ORIGINAL ARTICLE
JÚNIOR, Wilson Pereira da Costa [1], SILVA, Tammyse Araújo da [2]
JÚNIOR, Wilson Pereira da Costa. SILVA, Tammyse Araújo da. Diabetes Mellitus: Main characteristics and perspectives for civil aviation. Revista Científica Multidisciplinar Núcleo do Conhecimento. Year 05, Ed. 08, Vol. 05, pp. 146-164. August 2020. ISSN: 2448-0959, Access link: https://www.nucleodoconhecimento.com.br/science-aeronautics/civil-aviation
SUMMARY
The present article has as scope to discuss diabetes mellitus, a disease relevant and of global reach that in many cases uses insulin as a treatment, or as a kind of compensation, considering that some organisms cannot produce this substance. When this disease affects an airplane pilot or a candidate for this profession, there are restrictions on the issuance of training, due to insulin dependence, and this fact directly reflects on the reality of the aeronaut. The diagnosis of diabetes in pilots led to the discussion about the limits to practice the profession when routineuse of insulinics. Therefore, through a qualitative documentary and bibliographic methodology, the objective was the research to verify the current scenario regarding the decisions on the national and international protocols adopted regarding the disease. At the same time, its reflexes were observed in the professional activity of the aviator. Thus, it was found that insulin, hypoglycemia, glucose and other biological conditions related to diabetes are important and influencing aspects in the health of individuals who have this disease. Therefore, in Brazil, people who lack insulin are considered unfit to be airplane pilots, although diabetics who do not use this treatment, there is the possibility of having their certificates. It has also been found that in the United States, at the forefront of what the world’s future on the subject may be, pilots who use insulin are considered fit, provided they follow a strict protocol of care and preventions. From research conducted by scholars in Europe, it has been found that the use of insulin analogues can control hypoglycemia and that autoimmune diabetic pilots will perform their function if they monitor and follow strict guidelines. It is concluded that, with the study that Brazilians with type 1 diabetes, cannot practice the profession of airplane pilot and that today, there is no horizon for change, since the Brazilian Civil Aviation Regulation (RBAC) 67, which deals with this issue, was updated and amended in 2020. On the other hand, discussions do not cease, and in international scenarios the prospects are more promising.
Keywords: Diabetes Mellitus, aviation perspectives, flight safety, human factor in aviation, airline pilots with diabetes mellitus.
INTRODUCTION
Diabetes mellitus is a disease that affects a significant part of the world and Brazilian population. This disease is related to glucose metabolism, caused from the absence of insulin in the body, or simply by the malabsorption of this hormone in the human body. Diabetes is unfolded in three types, such as 1, 2 and gestational. The symptoms of the disease are several and each organism reacts differently. Its reflexes are severe to physical health, to the point of affecting even the social life of the individual. Thus, early diagnosis is essential with a view to a routine care routine.
It is a disease that affects several social segments. In some cases, it is possible that insulin dependence reduces participation in the world of work and this extends to the activity of an airplane pilot. Apparently, there are indications that aeronaut, when affected with diabetes that lack insulin, is considered unfit for professional practice.
Considering the above, and aiming to analyze the discussions that are in evidence on the subject, the purpose of this research is to examine, in the national and international scenario, the most current questions regarding the diabetic pilot, in addition to the probable impairment of his career, and in parallel, identify if there is a possibility of reversing the apparent condition of ineptitude.
The study is justified because in some cases, the permanent use of insulin can enable the patient to have a better quality of life, so that it does not limit his professional activities, even if the pilot still depends on constant monitoring.
To carry out this research, we chose to use a methodology of a basic nature, with descriptive objectives, performing a qualitative approach of bibliographic and documentary procedures. Thus, the structure of the study is consistent with the adopted method, where it was divided into two sections. The first will demonstrate the main characteristics of diabetes mellitus and will present an overview of the disease, its treatment, in addition to describing some recommendations. It will then seek to examine diabetes from the perspective of civil aviation.
It is expected, with this study, to find evidence that allows the pilot to exercise his profession, even if he/she has diabetes and lacks insulin, allowing the aviator to practice his profession, without endangering the safety of the flight.
1. CONCEPT AND TYPES OF DIABETES MELLITUS
The World Health Organization – WHO[3] (2019) defines the term diabetes as a group of metabolic disorders characterized and identified by the presence of hyperglycemia. This disease is associated with dysfunctions and insufficiency of various organs, such as the brain, heart, blood vessels, eyes, kidneys, among other organs. In the end, it results in the destruction of beta cells of the pancreas, and these cells are responsible for the production of insulin, a hormone that is totally influential in the life of an individual with this disease.
It is understood that diabetes, over the years, has become part of the reality of many individuals from various countries, even after carrying out several scientific studies aimed at a better coverage of the types of the disease. Thus, it is observed that caution and early care are in fact a way for several people to maintain primary care with regard to diabetes mellitus and its prevention.
It is worth mentioning that the Portuguese Society of Diabetology – SPD (2020) considers that diabetes mellitus has become the focus of many international studies in relation to its diagnosis and classification. Therefore, the focus of this research is the mellitus disease, defined by the SPD as a metabolic disorder of multiple etiology, characterized by a chronic hyperglycemia with disorders in metabolism, resulting from deficiencies in the secretion or action of insulin that in the long term leads to dysfunction and failure of various organs and, in the absence of appropriate treatment also leads to death.
Moreover, the WHO (2019) understands that it is a disease that affects the world population widely, which increases every year, and that its effects go beyond the individual, affecting family and societies. The International Diabetes Federation IDF[4] (2019) presents the estimated number of adults with diabetes in 2019, as shown in Figure 1:
Figure 1 – Estimated total number of adults between 20 and 79 years of age with diabetes in 2019:
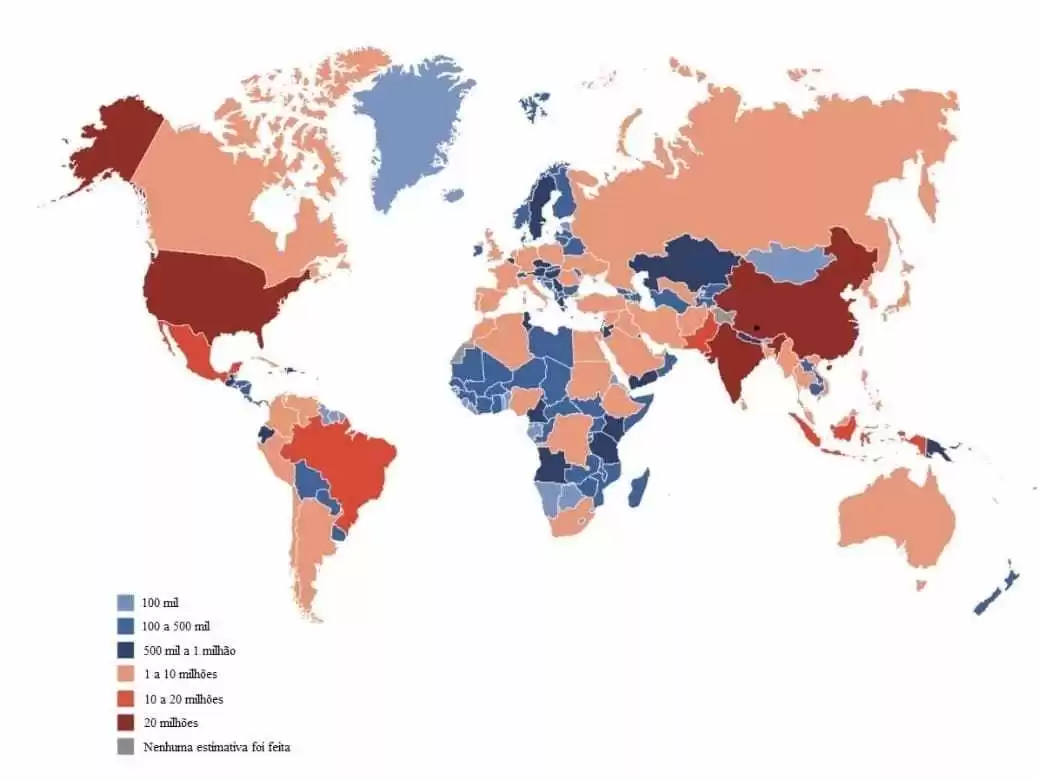
The International Diabetes Federation (2019), as shown in Figure 1, estimates that 463 million adults aged 20 to 79 years worldwide (about 9.3% of all adults in this age group) have diabetes. In addition, it projects the estimated total number of adults aged 20 to 79 years and 79.4% living in low- and middle-income countries.
Based on these 2019 estimates, the IDF also projects that, regardless of type, by 2030 there will be 578.4 million people living with diabetes and that by 2045, this number will increase to 700.2 million. Table 1 shows this estimate:
Table 1 – Estimated total number of people (20 to 79 years) with diabetes in 2019, 2030 and 2045
| 2019 | 2030 | 2045 | |
| Total population of the world | 7.7 billion | 8.6 billion | 9.5 billion |
| Adult population (20-79 years) | 5.0 billion | 5.7 billion | 6.4 billion |
| Diabetics (20-79 years) | |||
| Global Prevalence | 9,30% | 10,20% | 10,90% |
| Number of people with diabetes | 463.0 million | 578.4 million | 700.2 million |
| Number of deaths from diabetes | 4.2 million | ||
| Total Health Spending for Diabetes | $760.3 billion | $824.7 billion | $845.0 billion |
| Hyperglycemia in pregnancy | |||
| Proportion of affected live births | 15,80% | 14,00% | 13,30% |
| Number of live births affected | 20.4 million | 18.3 million | 18.0 million |
| Decreased glucose tolerance (20-79 years) | |||
| Global Prevalence | 7,50% | 8,00% | 8.6 million |
| Number of people with glucose tolerance deficiency | 373.9 million | 453.8 million | 548.4 million |
| Type 1 diabetes (0 to 19 years) | |||
| Number of children and adolescents with type 1 diabetes | 1.110.100 | ||
| Number of newly diagnosed cases each year | 128.900 |
Source: Adapted from IDF (2019).
According to the American Diabetes Association[5] – ADA (2019) it is important to classify the type of diabetes in order to determine the appropriate treatment, although some individuals cannot be clearly classified as to the type of diabetes at the time of diagnosis.
The authors Balda and Pacheco-Silva (1999) report that the main categories of diabetes are type 1, type 2 and gestational. Type 1 is the leading cause of diabetes in childhood and lacks uninterrupted insulin treatment, type 2 is responsible for the vast majority of diabetes worldwide (about 90%), while gestational, increases the risk of complications during pregnancy and at birth, both for the mother and for the baby.
The Brazilian Society of Diabetes – SBD (2019) considers that type 1 diabetes, also known as insulin-dependent diabetes, childhood diabetes and immunomediated diabetes, develops in children, adolescents or young adults, and may also appear in adults and the elderly, and may be hereditary.
For the International Diabetes Federation (2019) type 1 is the most aggressive, as the person produces antibodies that act against the insulin-producing cells of the pancreas (β cells), resulting in little, or no insulin production, thus lacking daily injections to maintain a glucose level in the appropriate range.
In this sense, the research of the authors Balda and Pacheco-Silva (1999) demonstrated a sudden inability of the pancreas to produce insulin because of complete cell destruction. This destruction is caused by the immune system itself of the person with diabetes, which normally protects the body from infections and other external aggressions and sometimes destroys parts of the body itself. That’s why type 1 diabetes is a disease said to be autoimmune.
According to the Ministry of Health (2019), patients with type 1 diabetes require daily insulin injections as a treatment to prevent ketoacidosis, coma status, micro and macrovascular events and even death.
For Balda and Pacheco-Silva (1999), people with type 1 diabetes are generally thinner because the body compensates for the lack of fuel by breaking fat reserves. Individuals with normal weight are quite intestable, and metabolic control of the disease is difficult, thus diabetic ketoacidosis may occur. Diabetic ketoacidosis occurs in people with type 1 diabetes, but may also occur in people with type 2.
In this sense, Soares (2014) explains that diabetic ketoacidosis is a medical emergency, and occurs when blood sugar levels are high, as well as the increase in the amount of ketonas in the blood. Keons are acidic substances that unbalance the pH of the blood and cause an imbalance in blood composition that can lead to coma and even death if left untreated.
To avoid extreme cases, it is necessary to make a diagnosis, and that it is more uniform, especially in diabetes mellitus, as clarified by the SPD (2020), but for this, it is necessary to understand the symptoms.
The International Diabetes Federation (2019) describes that the most common symptoms include over-home (polydipsia), frequent urination (polyuria), blurred vision, weight loss, fatigue and lack of energy, however, some of these factors may not be symptomatic, which leads to late diagnosis.
The treatment of people with diabetes mellitus has five components: diabetes education, insulin therapy, glycemic self-monitoring, nutritional guidance and monitored practice of physical exercise (AMERICAN DIABETES ASSOCIATION, 2019; MINISTÉRIO DA SAÚDE, 2019).
The other type of diabetes, the 2, responsible for about 90% to 95% of diabetes cases, is considered a global health problem. The problem evolves with the consumption of processed foods, sugary drinks, obesity and reduced physical activities. It is common in adults, but has shown an increasing number among children and adolescents, and most people with type 2 diabetes are overweight, or even obese, which causes worsening insulin resistance, according to WHO (2019).
According to author Dib (2006), most people with type 2 diabetes are resistant to insulin. This resistance is due to the decrease in the action of insulin in muscles and adipose tissue. Over time and with the increase of this resistance, the disease may evolve and the patient presents difficulty in insulin secretion due to the exhaustion of the secretory capacity of the cells.
The Brazilian Society of Endocrinology and Metabology – SBEM (2007), explains that this type is called non-insulin-dependent diabetes or adult diabetes that arises from relative insulin deficiency and obesity.
The Global Diabetes Community[6] (2019) adds that in these cases, the pancreas secretes insulin normally, but there are leftoverinsulin and glucose in the blood and low-glucose cells. Thus, the pancreas releases a lot of insulin causing the cells to deteriorate, and the destroyed cells have no insulin production, and consequently the individual now has the need to take insulin and medications to increase sensitivity to this hormone.
Studies by authors Reis e Velho (2002) warn that type 2 diabetes mellitus (DM2) results from defects in insulin secretion and action, and the pathogenesis of both mechanisms is related to genetic and environmental factors. Its incidence has been increasing in several populations and thus becoming one of the most prevalent diseases in the world. The fact is that diabetes is associated with increased mortality and the high risk of developing complications, micro and macro vascular, as well as neuropathies, which may result in blindness, renal failure and even amputations of limbs.
Type 2 diabetes is caused by reduced sensitivity of target tissues to the effect of insulin. In order to overcome this resistance and prevent the accumulation of glucose in the blood, there must be an increase in the amount of insulin secreted. Although it is not known what causes this type of diabetes, it is considered that the hereditary factor has a much greater importance than in type 1. There is also a connection between obesity and DM2, although obesity does not necessarily lead to diabetes (RUIZ; PRADO, 2018).
According to SBD (2019), anyone may have type 2 diabetes, however, there are cases where the risk may be higher, such as in people who consume excessive alcohol, have hypertension, high triglycerides, sedentary lifestyle, low HDL cholesterol levels, previous gestational diabetes, prediabetes, obesity and overweight, who are over 45 years old, including the factor that is most common, family history of type 2 diabetes. Table 2 lists the main risk factors.
Table 2 – Risk factors for developing diabetes
| N. | Risk factors |
| 1 | High pressure |
| 2 | Diagnosis of prediabetes |
| 3 | High cholesterol or change in the rate of triglycerides in the blood |
| 4 | Overweight, especially if fat is concentrated |
| 5 | Close relatives with diabetes |
| 6 | Use of glucocorticoideclass medications |
| 7 | Sleep apnea |
| 8 | Schizophrenia, depression, bipolar disorder |
| 9 | Polycystic ovary syndrome |
| 10 | Gestational diabetes |
| 11 | Woman who gave birth to child over 4 kg |
| 12 | Chronic or chronic diseases |
Source: Adapted from the Ministry of Health (2019).
As the Ministry of Health (2019) warns people with type 2 diabetes, as well as type 1 carriers, are asymptomatic at first, and may have the disease for years without realizing it. The first symptoms of type 2 diabetes are frequent infections, such as skin and urinary infections, and the patient may also present constant ly, hunger outside the normal, willingness to urinate several times a day, tingling in the feet and hands, vision problems such as difficulty seeing, blurred vision, or exaggerated increase in degree, and finally, wounds that take time to heal.
As evidenced earlier, an important detail regarding diabetes is what concerns healing, the difficulty of regeneration of a bruise occurs due to cardiovascular problems, which cause a blockage of blood circulation in the veins, and the excess glucose in the bloodstream, which directly harms the immune system. In this way, cases such as amputation in people with diabetes are extremely common.
The Ministry of Health (2019) emphasizes the importance of performing physical activities in order to maintain a good blood flow, to improve the healing process, and that this can be done through measures that lower cholesterol and high blood pressure levels.
In addition to the two types of diabetes mentioned above, there is also gestational diabetes. The risks provided by this type of diabetes are numerous, which puts the life of the pregnant woman and the fetus at risk.
The third type of diabetes, gestational, as explained by SBEM (2007) occurs when the high blood glucose rate (hyperglycemia) is diagnosed in pregnancy, and complications may occur during pregnancy and even after delivery, both for the woman and for the baby.
The author Zajdenverg (2019) understands that, due to the hormonal change that every pregnant woman suffers during pregnancy, the body produces a greater amount of insulin to transport glucose from food ingested to cells. However, other hormones that the placenta releases, hinder this process and force the pancreas to produce more insulin, working harder and maintaining levels of the normal substance.
Despite this, this work is not always enough, and blood sugar levels rise more than normal, turning into gestational diabetes. The baby receives more glucose through the placenta, the pancreas ends up overloading, glucose is not transformed into energy, and what remains of sugar ends up turning into fat, increasing the child’s weight dramatically. It is important to emphasize that gestational diabetes generates the risk of premature delivery (ZAIDENVERG, 2019).
According to Zajdenverg (2019), some symptoms of gestational diabetes are similar to those of type 1 and 2, such as frequent tiredness, constant sea and a lot of willingness to urinate. Risks are diabetes in previous pregnancies, family history of diabetes, twin pregnancy, overweight, obesity, polycystic ovary syndrome, high triglycerides, high cholesterol, out-of-normal weight gain in pregnancy, high blood pressure, and older pregnancy. Tests for the diagnosis of the disease are done in prenatal care, checking the rate of triglycerides, fasting glycemia and cholesterol. Ultrasound examinations are also performed and, in the twenty-fourth week of pregnancy, an oral glucose tolerance test (glycemic curve) is requested. Gestational diabetes is confirmed if the diagnosis is equal to or greater than 95 mg/dl.
Usually gestational diabetes resolves soon after delivery, but in some cases ends up returning years later. Therefore, preventive methods are important, such as a balanced diet and exercise frequently (SOCIEDADE BRASILEIRA DE ENDOCRINOLOGIA E METABOLOGIA, 2007).
As seen, the three types of diabetes generate consequences that sometimes develop silently and that physical exercise and food care are the basis of prevention. Thus, balanced diets are essential to reduce the level of blood glucose (MINISTÉRIO DA SAÚDE, 2019).
From Haber’s point of view (2001) glucose is regulated by the pancreas, by joint action of glucagon, and mainly insulin. Insulin is produced by beta cells of the pancreas, and is responsible for decreasing blood glucose levels, and so it is of utmost importance to people with diabetes, especially people with type 1 diabetes, facilitating the absorption of glucose by skeletal muscle cells, adipose tissue and liver. Glucagon is produced by alpha cells of the pancreas and performs process contrary to insulin, thus increasing blood glucose levels by stimulating glycogen breakdown.
The SBD (2017) explains that if the person does not follow the proposed diet, exaggerate medication, skip meals, increase the amount of exercise without guidance or adjustments in eating and have the consumption of alcoholic beverages can often occur hypoglycemia.
According to the SBD (2017), the symptoms of hypoglycaemia are: Hunger and nausea, drowsiness, blurred vision, tingling or numbness in the lips and tongue, headache, weakness, fatigue, sadness or anger, tremiling, nervousness, anxiety, sweating and chills, mental confusion, delusions, aquicardia, dizziness or vertigo, irritability and impatience, lack of motor coordination, nightmares, crying during sleep, convulsions and unconsciousness.
According to author Pimazoni Netto (2018), diabete is a disease that is not only treated with medicines, but with a general change in lifestyle. The person should totally change his/her routine to stay healthy, practicing physical exercises daily and especially changing his/her diet. One should maintain a healthy diet, feeding on small meals 3 in 3 hours.
Therefore, it can be understood that meals performed throughout the day should be based on foods rich in essential vitamins, avoiding excessive consumption of foods that have high fat content and high sugar content. It is emphasized at this moment, the relevance that breakfast has, since this is the first meal of the day, and thus, it should be manipulated from the intake of healthy foods, and that have nutrients.
According to SBD (2017), many foods should be avoided, such as sugar, trans fats, refined carbohydrates, white flour, saturated fats, dietary foods, processed foods and especially fried foods.
It is scientifically proven that the body responds negatively when diabetes sufferers maintain a diet based on foods rich in fats and starches, which alters the clinical picture, consequently promoting a higher risk to the individual’s health.
Many foods are essential in the diet of those who have diabetes, for example, those that have bagasse are rich in fiber and give greater satiety, while the apple, in addition to satiety, helps regulate the intestine. Cinnamon has properties that aid in glycemic control, regulate blood glucose levels and prevent hyperglycemia, while oats slow stomach emptying and glucose absorption by blood, as well as improving insulin sensitivity.
2. WORK, GUIDELINES AND REQUIREMENTS OF REGULATORY BODIES IN CASES OF DIABETES
As seen, the IDF (2019) pointed to alarming estimates, both in current and projected long-term numbers. This suggests that the disease reaches a high share of society, including in the professional sphere. The National Diabetes Care Association, ANAD (2016) ensures that diabetes generally has no impact on an individual’s work ability and that many employers are unaware of diabetic employees.
For ANAD (2016), U.S. legislation, for example, protects diabetic individuals from discriminatory acts, aiming to classify them as having a disability in the endocrine system, capable of performing their activities.
The ANAD (2016) suggests that the decision to employ a diabetes patient should take into account an appropriate individual assessment and use guidelines and protocols that assess, among other dimensions, the risk to the safety of workers with diabetes.
In this sense, the author Pimazoni Netto (2014) warns that the National Civil Aviation Agency (ANAC) determined, if the medical examination for airline pilots, especially those intended for commercial aviation, finds that the individual has a clinical diagnosis of insulin-dependent diabetes mellitus, he/she will not be able to practice the profession of pilot.
The examination to which the author Pimazoni Netto (2014) refers is the Aeronautical Medical Certificate (CMA) that has different classes due to the type of activity in which the future professional wishes to act, as shown in Table 3 below:
Table 3 – Types of pilot health examination: CMA
| Class | Type of activity |
| First | Airline pilot, commercial pilot and multiple crew pilot. |
| Second | Private pilot with IFR qualification, private pilot, flight attendant, special equipment operator, flight mechanic and free balloon pilot. |
| Third | Air pilot and glider pilot. |
| Fourth | Remote pilot of remotely piloted aircraft |
Source: National Civil Aviation Agency (2016).
The first class CMA exams are the most rigorous, as they are valid, where it turns out that it is 12 months and, in the case of pilots over 60 years of age who operate in public air transport are 6 months.
Second-class ones, the validity of the CMA is 24 and 12 months, the latter being applied to pilots over 60 years. Thus, the Brazilian Civil Aviation Regulation (RBAC) outlines a series of requirements for obtaining the CMA, among them, behavioral, neurological, cardiological, pneumonological, digestive, metabolic, nutritional and endocrine, hematological, nephrological and urological, auditory and others (AGÊNCIA NACIONAL DE AVIAÇÃO CIVIL, 2020).
According to ANAC (2020), among these requirements there are those that characterize the individual as not fit for the activity, and others that consider it the evaluation of the examiner or the regulatory agency.
According to the organization that will be demonstrated, according to Table 1 based on metabolism disorders, it is possible to verify that there are three cases causing inability to practice the profession of airplane pilot, mainly because they suggest that its occurrence affects flight safety and that the other cases will only allow exercise if there is proof of follow-up and control of the disease. What is evident is that diabetics who use insulin are considered unfit. Table 1 will show these cases below:
Table 1 – Metabolic, nutritional and endocrine requirements (CMA first and second class):
| N. | Disorders with regard to cases of diabetes | Cause | |
| Fitness | Disability | ||
| 1 | History or clinical diagnosis of insulin-dependent diabetes mellitus | X | |
| 2 | Diabetes mellitus not treated with insulin provided that it proves that its metabolic state can be satisfactorily controlled only with diet, or diet combined with oral intake of antidiabetic drugs, whose use is compatible with the safe exercise of the assignments of the flight crew member. | X1 | |
| 3 | Be with blood glucose below 50mg/dl or higher than 140mg/dl, confirmed after two repetitions, on different days. | X | |
| 4 | Be with blood glucose between 50 and 69 mg/dl, or between 115 and 139 mg/dl, confirmed after two replications, on different days. | X1 | |
| 5 | Use hypoglycemic agents orally, provided that, after a period of observation of 60 days, a satisfactory control of blood glucose, which should be higher than 69mg/dl and less than 140mg/dl. | X2 | |
| 6 | Patients with reactive hypoglycemia or other hypoglycemia that is difficult to control or out of the possibility of control. | X | |
Source: ANAC (2020).
Legend: X1 – May be considered fit, at the discretion of the examiner or ANAC, provided that it complies with the requirements stipulated by this document and does not affect flight safety, X2 – May be considered fit, at the discretion of the examiner or ANAC, provided that it complies with the requirements stipulated by this document and does not affect flight safety, however, the maximum validity to be granted for the reassessed CMA must be 6 months.
The author Pimazoni Netto (2015), understands that, in practice, there are five interventions that should be followed in relation to pilots with diabetes who initially understand accurate and early diagnosis, through annual evaluations when the pilot has a family history or risk factors for diabetes. Next, they deal with intensive intervention of home blood glucose self-monitoring in order to determine the daily and sequential glycemic profile.
The third includes the definition and continuous reviews of therapeutic approaches. The fourth consists of the permanent evaluation of the pilot’s support to the recommendations received from the health team. Finally, the strict evaluation of glycemic control to verify the efficacy of the treatment being followed. Although this research has not obtained studies that evidence the current scenario of pilots in Brazil affected by diabetes and what are the labor consequences on them, there are reports that suggest discussions about the use of insulin, especially with regard to commercial aviation.
It was verified that even a digital petition was held, in favor of returning to the career, Change.org (2017), with 1,058 signatures, this fact caused many discussions in the SBD (2015), where there are notes that suggest that the insulinic treatment may not be the only parameter that makes the professional activity impossible, and that cases should be evaluated, taking into account the knowledge about the disease by the pilot , its strict adhering to medical recommendations and the effectiveness of its treatment.
In international scenarios, the discussions are at a level of evolution, given the most recent protocols launched by the Federal Aviation Administration (FAA) in November 2019, where they inaugurate for U.S. pilots, the permission for those with Type 1 or 2 diabetes mellitus treated with insulin to obtain the first or second class medical certificate, provided they do not present a risk to flight safety. This document is FAR Part 67.401.
According to the FAA (2019a; 2019b) the pilot to be allowed to fly requires Continuous Glucose Monitoring (CGM) [7] and without CGM. The option without CGM applies only to third-class candidates, however, the option with CGM is required for class 1 and 2 candidates.
According to the FAA (2019a; 2019b), the protocols allow medical certification issued especially for some candidates treated with insulin or for those who considered clinically stable in their treatment regimen for a period of 6 months or more. In addition, everyone must provide medical documentation about their current treatment history, accidents, and medical status.
The protocol establishes that in cases requiring CGM, to consider the certification of first and second class pilots, the aviator must send the data relating to this monitoring and all certification requirements, including those showing the information on diabetes treated with insulin and the blood glucose worksheet (FEDERAL AVIATION ADMINSTRATION, 2019a).
In addition, to apply for the third class certificate, episodes of hypoglycaemia must be non-existent in the last 05 years. It shall also provide copies of all medical records or accidents and incidents, and submit a complete detailed medical report, preferably made available by a professional specialized in the treatment of diabetes (FEDERAL AVIATION ADMINSTRATION, 2019b).
The FAA (2019b) considers that for the guarantee of a safe flight, existing monitoring measures and actions necessary during its operation should be applied to those pilots who do not use the CGM. A log glucometer should be taken during the flight, plus a supply to obtain rapidly absorbable blood and glucose samples in 10g parts for a full planned flight duration.
Some actions should be followed for the operation of the flight, such as, 30 minutes before the flight, the pilot should obtain the concentration of glucose in the blood, and the result should be greater than 100 mg/dl, if applicable, the pilot should ingest appropriate glucose and measure the concentration of glucose 30 minutes later. If you are between 100 and 300 mg/dl you can fly normally, and if you are over 300 mg/dl the flight should be cancelled.
Every 1 hour of flight, and every 30 minutes before landing, the pilot must receive his blood glucose concentration, and if not expected, he/she must take the necessary measures (FEDERAL AVIATION ADMINSTRATION, 2019b).
In the wake of the United States of America, Simons, Stüben and Maher (2011) in a study affiliated with the European Society for Aerospace Medicine (ESAM [8], 2011) consider that it is possible to keep types 1 and 2 of diabetes treated with insulin, since if diabetic pilots in flight status use glucose continuously and monitor blood glucose levels in the pre-flight, there will be no damage to operations. However, it emphasizes the risks of hypoglycemia, which can be reduced with the use of insulin analogs, and that medical certification should be considered on a case-by-case basis.
FINAL CONSIDERATIONS
It is understood that the present study addressed the types of diabetes, its consequences in the human body and found that in both cases, the disease needs monitoring and care, which includes a good diet.
However, when the diagnosis of this disease is discussed in the field of aviation, it is observed that in Brazil, type 2 diabetes does not produce consequences for the aeronaut, however, the pilot, or pilot candidate with type 1 diabetes, is considered unfit for the profession. This is due to the complications that the disease causes.
It is still questionable by many scholars whether insulin use is actually effective, that is, whether treatment with the said hormone effectively aids in the reality of the individual who has been diagnosed with insulin-dependent diabetes mellitus, and whether consequently, that may be or may not be, airplane pilot.
On the other hand, the research found that the international scenario, more precisely the North American scenario, is ahead of Brazil, comparing the scientific studies that have been conducted in recent years, with regard to the pilot, if he can actually practice the profession, if he is a carrier of this disease, and that if the aviation professional maintains a continuous treatment and if he is following a strict and monitored protocol , you can keep up and hold constantly. It was observed that, in Europe, the present case with a similar position is also analyzed.
Thus, it is concluded that reflections on the use of insulin by pilots should envision new horizons in Brazil, since innovative ways of controlling and monitoring the disease are being widely discussed globally. In practical terms, in order to make significant progress on this theme in Brazil, it is suggested that entities such as SBD and SBEM, important figures on the theme of Brazilian civil aviation, develop further research and significant studies that may lead to the repositioning of Brazilian norms, in order to improve the professional reality of numerous aviators who suffer from the reflexes of diabetes mellitus disease.
Therefore, it is understood that, preventing an aviator from performing his profession because he performs a health treatment from the use of insulin, is not correct, really relevant criteria should be analyzed, such as the performance of a safe follow-up, suiting the physical health of the aviation professional and the existing disease with his work reality.
REFERENCES
AGÊNCIA NACIONAL DE AVIAÇÃO CIVIL. CMA – exame médico. 2016. Disponível em: <https://www.anac.gov.br/assuntos/setor-regulado/profissionais-da-aviacao-civil/processo-de-licencas-e-habilitacoes/cma>. Acesso em 25 abr. 2020
. Regulamento brasileiro da aviação civil: RBAC n. 67, Emenda n. 04. Brasília: ANAC, 2020. Disponível em: https://www.anac.gov.br/assuntos/legislacao/legislacao-1/rbha-e-rbac/rbac/rbac-067/@@display-file/arquivo_norma/RBAC67EMD04%20-%20Retificado.pdf. Acesso em: 19 mar. 2020.
AMERICAN DIABETES ASSOCIATION. Classification and diagnosis of diabetes: standards of medical care in diabetes – 2019, Diabetes Care, v. 42, supplement 1, January, p. S13-S28, 2019.
ASSOCIAÇÃO NACIONAL DE ATENÇÃO AO DIABETES. Diabetes e emprego. 2016. Disponível em: <https://www.anad.org.br/diabetes-e-emprego/>. Acesso em: 28 abr. 2020.
BALDA, C. A.; PACHECO-SILVA, A. Aspectos imunológicos do diabetes melito tipo 1. Revista da Associação Médica Brasileira, São Paulo, v. 45, n. 2, p. 175-180, 1999.
DIB, S. A. Resistencia a insulina e síndrome metabólica no diabetes mellitus tipo 1, Arquivos Brasileiros de Endocrinologia & Metabólica. São Paulo, v.50, n. 2, p. 250-263, 2006. Disponível em: <https://www.scielo.br/scielo.php?script=sci_arttext&pid=S0004-27302006000200011>. Acesso em 19 mar. 2020.
FEDERAL AVIATION ADMINSTRATION. Guide for aviation medical examiners: decision considerations disease protocols – diabetes mellitus type I or type II – insulin treated – CGM option. Washington: FAA, 2019a. Disponível em: https://www.faa.gov/about/office_org/headquarters_offices/avs/offices/aam/ame/guide/dec_cons/disease_prot/itdm/. Acesso em: 30 abr. 2020.
. Guide for aviation medical examiners: disease protocols – diabetes mellitus type I and type II – insulin treated – non-CGM – third class option. Washington: FAA, 2019b. Disponível em: https://www.faa.gov/about/office_org/headquarters_offices/avs/offices/aam/ame/guide/dec_cons/disease_prot/diabetes_insulin/. Acesso em: 01 maio 2020.
GHANGE.ORG. ANAC autorize pilotos diabéticos que fazem uso de análogos de insulina a obter CMA. 2017. Disponível em: https://www.change.org/p/anac-ag%C3%AAncia-nacional-de-avia%C3%A7%C3%A3o-civil-anac-autorize-pilotos-diab%C3%A9ticos-que-fazem-uso-de-an%C3%A1logos-de-insulina-a-obter-cma. Acesso em 10 maio 2020.
HABER, E. P. Secreção da insulina: efeito autócrino da insulina e modulação por ácidos graxos. Arquivos Brasileiros de Endocrinologia & Metabólica, São Paulo, v. 45, n. 3, p. 2019-227, junho 2001. Disponível em: <https://www.scielo.br/scielo.php?script=sci_arttext&pid=S0004-27302001000300003>. Acesso em 03 abr. 2020.
INTERNATIONAL DIABETES FEDERAL. IDF Atlas. 9th. Brussels, Belgium: IDF, 2019.
MINISTÉRIO DA SAÚDE. Secretaria de Ciência, Tecnologia e Insumos Estratégicos. Protocolo clínico e diretrizes terapêuticas diabetes mellitus tipo 1: relatório de recomendação. Brasília: CONITEC, 2019.
PIMAZONI NETTO, A. Análogos de insulina e hipoglicemia em pilotos de aeronaves. 2014. Disponível em: <https://www.diabetes.org.br/publico/component/content/article?id=892:a-importancia-ea-flexibilidade-do-tratamento>. Acesso em 05 abr. 2020.
. O uso de insulina por pilotos de aeronaves pode impedir o exercício de sua profissão de voar? 2015. Disponível em: <https://www.diabetes.org.br/publico/artigos-sobre-diabetes/1190-o-uso-da-insulina-por-piloto-de-aeronave-pode-impedir-o-exercicio-de-sua-profissao-de-voar>. Acesso em 5 abr. 2020.
. O uso de insulina por pilotos de aeronaves pode impedir o exercício de sua profissão de voar? 2017. Disponível em: <https://www.diabetes.org.br/publico/conte-sua-historia/1551-monica-supera-dificuldades-de-cegueira-e-lanca-seu-segundo-livro>. >. Acesso em 04 abr. 2020.
. Viva saudável com diabetes. 2018. Disponível em: <https://www.diabetes.org.br/publico/viva-saudavel-com-diabetes>. Acesso em 03 abr. 2020.
REIS, A. F.; VELHO, G. Bases genéticas do diabetes mellitus tipo 2, Arquivos Brasileiros de Endocrinologia & Metabologia, São Paulo, v. 46, n. 4, p.426-432, agosto, 2002.
RUIZ, L. V. B.; PRADO, R. P. Nefropatia diabética: diabetes melittus na nefropatia diabética. In: Anais da Semana Acadêmica, Científica e Cultural da FSP – 2017, Campus Itapetininga, São Paulo, Curso de Biomedicina, 2018. Disponível em: <http://unifsp.edu.br/itapetininga/wp-content/uploads/2018/08/Anais-da-Semana-Acad%C3%AAmica-Cient%C3%ADfica-e-Cultural-da-FSP-2018-Curso-de-Biomedicina.pdf>. Acesso em: 02 abr. 2020.
SIMONS, R.; STÜBEN, U.; MAHER, D. Insulin treated diabetic pilot applicants: recommendations. Brussels: ESAM, 2011. Disponível em: <http://www.esam.aero/images/docs/Position_Paper_Insulin_treated_diabetic_pilot_applicants.pdf>. Acesso em 1 maio 2020.
SOARES, A. H. Cetoacidose diabética é uma grave emergência médica. 2014. Disponível em: <https://www.diabetes.org.br/publico/ultimas/774-cetoacidose-diabetica-e-uma-grave-emergencia-medica>. Acesso em: 15 mar. 2020.
SOCIEDADE BRASILEIRA DE DIABETES. Tipos de diabetes. 2017. Disponível em: <https://www.diabetes.org.br/publico/diabetes-tipo-1/66-tudo-sobre-diabetes/581-tipos-de-diabetes>. Acesso em: 10 mar. 020.
. Tipos de diabetes, fatores de riscos. 2019. Disponível em: <https://www.diabetes.org.br/publico/diabetes/tipos-de-diabetes>. Acesso em: 11 mar. 2020.
SOCIEDADE BRASILEIRA DE ENDOCRINOLOGIA E METABOLOGIA. O que é diabetes? 2007. Disponível em: <https://www.endocrino.org.br/o-que-e-diabetes/>. Acesso em 14 mar. 2020.
. Diabetes mellitus gestacional, Revista da Associação Médica Brasileira, São Paulo, v. 54, n. 6, p´. 471-486, nov./dez., 2006. Disponível em: <https://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-42302008000600006>. Acesso em 14 mar. 2020
SOCIEDADE PORTUGUESA DIABETOLOGIA. Definição, diagnóstico e classificação do diabetes mellitus. 2020. Disponível em: <https://www.spd.pt/index.php/grupos-de-estudo-mainmenu-30/28-classificao-de-diabetes-mellitus/58-definio-diagnstico-e-classificao-da-diabetes-mellitus>. Acesso em: 25 mar. 2020.
THE GLOBAL DIABETES COMMUNITY. Pancreas and diabetes. 2019. Disponível em: <https://www.diabetes.co.uk/body/pancreas-and-diabetes.html>. Acesso em: 25 mar. 2020.
WORLD HEALTH ORGANIZATION. Classification of diabetes mellitus 2019. Geneva: WHO, 2019.
ZAJDENVERG, L. Diabetes gestacional. 2019. Disponível em: <https://www.diabetes.org.br/publico/diabetes-gestacional>. Acesso em 03 abr. 2020.
APPENDIX – FOOTNOTE REFERENCES
3. World Health Organization (WHO)
4. International Diabetes Federation (FID)
5. American Diabetes Association.
6. Global Diabetes Community.
7. Continuous Glucose Monitoring.
8. European Society of Aerospace Medicine.
[1] Degree in Aeronautical Sciences.
[2] Graduation in Visual Arts. Specialization in University Teaching.
Sent: June, 2020.
Approved: August, 2020.