies (BRAZIL, 2012).
The use of herbal medicine for the public health network in Brazil aims to rescue the traditional culture of the use of medicinal plants by population, prevention of diseases, increase your access, promotion, maintenance and restoration of health, encouraging Thus, the strengthening of the fundamental principles of the SUS (GAUTAM et al. 2013).
Antonio, Tamer and Moretti-Pires (2013) analyzed programs and actions of phytotherapy in APS. The main reasons for the implementation of actions or programmes of phytotherapy on APS found for they illustrate the picture 1 and 2.
Table 1. Goals and motivations for deployment of phytotherapy on APS
| Actions/programs with emphasis on professional prescription of herbal medicines and medicinal plants scientifically standardized | |
| Motivations | Goals |
| Diversify therapeutic options | Dispense herbal medicines handled and processed |
| Public policies | Establish public policies in the area of preservation, research and use of medicinal plants |
| Health education scientific | Guide to use "correct" plants |
| Cost reduction | Offer the population an alternative drug safe, effective and cheap |
Source: (ANTONIO, TAMER, MORETTI-PIRES, 2013) adapted
Table 2. Goals and motivations for deployment of phytotherapy on APS
| Actions/programs for the community with educational, social and environmental perspective | |
| Motivations | Goals |
| Botanical identification | Guide the use of plants to professionals and users |
| Desmedicamentalização | Reduce unnecessary use of psychotropic substances |
| Homemade vegetable gardens to prevent vacant land | Prevent poisonous animals and mosquitoes |
| Solidarity and quality of life | Promote dialogue between different knowledge and solidarity |
| Bond, humanization | Stimulate exchange of experience with team link community |
| Environmental education | Stimulate environmental education |
| Family agriculture | Encourage family farming as a way of improving the quality of life |
| Interculturality | Preserve the brazilian cultural diversity |
Source: (ANTONIO, TAMER, MORETTI-PIRES, 2013).
Even in this study we evaluated the programs and actions of herbal medicine in primary health care. In the literature reviewed there were different forms of work with herbal remedies under the APS services (ANTONIO; TAMER; MORETTI-PIRES, 2013).
Table 3. Ways of working with herbal remedies on APS
| Forms of work | Description | Technical support |
| Pharmacy-alive | Carrying out activities that perform cultivation, collection, processing, storage, handling and dispensing of medicinal plants and herbal medicines handled. | Pharmacist, agronomist, agricultural technical and/or of grass |
| Compounding pharmacy of herbal remedies | Manipulation of the area derived from vegetable raw material processed according to legislation of the national health surveillance agency (ANVISA). | Pharmacist |
| Dispensation of herbal medicines | The cast of herbal medicines is part of the basic component of Pharmaceutical Assistance National ratio of Medicines. | Pharmacist |
| Dispensation of dry plant (vegetable drug) | Refers to activities related to drying and dispensation of dry plant in the form of teas. | Pharmacist |
| Teaching gardens | Areas for the cultivation of plants in natura, botanical identification, preservation of endangered species and studies, teaching about plants. | Agronomist, agricultural technical and/or of grass |
| Community gardens | Areas intended for organic farming, drying craft, Exchange or donation of seedlings of plant species, in the vast majority, without botanical identification, but based on the popular and traditional culture. | Agronomist, agricultural technical and/or of grass |
| Workshops of home remedies | Areas and actions aimed at the preparation and distribution of traditional herbal medicine formulas and seedlings by non-governmental institutions. | With or without the participation of health professionals |
Source: ANTONIO, TAMER, MORETTI-PIRES, 2013, adapted.
Each shape can be supervised or rely on technical support from a qualified professional. The home remedies are familiar, popular and traditional initiatives, based on their own knowledge, so it may or may not occur with the participation of health professionals. Such possibilities allow to occur several ways that include and go beyond the therapeutic character of herbal medicine as a remedy prescribed, however all they need to manage, somehow, at least in public services environment health, safety, effectiveness and quality (ANTONIO, TAMER, MORETTI-PIRES, 2013).
Some of these forms of work cited in illustration present legislation specifies. The Living Pharmacy, for example. The ministerial order n° 886, of 20 April 2010 setting up the Pharmacy Alive within the SUS, and RDC n° 18, of 3 April 2013 offers on the best practices of processing and storage of medicinal plants, preparation and dispensing of magistral and Officinal products of plan medicinal and herbal pharmacies TAS alive under the SUS. The realization of programs like this are an incentive for the correct use of herbal medicines selected by your safety and effectiveness as a replacement for everyday use based solely on plant communities experience (SILVA et al. 2006).
3.2. THE DECISION BY HERBAL MEDICINE
In countries where the main form of medicine is allopathic, still other forms of health care are called complementary or alternatives (KUREBAYASHI; FREITAS; OGUISSO, 2009).
The Brazil has the highest biodiversity in the world, and added to an ethical and cultural heterogeneity has a precious traditional knowledge associated with the use of medicinal plants, thus has a huge potential for the development of herbal medicine ( BRAZIL, 2006b).
Despite the rich diversity of plants in Brazil, around 55000 species, there is reports of investigation of bioactive compounds in only 0.4% of the flora (SILVA; ALBIERO, 2014). Still, most of the medicines available in the world today, have or have had your source in studies developed from the popular culture that make the great brazilian biodiversity a wide field of scientific research (BRAZIL, 2011a).
Some aspects in the choice of this therapeutic support as: improving health care, sustainable use of plant diversity, encouragement of the brazilian family agriculture, employment and income generation, technological and industrial development with social inclusion and regional perspective (BRAZIL, 2006b).
The expansion of the sector of medicinal plants and herbal remedies shown as a strategy to address regional inequalities that exist in our country. It is an opportunity of socioeconomic insertion of populations living in areas with precarious social indicators. Structuring production chains directed to commercial farming and herbal remedies can assist in the reduction of different concentrations of income between regions of the country (BRAZIL, 2006b).
The popular and institutional interest has been growing, but several issues arise from the moment if you want to use a herbal therapy: how and when to prescribe? For who? And that herbal medicines use? These can be some of the questions that arise when defining the herbal medicine as a treatment. To assist the decision of the health professional, Fintelman and Weiss (2010) ranked the herbal medicines in four different therapeutic categories. This framework can serve as a guide to guide clinical decision and elucidate the possible phytotherapeutic treatment options.
Table 4. Therapeutic categories of herbal remedies
| Category 1 | Indications for which the medicinal plants are the therapeutic option of first choice, and for which, as an alternative, there'd be no synthetic medicines, or if they exist, would not be as efficient as the phytotherapic. Examples: toxic hepatitis, benign prostate hyperplasia, among others. |
| Category 2 | Indications for which synthetic medicines can be substituted by herbal medicines. Example: light States of anxiety and/or depression reactive, non-neoplastic ulcerative dyspepsia, urinary infections, nonspecific, among others. |
| Category 3 | Indications in which herbal remedies can be used as adjuncts to a basic therapy. Example: other liver diseases and respiratory tract, among others. |
| Category 4 | Indications in which the use of herbal medicines is not suitable, featuring even medical malpractice, the possibility to delay or prevent a rational therapy with synthetic medicines. Example: primary treatment of cancer. |
Source: FINTELMANN; WEISS, 2010, p. 17, adapted.
This classification is an important guide in clinical decision and can help clarify if there are possibilities, or not to be a phytotherapeutic treatment, be it exclusive or combined.
As you can see, prescribe herbal medicine is not as simple as common sense might suggest. There are several implications in this choice. So there is a conscious choice, professional training that will make that decision.
3.3. TRAINING OF PROFESSIONALS FOR PHYTOTHERAPY
Although phytotherapy be developing more each day in Brazil, the availability of herbal products on the market, from production to marketing and use by the population is still quite worrying, since the training of professionals in this area is not yet satisfactory (CALIXTO, 2000).
Although many studies show that health care with herbal-based products is beneficial for human health, it is necessary that the user has knowledge about your purpose, risk and beneficial. The safest place for the individual to obtain this information is in the health unit (FATIMA et al., 2015).
The problem is that the population search, on many occasions, information out of the environment health unit, on-site marketing of medicinal plants, for example. The concern in such cases is that people who sell these plants, called herbalists, obtain their knowledge of oral tradition without scientific backing. This was demonstrated in a study in the city of Campina Grande, in Paraíba, where few herbalists that associated knowledge acquired with the oral tradition to literature on the subject (FRANCE et al., 2008). This fact confirms the need for training of health professionals on this topic.
Even with the recognition of the professional health councils herbs such as pharmacy, medicine and nutrition, many professionals don't feel safe to approach the subject. Stresses, therefore, the need for spaces for the discussion of the theme, both in the academic environment as in work, in addition to the legal enactment to ensure your offering (AXE; CZERMAINSKI; LEE, 2012).
After observational study with 27 doctors of the family health program (PSF) in the municipality of Canoas (RS), Rosa, and Beria (2011) found that the intended use of herbal medicine was greater among those who had greater knowledge of the subject. This fact shows the importance of the training of professionals and the investment in permanent education program. The professionals interviewed revealed a concern with contemporary scientific criteria of this therapy.
The development of technical material to compose a program including pre-clinical and clinical studies and the validity of use of medicinal plants and/or herbal medicines would be a facilitator for the use of this therapy in the SUS (pink; Chamber; BERIA, 2011).
Some professionals fail to prescribe due to lack of information on the subject. But among those who prescribe there is also a need for capacity-building, since often they associate the use of herbal medicines with allopathic drugs, and unaware that this practice can generate risks. What they often ignore is that several have been described interactions between herbal medicines and drugs chemically defined, some related to the modulation of enzyme activity at the place of performance (SANTOS et al., 2011).
Health professionals who will prescribe herbal medicines should be alert to several factors that interfere in the performance of the active complex obtained through vegetables. Each individual has a genetic aspect can express different activities of bioactive substances present. These bioactive substances can be compromised also due to weather conditions like rainfall, luminosity, soil conditions and other factors. It is essential, therefore, to know the taxonomy of botanical raw material that will be used as herbal medicines may present a high risk of toxicity and side effects (FRANCE et al., 2008).
Fulfilling your institutional role, the Ministry of health carries out various actions with other governmental and non-governmental bodies for the elaboration of public policies directed to the insertion of medicinal plants and herbal medicine in the SUS and the development the industry. The productive chain of medicinal plants and herbal remedies permeates many areas of knowledge, requiring multidisciplinary actions, therefore. The expected results in the field of health are dependent on rules governing the steps and actions of the partners (BRAZIL, 2006a).
Establish mechanisms for the qualification of professionals in the local health system is a responsibility of the City Manager. According to the National Policy of Integrative and complementary Practices (PNPIC) for the SUS, in the section of "medicinal plants and herbal medicine" should be set locally to permanent training and education in medicinal plants and herbal medicine for professionals Act health services. This training will be in three tiers (BRAZIL, 2006c).
Table 5: permanent education levels
| Level 1 | Interdisciplinary basic common to the whole team: contextualizing the PNPIC, contemplating the general care with medicinal plants and herbal remedies. |
| 2 level | Specific to college level health professionals: detailing aspects of the handling, use and prescription of medicinal plants and herbal remedies. |
| Level 3 | Specific to agricultural workers: detailing the aspects related to the productive chain of medicinal plants. |
Source: adapted 2006c.
According to the PNPIC (BRAZIL, 2006c) it is necessary to "encourage the development of educational and informative material to support SUS managers in local project development of permanent training and education". Also to follow the recommendations of the PNPIC the Ministry of health has encouraged the inclusion of disciplines with content targeted to medicinal plants and herbal medicine in undergraduate and graduate courses, involved in the area.
Second Michiles (2004) there is a need for a greater commitment of managers to comply with the official guidance on the topic of herbal medicine. The author also highlights that most managers don't consider that actions in support of herbal medicine programs can collaborate for technological development and economic independence of our country in the field of medicines.
4 CONCLUSIONS
The knowledge of herbal medicine is needed as additional practice in the care of individuals in order to guide them on the proper way of identification, preparation and use of plants, making them about the rational use of the same. The use of herbal medicine is recognized as a practice that can assist health professionals in your professional conduct.
The practice of herbal medicine in SUS allows diversify therapeutic options leading to a reduction of medicalization, creates an environment of health education, AIDS in reducing costs, generates solidarity and quality of life, encourages the exchange of experiences establishing links between the community and the professionals, promotes environmental education, encourages the family farming as a way of improving the quality of life and preserving cultural diversity brazilian.
Popular and institutional interests come growing to strengthen phytotherapy in SUS, since from the early 1980 several regulatory instruments as resolutions, ordinances and reports were drawn up.
Although the brazilian flora is of an immense wealth and great use of plants by the population, there is a consensus on the lack of scientific studies on the subject. It is necessary to stimulate the awareness of the importance of the completion of these studies, considering the value of both individual and social results.
Health professionals must be enabled for the prescription of herbal medicines, based on technical and scientific knowledge and ethical principles, so that can spread knowledge and make a safe use of the same, looking this way, fill in a rational way and qualified to the needs of the population seeking care in the SUS.
Currently the growing training in universities and research centers, makes possible the development of Brazilian medicinal plants for use in public health programs. However, there is a need for greater integration between research institutions and industry.
It is possible to realize, therefore, that the decision of phytotherapy by entered in the public health service must occur along with your training.
REFERENCES
-ANTONIO, Gisele Damian; TAMER, Charles Dalcanale; MORETTI-PIRES, Rodrigo Otávio. Contributions of medicinal plants for the care and health promotion in primary care. -Interface communication, health, education, Botucatu, v. 17, no. 46, p. 615-633, jul/set 2013.
-BRAZIL. Ministry of health. Phytotherapy in the SUS and the herbal research program of Medicines. Brasília: Ministry of health, 2006. Available in: <http: bvsms.saude.gov.br/bvs/publicacoes/fitoterapia_no_sus.pdf="">.</http:> Accessed on 9 Feb. 2016.
– _______. Ministry of health. The national health surveillance agency. Herbal form of Brazilian Pharmacopoeia. Brasília: Ministry of health, 2011.
– ______. Ministry of health. Secretary of Health policies. Department of Health policy formulation. National Medicines policy. Brasília: Ministry of health, 2001. Available in: <http: bvsms.saude.gov.br/bvs/publicacoes/politica_medicamentos.pdf="">.</http:> Accessed on 10 Feb. 2016.
– _______. Ministry of health. National policy of medicinal plants and herbal remedies. Brasília: Ministry of health, 2006.
– _______. Ministry of health. Secretariat for health care. Department of basic attention. National policy of Integrative and complementary Practices in SUS: Attitude to expand access. Brasília: Ministry of health, 2006. Available in: <http: bvsms.saude.gov.br/bvs/publicacoes/fitoterapia_no_sus.pdf="">.</http:> Accessed on 9 Feb. 2016.
– _______. Ministry of health. Ordinance No. 886, 20 April 2010. The Living Pharmacy within the unified health system (SUS). [Diário Oficial da União], Brasilia, DF, 22 April 2010. Available in: <http: bvsms.saude.gov.br/bvs/saudelegis/gm/2010/prt0886_20_04_2010.html="">.</http:> Accessed on 17 Feb. 2016.
– _______. Ministry of health. Ministerial order No. 2488, of 21 October 2011. Approves the National Policy of primary health care by establishing the review of guidelines and standards for the Organization of basic attention to the family health Strategy (FHS) and the community health Agents program (PACS). [Diário Oficial da União], Brasilia, DF, 24 October 2011. Available in: <http: bvsms.saude.gov.br/bvs/saudelegis/gm/2011/prt2488_21_10_2011.html="">.</http:> Accessed on 17 Feb. 2016.
– _______. Ministry of health. Secretariat for health care. Department of basic attention. Schedules of basic attention. Integrative and complementary practices: medicinal plants and herbal medicine in the basic attention. Brasília: Ministry of health, 2012.
– _______. Ministry of health. The national health surveillance agency. Resolution RDC 18 of 13 April 2013. Offers on the best practices of processing and storage of medicinal plants, preparation and dispensing of magistral and Officinal products of medicinal plants and herbal medicines in pharmacies alive within the unified health system (SUS). [Diário Oficial da União], Brasilia, DF, 14 April 2013. Available in: <http: bvsms.saude.gov.br/bvs/saudelegis/anvisa/2013/rdc0018_03_04_2013.html="">.</http:> Accessed on 26 Feb. 2016.
– _______. Ministry of health. The national health surveillance agency. Resolution RDC 26 of May 13 of 2014. Rules on the registration of herbal medicines, and the registration and notification of traditional herbal products. [Diário Oficial da União], Brasilia, DF, 14 may 2014. Available in:
<https: www.diariodasleis.com.br/busca/exibelink.php?numlink="227191">.</https:> Accessed on 26 Feb. 2016.
-CALIXTO, J.B. Efficacy, safety, quality control, marketing and regulatory guidelines for herbal medicines (phytotherapeutic agents). Brazilian Journal of Medical an Biological Research, v. 33, n. 2, p. 179-189, 2000.
-FÁTIMA, Christiane; GENTLEMAN, Claudia Angelica Nunes; MOLIN, Gislaine Tisott Dal; CAVINATTO, Aline Wiliens; SCHIAVO, Morgana; SAMUELS, Karin Hepp; OLIVEIRA, Karla Renata. Use of medicinal plants by users of the public health service of the city of Ijuí/RS. Brazilian magazine of family and community medicine, Rio de Janeiro, v. 10, n. 36, p. 1-13, 2015.
-FISHER, Vitor F.; Pinto, Angelo C. Phytotherapy in today's world. New chemistry, vol. 33, n° 9, pp. 1829-1829, 2010.
-FINTELMANN, Volker; WEISS, Rudolf f. Manual of herbalism. Rio de Janeiro: Guanabara Koogan, 2010.
-FRANCE, Le Hong Satyr Xavier; Souza, Jehovah Adams; BAPTISTA, Rosilene Santos; BASSETT, Virginia Rossana de Sousa. Folk medicine: benefits and harms of medicinal plants. Brazilian Journal of nursing, v. 61, no. 2, p. 201-208, 2008.
-GONÇALVES, Maria Tavares Dion et al. Health policies for phytotherapy in Brazil. Revista Cubana de Plantas Medicinales, Havana, v. 18, n. 4, p. 632-637, 2013.
-KALUFF, Steph. Functional herbal medicine: the active principles to the prescription of herbal medicines. São Paulo: Editora, 2008 VP.
-KUREBAYASHI, Riza Fumiko Sato; FREITAS, Genival Fernandes; OGUISSO, Taka. Diseases treated by acupuncture and treatable according to perception of nurses. Journal of school of nursing of the University of São Paulo, São Paulo, v. 43, n. 4, p. 930-936, 10.2009.
-AXE, Dani Lamb; CZERMAINSKI, Silvia Beatriz Costa; LEE, Edyane Cardenas. Perceptions of coordinators of health units on phytotherapy and other integrative and complementary practices. In Health Debate. Rio de Janeiro, v. 36, n. 95, p. 615-623,/dez.. 2012.
-MELO, Denise Barrie et al. Herbal medicine, why not? Brazilian magazine of family and community medicine, Florianópolis, v. 7, Jun 2012.
-MICHILES, Elizabeth. Situational diagnosis of the herbal medicine services in the State of Rio de Janeiro. Brazilian Journal of Pharmacognosy, Curitiba, v. 14, Suppl. 1, p. 16-19, 2004.
-SILVA, Alzira Denski of Durga; ALBIERO, Adriana Lenita Meyer. Herbal medicine programs in primary health care: there are successful experiences? Brazilian Journal of Pharmacy, Rio de Janeiro, v. 3, p. 889-908, 2014.
-SILVA, Maria Isabel g. et al. Use of herbal remedies in the basic health care units of the family in the city of Maracanaú (EC). Brazilian Journal of Pharmacology, São Paulo, v. 16, n. 4, p. 455-462, 2006.
-SANTOS, R.L.; GUIMARÃES, G.P.; NOBLE, M.S.C.; PORTELA, A.S. analysis on phytotherapy as integrative practice in the health system. Brazilian Journal of medicinal plants. Botucatu, v. 13, n. 4, p. 486-491.2011.
Rose, Caroline; CAMERA, Sheila Gonçalves; BERIA, Jorge Umberto. Representations and intended use of herbal medicine in the basic attention to health. Science and public health, v. 16, n. 1, p. 311-318, 2011.
[1] Nutritionist specializing in Personal Dietitian in Clinic, sports and herbal medicine "by UBM.
[2] Nutritionist, Coordinator of Nutrition of UBM